Tuesday Poster Session
Category: Biliary/Pancreas
P4347 - Comparative Risk of Cholangiocarcinoma With GLP-1 Receptor Agonists and Bariatric Surgery in Patients With Diabetes and Obesity: A Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yahya Alhalalmeh, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohamed Eldesouki, MD4, Basile Njei, MD, PhD, MPH5
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 3New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5VA Connecticut Healthcare System and Yale University, West Haven, CT
Introduction: Cholangiocarcinoma (CCA) is a rare but aggressive bile duct cancer with rising global incidence. Type 2 diabetes mellitus (T2DM) and obesity are independent risk factors for CCA. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and bariatric surgery are commonly used for glycemic and weight control in this population. While GLP-1 RAs offer clear metabolic benefits, prior studies have reported variable associations with gastrointestinal malignancies, including CCA. This study compares CCA risk in patients treated with GLP-1 RAs versus those who underwent bariatric surgery.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify adults (age ≥18) with T2DM and BMI >30 who initiated GLP-1 RA therapy or underwent bariatric surgery. A secondary analysis included patients with BMI >35, regardless of diabetes status. Patients with a prior history of CCA were excluded. Propensity score matching was applied in a 1:1 ratio to balance GLP-1 RA users and bariatric surgery patients on key characteristics (Figure 1). We adjusted for CCA risk factors and other diabetes- or obesity-related medications. The primary outcome was CCA incidence post-intervention. Risk was further stratified by age and sex. Adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs) were estimated via Cox proportional hazards models.
