Tuesday Poster Session
Category: Biliary/Pancreas
P4348 - Impact of Prior Bariatric Surgery on the Outcomes of Acute Pancreatitis in Obese Adults: A TriNetX Database Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Thai Hau Koo, MD
University of Sciences Malaysia Specialist Hospital
Kelantan, Kelantan, Malaysia
Presenting Author(s)
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Obese patients are at increased risk of developing severe acute pancreatitis (AP) with increased complication morbidities including pancreatic necrosis and intensive care unit admission. Bariatric surgery (BS) was reported to reduce mortality among AP patients in the US inpatient database. We aimed to evaluate whether the benefit from prior BS applies to a broader population.
Methods: We conducted a retrospective cohort study using de-identified TriNetX database, which includes data on over 179 million individuals globally, from January 1, 2015, to January 1, 2025. Adult patients (≥18 years) with a diagnosis of AP and BMI ≥ 40 kg/m² were divided into two cohorts based on the presence or absence of sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) history performed at least 6 months prior to AP diagnosis. Propensity score matching (1:1) was performed to adjust for demographics and confounders. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of the primary outcome (mortality) and secondary outcomes, including acute renal failure, respiratory failure, necrotizing pancreatitis, sepsis, septic shock, and need for surgical drainage of pancreatic fluid collections at 2 weeks, 1 month, and 3 months after AP diagnosis, based on the revised Atlanta classification.