Results: A total of 94,452 patients who initiated GLP-1 RA therapy and 23,515 who underwent bariatric surgery were identified. After propensity score matching, 19,851 patients remained in each group. In the cohort with T2DM and BMI >30, GLP-1 RAs showed significantly lower risk of CCA compared to bariatric surgery (aHR = 0.45, 95% CI: 0.28–0.73; p = 0.01). Subgroup analysis showed this association was significant in females (aHR = 0.37, 95% CI: 0.17–0.77; p = 0.01) and in patients over age 45 (aHR = 0.49, 95% CI: 0.30–0.80; p = 0.01), but not in males (aHR = 0.59, 95% CI: 0.29–1.18; p = 0.13). Among those with BMI >35, GLP-1 RAs were also associated with a lower risk of CCA (aHR = 0.59, 95% CI: 0.35–0.99; p = 0.04), as shown in Figure 2.
Discussion: In this large real-world cohort, GLP-1 receptor agonists were associated with a significantly lower risk of CCA compared to bariatric surgery among patients with obesity and T2DM. These findings highlight a potential association between GLP-1 RA use and lower CCA risk, warranting further prospective studies to confirm causality and explore underlying biological mechanisms.
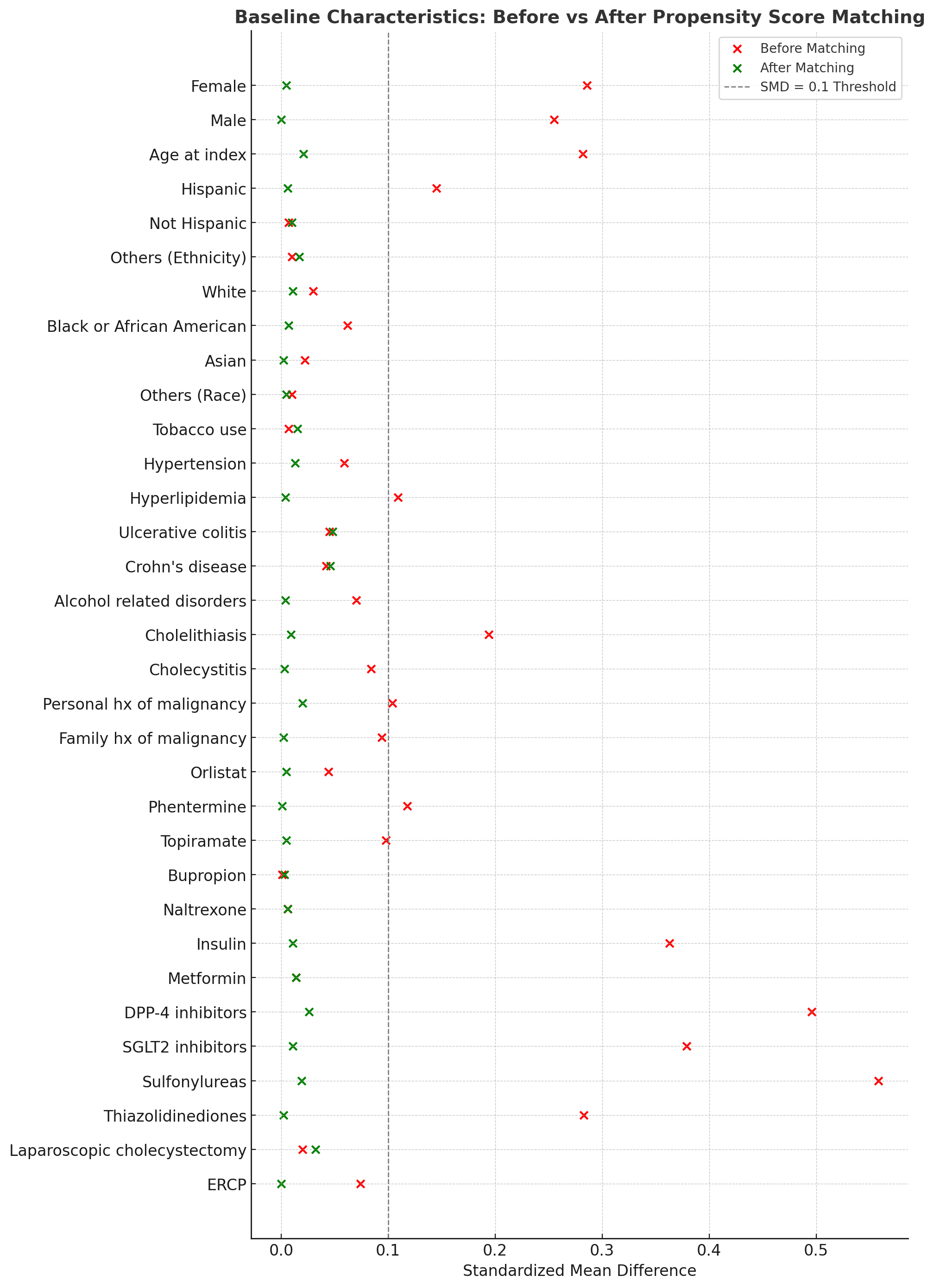
Figure: Figure 1
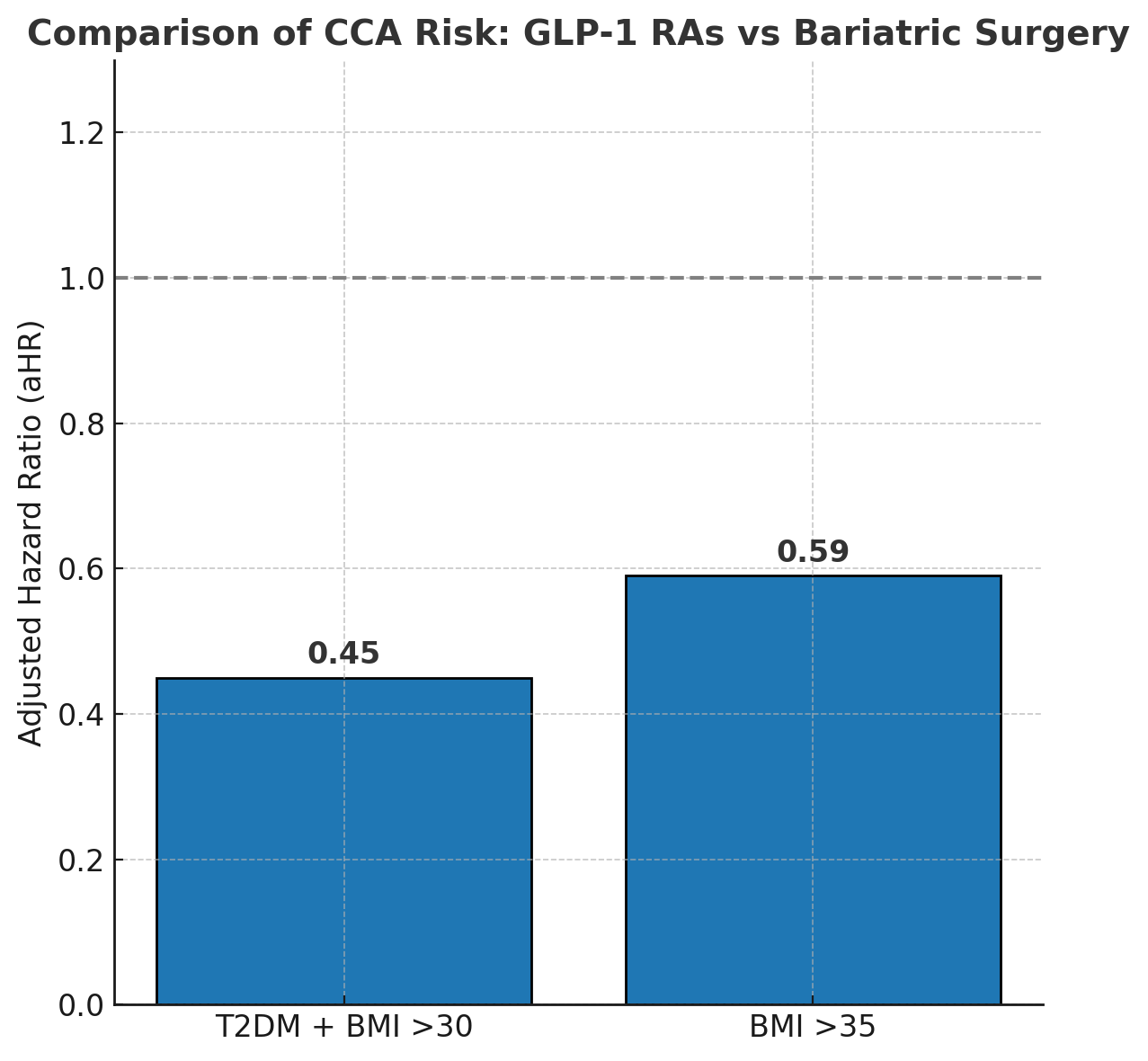
Figure: Figure 2
Disclosures:
Yahya Alhalalmeh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Ismail Althunibat indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohamed Eldesouki, MD4, Basile Njei, MD, PhD, MPH5. P4347 - Comparative Risk of Cholangiocarcinoma With GLP-1 Receptor Agonists and Bariatric Surgery in Patients With Diabetes and Obesity: A Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 3New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ; 5VA Connecticut Healthcare System and Yale University, West Haven, CT