Results: Among 2,798 patients with prior SG+RYGB and 47999 without, PSM yielded 2,792 matched pairs (Table 1). Patients with prior SG or RYGB were younger (mean age 51.1 ± 13 years vs. 53.3 ± 16.5 years, p< 0.001) and more likely to be female (75% vs. 59%, p< 0.001). After matching, patients with prior SG or RYGB had significantly lower odds of acute respiratory failure at 2 weeks (OR 0.581, p = 0.002) and 1 month (OR 0.623, p = 0.003, Table 2). No significant differences were observed in mortality, acute kidney failure, or necrotizing pancreatitis at all time points. The rates of sepsis, septic shock, and mortality tended to be lower in the SG or RYGB group without statistical significance.
Discussion: History of SG or RYGB decreased the risk of acute respiratory failure among obese patients within one month post-AP diagnosis based on this large cohort analysis. These findings suggest the history of SG or RYGB may serve as a protective factor against systemic complications of AP.
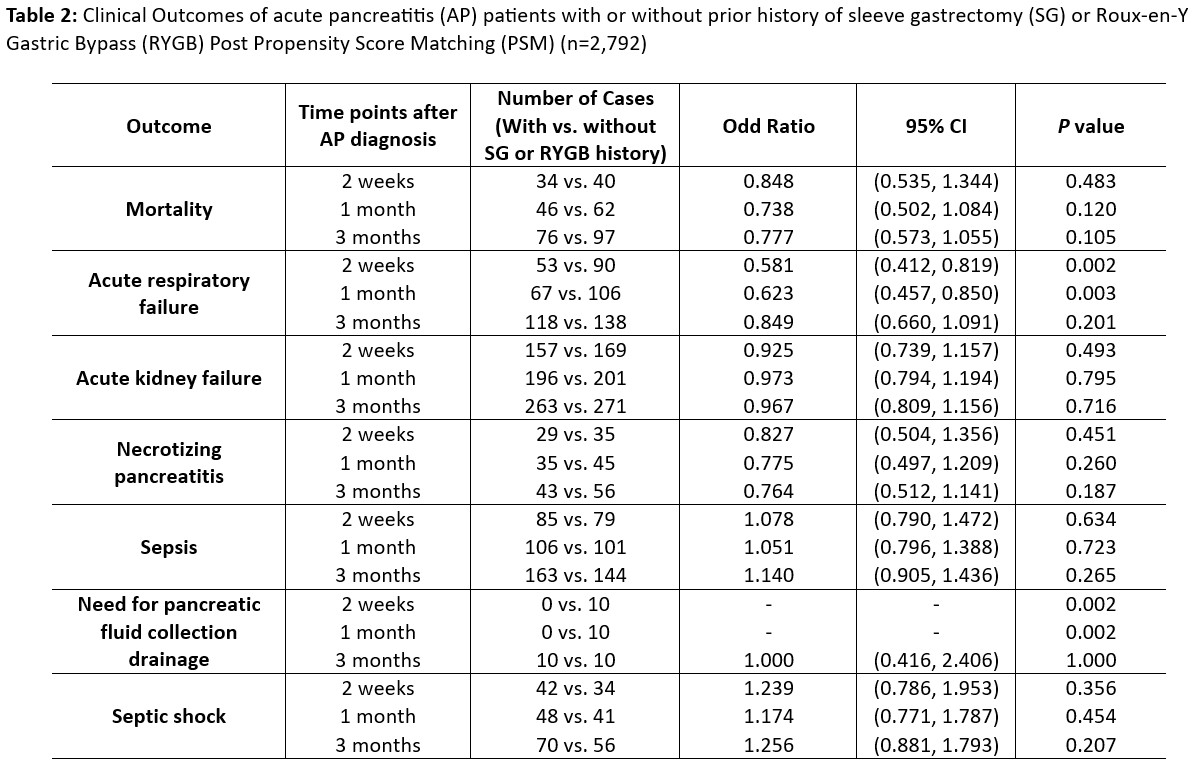
Figure: Table 1: Demographics and clinical variables of acute pancreatitis (AP) patients with or without history of sleeve gastrectomy (SG) or Roux-en-Y Gastric Bypass (RYGB)
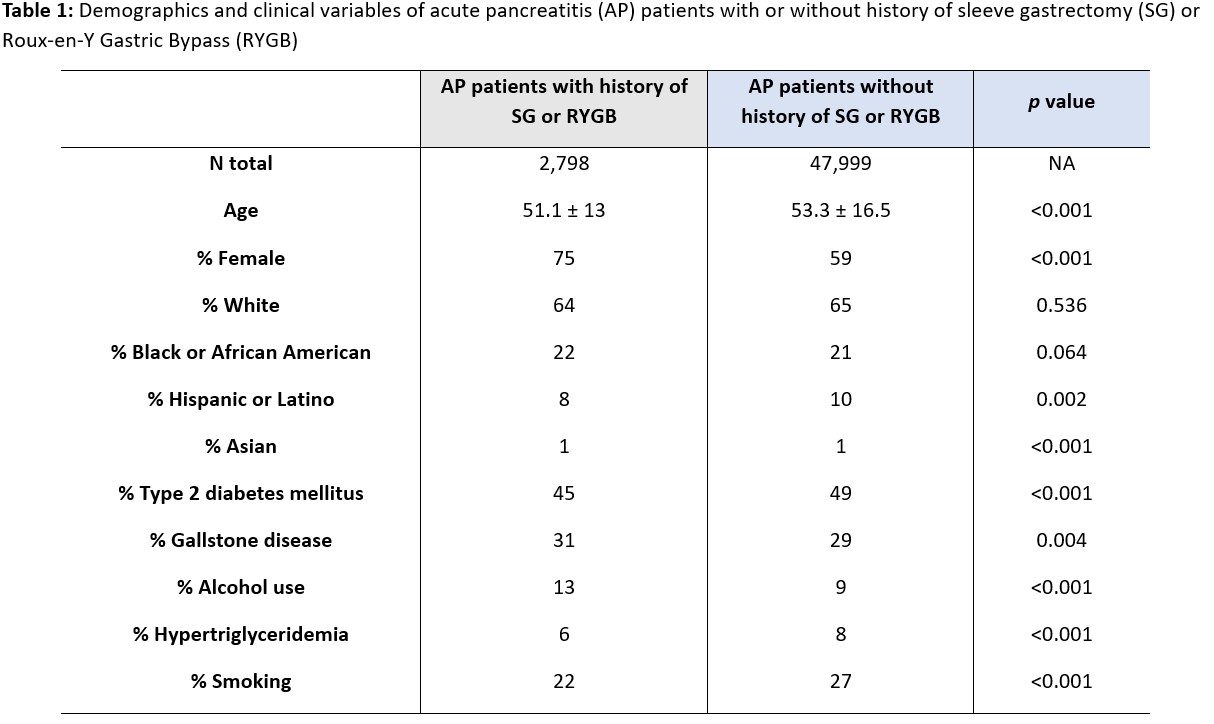
Figure: Table 2: Clinical Outcomes of acute pancreatitis (AP) patients with or without prior history of sleeve gastrectomy (SG) or Roux-en-Y Gastric Bypass (RYGB) Post Propensity Score Matching (PSM) (n=2,792)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P4348 - Impact of Prior Bariatric Surgery on the Outcomes of Acute Pancreatitis in Obese Adults: A TriNetX Database Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2University of Maryland Medical Center, Baltimore, MD; 3Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, OH
Introduction: Obese patients are at increased risk of developing severe acute pancreatitis (AP) with increased complication morbidities including pancreatic necrosis and intensive care unit admission. Bariatric surgery (BS) was reported to reduce mortality among AP patients in the US inpatient database. We aimed to evaluate whether the benefit from prior BS applies to a broader population.