Introduction: Cholangiocarcinoma (CCA) is a rare but aggressive bile duct cancer with rising global incidence. Type 2 diabetes mellitus (T2DM) and obesity are independent risk factors for CCA. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and bariatric surgery are commonly used for glycemic and weight control in this population. While GLP-1 RAs offer clear metabolic benefits, prior studies have reported variable associations with gastrointestinal malignancies, including CCA. This study compares CCA risk in patients treated with GLP-1 RAs versus those who underwent bariatric surgery.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify adults (age ≥18) with T2DM and BMI >30 who initiated GLP-1 RA therapy or underwent bariatric surgery. A secondary analysis included patients with BMI >35, regardless of diabetes status. Patients with a prior history of CCA were excluded. Propensity score matching was applied in a 1:1 ratio to balance GLP-1 RA users and bariatric surgery patients on key characteristics (Figure 1). We adjusted for CCA risk factors and other diabetes- or obesity-related medications. The primary outcome was CCA incidence post-intervention. Risk was further stratified by age and sex. Adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs) were estimated via Cox proportional hazards models.
Results: A total of 94,452 patients who initiated GLP-1 RA therapy and 23,515 who underwent bariatric surgery were identified. After propensity score matching, 19,851 patients remained in each group. In the cohort with T2DM and BMI >30, GLP-1 RAs showed significantly lower risk of CCA compared to bariatric surgery (aHR = 0.45, 95% CI: 0.28–0.73; p = 0.01). Subgroup analysis showed this association was significant in females (aHR = 0.37, 95% CI: 0.17–0.77; p = 0.01) and in patients over age 45 (aHR = 0.49, 95% CI: 0.30–0.80; p = 0.01), but not in males (aHR = 0.59, 95% CI: 0.29–1.18; p = 0.13). Among those with BMI >35, GLP-1 RAs were also associated with a lower risk of CCA (aHR = 0.59, 95% CI: 0.35–0.99; p = 0.04), as shown in Figure 2.