Methods: We conducted a retrospective cohort study using de-identified TriNetX database, which includes data on over 179 million individuals globally, from January 1, 2015, to January 1, 2025. Adult patients (≥18 years) with a diagnosis of AP and BMI ≥ 40 kg/m² were divided into two cohorts based on the presence or absence of sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) history performed at least 6 months prior to AP diagnosis. Propensity score matching (1:1) was performed to adjust for demographics and confounders. Kaplan-Meier survival analysis and univariate Cox proportional hazards models were used to assess the incidence of the primary outcome (mortality) and secondary outcomes, including acute renal failure, respiratory failure, necrotizing pancreatitis, sepsis, septic shock, and need for surgical drainage of pancreatic fluid collections at 2 weeks, 1 month, and 3 months after AP diagnosis, based on the revised Atlanta classification.
Results: Among 2,798 patients with prior SG+RYGB and 47999 without, PSM yielded 2,792 matched pairs (Table 1). Patients with prior SG or RYGB were younger (mean age 51.1 ± 13 years vs. 53.3 ± 16.5 years, p< 0.001) and more likely to be female (75% vs. 59%, p< 0.001). After matching, patients with prior SG or RYGB had significantly lower odds of acute respiratory failure at 2 weeks (OR 0.581, p = 0.002) and 1 month (OR 0.623, p = 0.003, Table 2). No significant differences were observed in mortality, acute kidney failure, or necrotizing pancreatitis at all time points. The rates of sepsis, septic shock, and mortality tended to be lower in the SG or RYGB group without statistical significance.