Discussion: In this large real-world cohort, GLP-1 receptor agonists were associated with a significantly lower risk of CCA compared to bariatric surgery among patients with obesity and T2DM. These findings highlight a potential association between GLP-1 RA use and lower CCA risk, warranting further prospective studies to confirm causality and explore underlying biological mechanisms.
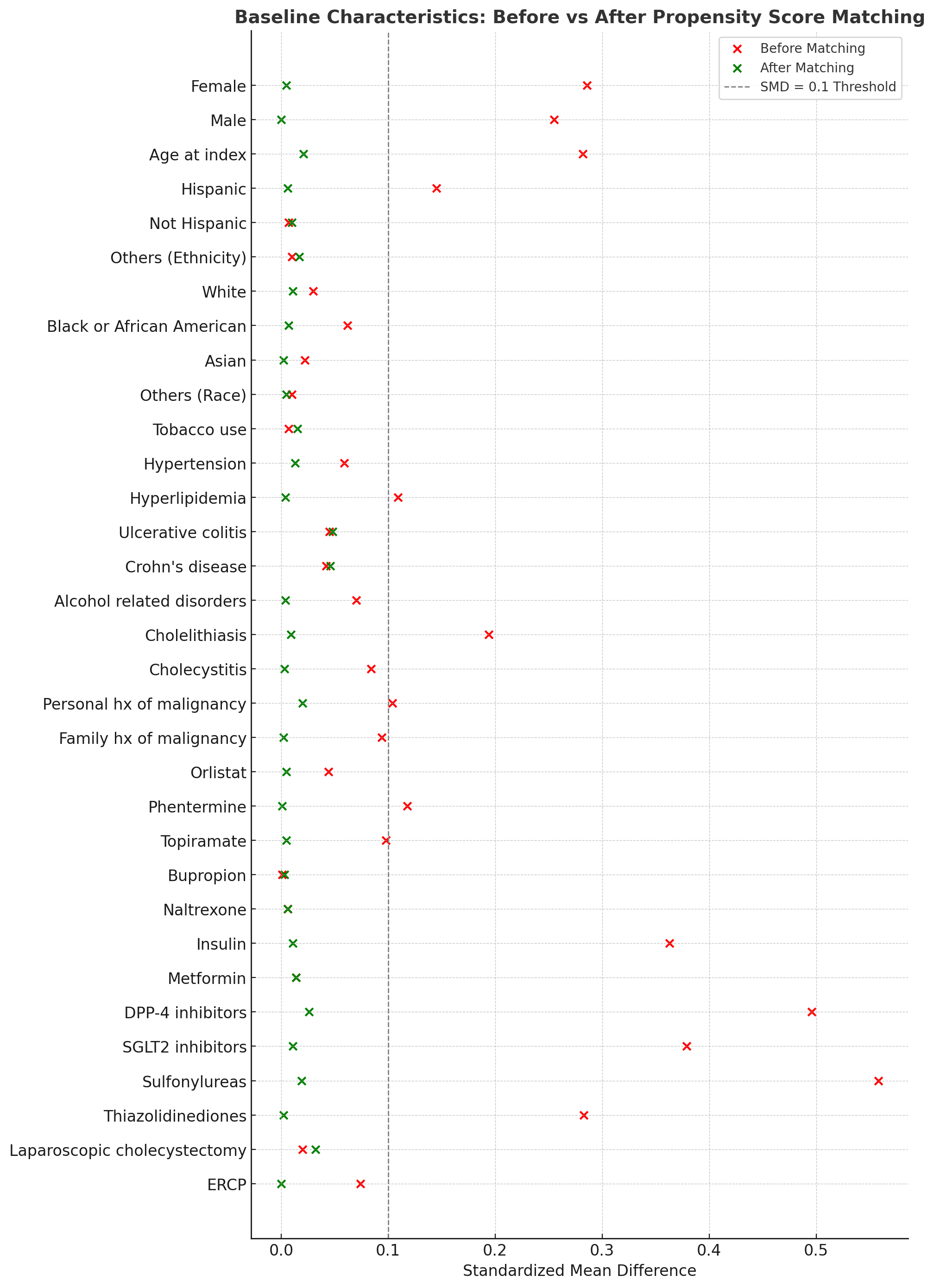
Figure: Figure 1
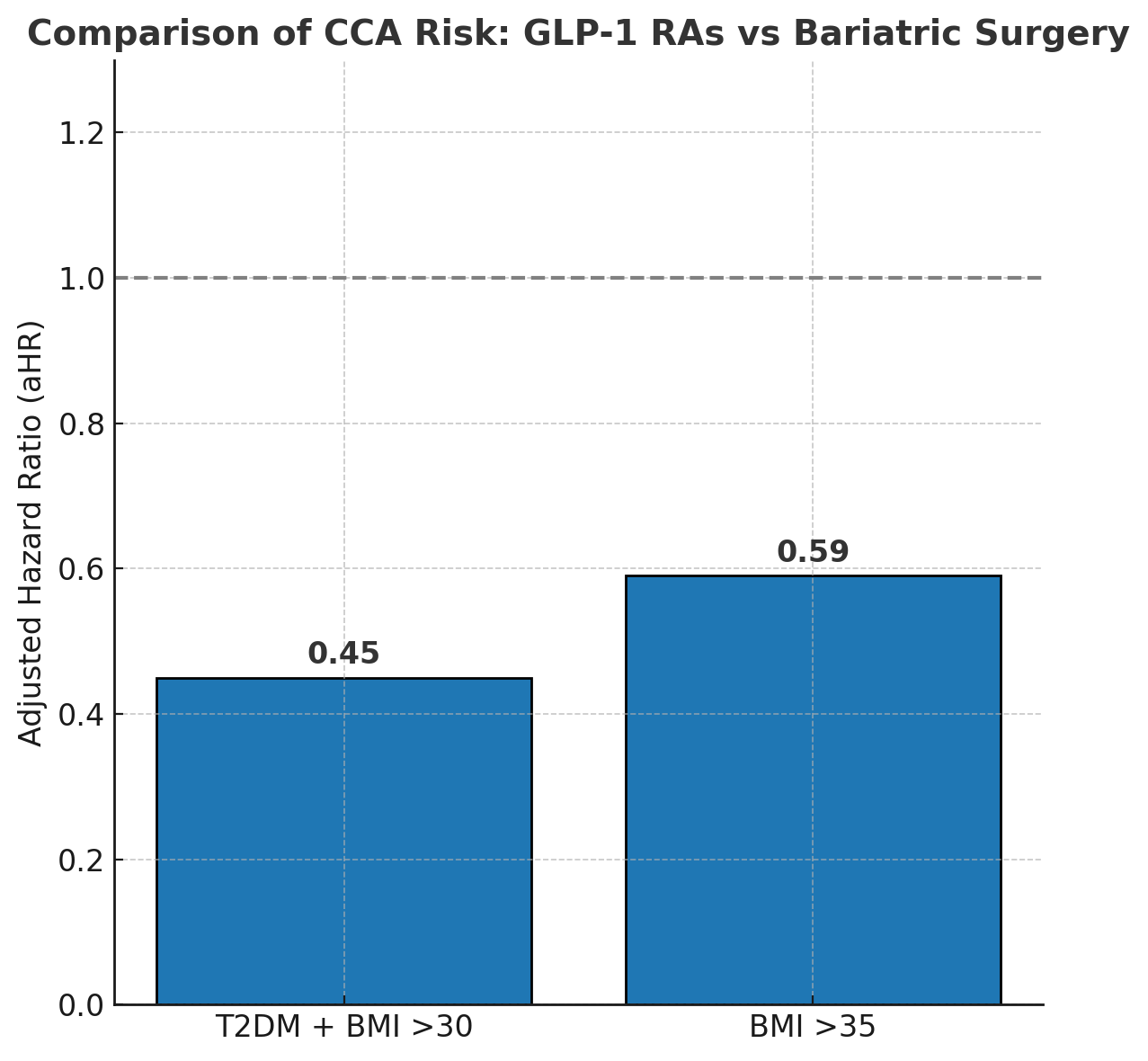
Figure: Figure 2
Disclosures:
Yahya Alhalalmeh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Ismail Althunibat indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohamed Eldesouki, MD4, Basile Njei, MD, PhD, MPH5. P4347 - Comparative Risk of Cholangiocarcinoma With GLP-1 Receptor Agonists and Bariatric Surgery in Patients With Diabetes and Obesity: A Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