Discussion: History of SG or RYGB decreased the risk of acute respiratory failure among obese patients within one month post-AP diagnosis based on this large cohort analysis. These findings suggest the history of SG or RYGB may serve as a protective factor against systemic complications of AP.
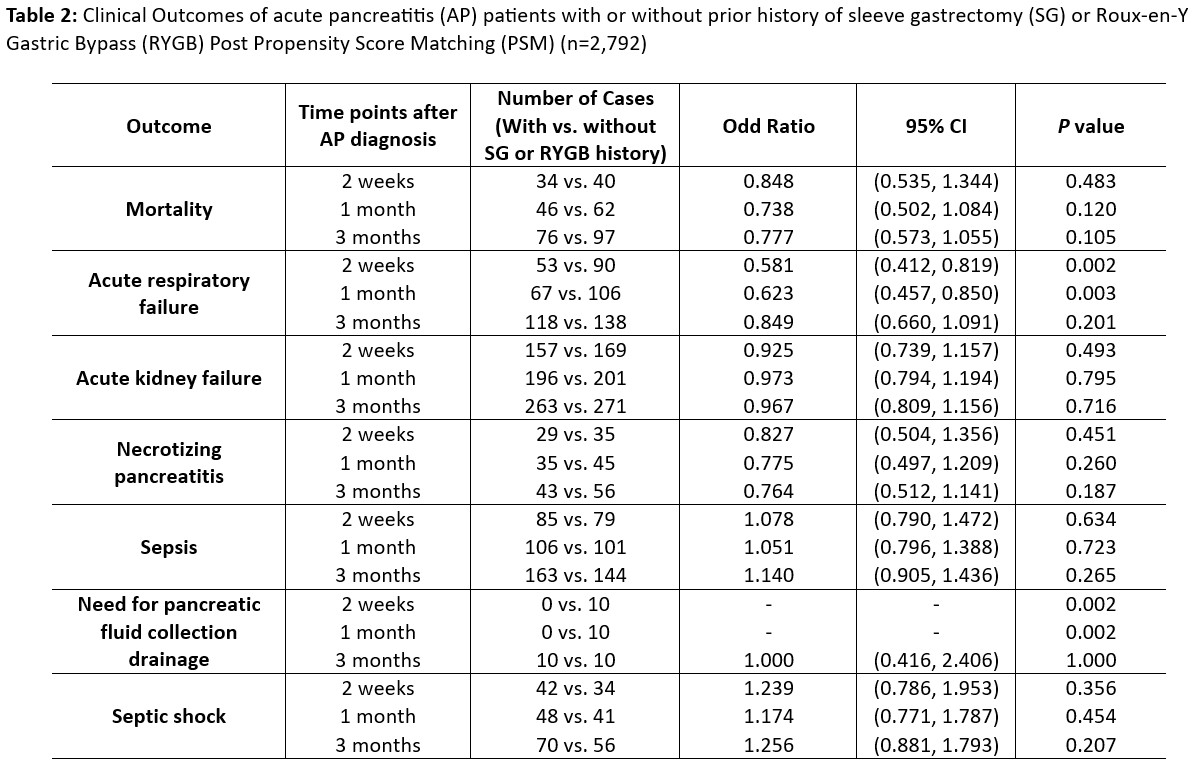
Figure: Table 1: Demographics and clinical variables of acute pancreatitis (AP) patients with or without history of sleeve gastrectomy (SG) or Roux-en-Y Gastric Bypass (RYGB)
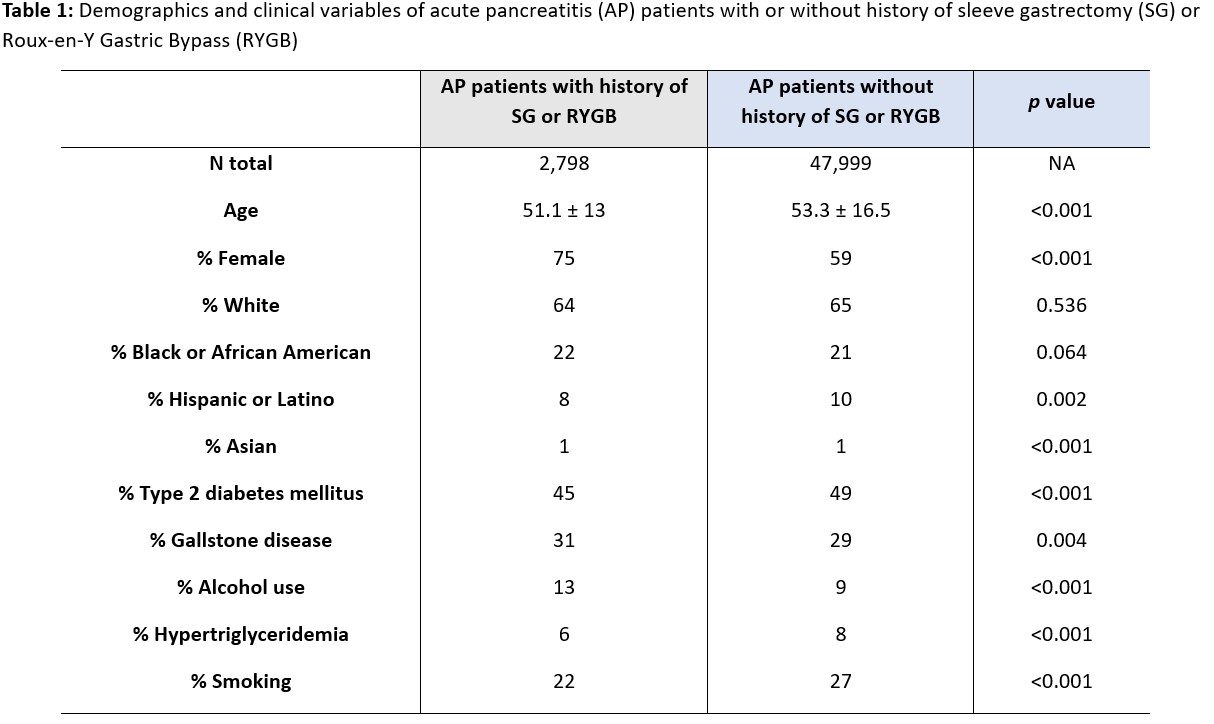
Figure: Table 2: Clinical Outcomes of acute pancreatitis (AP) patients with or without prior history of sleeve gastrectomy (SG) or Roux-en-Y Gastric Bypass (RYGB) Post Propensity Score Matching (PSM) (n=2,792)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Yilin Song indicated no relevant financial relationships.
Stephen Firkins indicated no relevant financial relationships.
Roberto Simons-Linares indicated no relevant financial relationships.
Thai Hau Koo, MD1, Yilin Song, MD2, Stephen Firkins, MD3, Roberto Simons-Linares, MD3. P4348 - Impact of Prior Bariatric Surgery on the Outcomes of Acute Pancreatitis in Obese Adults: A TriNetX Database Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
