Tuesday Poster Session
Category: Biliary/Pancreas
P4430 - When the Flow Stops: Functional Biliary Obstruction Secondary to Chronic Opioid Use
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taiwo Ajani, MD (he/him/his)
University of Texas Rio Grande Valley
McAllen, TX
Presenting Author(s)
Taiwo Ajani, MD1, Jose Loayza Pintado, MD1, Jorge Aboytes Trevino, MD1, Ivan Mogollon, MD2, Calderon Aura, MD1, Ismael Cantú, MD2
1University of Texas Rio Grande Valley, McAllen, TX; 2University of Texas Rio Grande Valley, Edinburg, TX
Introduction: Sphincter of Oddi dysfunction (SOD) is a functional biliary disorder that can mimic obstructive pathology despite the absence of anatomical abnormalities. While often associated with post-cholecystectomy states, SOD may also be induced by chronic opioid use. Diagnosing opioid-related SOD remains difficult due to nonspecific symptoms and limitations of routine imaging.
Case Description/
Methods: A 55-year-old woman with epilepsy, type 2 diabetes, and recurrent pancreatitis presented with a year-long history of colicky upper abdominal pain, worsened by fatty foods and accompanied by nausea and vomiting. Vital signs and most lab values were unremarkable except for a mildly elevated alkaline phosphatase. Imaging (ultrasound, CT, MRCP, and EUS) showed dilated bile and pancreatic ducts without definitive obstruction. A urine drug screen was positive for opioids, and the patient admitted to long-term use. Based on her symptoms, intermittent liver enzyme elevation, and the absence of structural lesions, she was diagnosed with Milwaukee Type II opioid-induced SOD. Treatment included low-dose amitriptyline and lifestyle modifications.
Discussion: Opioids can elevate sphincter of Oddi tone via μ-opioid receptor activation, leading to functional outflow obstruction. This mechanism, though documented physiologically, is often underrecognized in clinical practice. In patients with chronic opioid use and biliary-type pain without visible obstruction, SOD should be considered. In this case, conservative management with a tricyclic antidepressant, not contraindicated in seizure disorders, alongside dietary and behavioral recommendations, provided a safer alternative to invasive intervention. Early recognition of opioid-induced SOD can help avoid unnecessary procedures and guide effective symptom control.
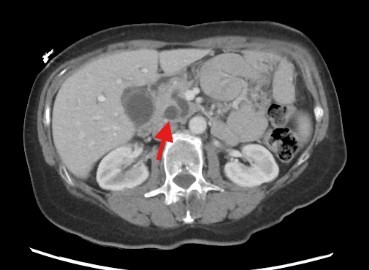
Figure: Image 1: Computed Tomography (CT) of the Abdomen
Moderate biliary tree dilation without evidence of calcified choledocholithiasis, along with accompanying dilation of the pancreatic duct.
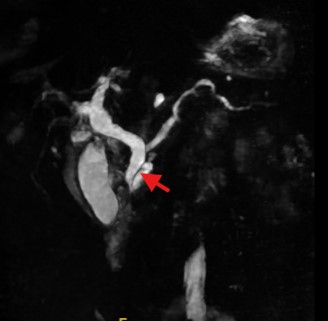
Figure: Image 2: Magnetic resonance cholangiopancreatography (MRCP)
Progressive dilation of both intrahepatic and extrahepatic bile ducts, along with prominence of the pancreatic duct, most notably in the region of the pancreatic head. No evidence of obstructing calculi or mass lesion is observed.
Disclosures:
Taiwo Ajani indicated no relevant financial relationships.
Jose Loayza Pintado indicated no relevant financial relationships.
Jorge Aboytes Trevino indicated no relevant financial relationships.
Ivan Mogollon indicated no relevant financial relationships.
Calderon Aura indicated no relevant financial relationships.
Ismael Cantú indicated no relevant financial relationships.
Taiwo Ajani, MD1, Jose Loayza Pintado, MD1, Jorge Aboytes Trevino, MD1, Ivan Mogollon, MD2, Calderon Aura, MD1, Ismael Cantú, MD2. P4430 - When the Flow Stops: Functional Biliary Obstruction Secondary to Chronic Opioid Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Rio Grande Valley, McAllen, TX; 2University of Texas Rio Grande Valley, Edinburg, TX
Introduction: Sphincter of Oddi dysfunction (SOD) is a functional biliary disorder that can mimic obstructive pathology despite the absence of anatomical abnormalities. While often associated with post-cholecystectomy states, SOD may also be induced by chronic opioid use. Diagnosing opioid-related SOD remains difficult due to nonspecific symptoms and limitations of routine imaging.
Case Description/
Methods: A 55-year-old woman with epilepsy, type 2 diabetes, and recurrent pancreatitis presented with a year-long history of colicky upper abdominal pain, worsened by fatty foods and accompanied by nausea and vomiting. Vital signs and most lab values were unremarkable except for a mildly elevated alkaline phosphatase. Imaging (ultrasound, CT, MRCP, and EUS) showed dilated bile and pancreatic ducts without definitive obstruction. A urine drug screen was positive for opioids, and the patient admitted to long-term use. Based on her symptoms, intermittent liver enzyme elevation, and the absence of structural lesions, she was diagnosed with Milwaukee Type II opioid-induced SOD. Treatment included low-dose amitriptyline and lifestyle modifications.
Discussion: Opioids can elevate sphincter of Oddi tone via μ-opioid receptor activation, leading to functional outflow obstruction. This mechanism, though documented physiologically, is often underrecognized in clinical practice. In patients with chronic opioid use and biliary-type pain without visible obstruction, SOD should be considered. In this case, conservative management with a tricyclic antidepressant, not contraindicated in seizure disorders, alongside dietary and behavioral recommendations, provided a safer alternative to invasive intervention. Early recognition of opioid-induced SOD can help avoid unnecessary procedures and guide effective symptom control.
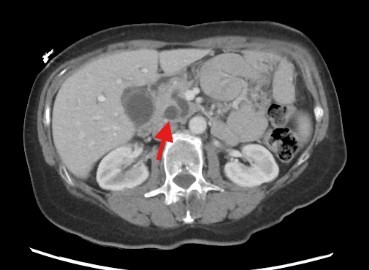
Figure: Image 1: Computed Tomography (CT) of the Abdomen
Moderate biliary tree dilation without evidence of calcified choledocholithiasis, along with accompanying dilation of the pancreatic duct.
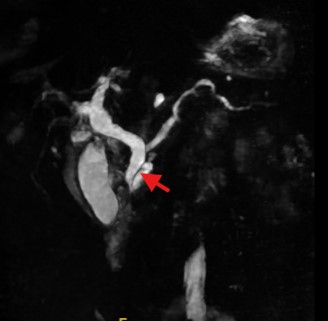
Figure: Image 2: Magnetic resonance cholangiopancreatography (MRCP)
Progressive dilation of both intrahepatic and extrahepatic bile ducts, along with prominence of the pancreatic duct, most notably in the region of the pancreatic head. No evidence of obstructing calculi or mass lesion is observed.
Disclosures:
Taiwo Ajani indicated no relevant financial relationships.
Jose Loayza Pintado indicated no relevant financial relationships.
Jorge Aboytes Trevino indicated no relevant financial relationships.
Ivan Mogollon indicated no relevant financial relationships.
Calderon Aura indicated no relevant financial relationships.
Ismael Cantú indicated no relevant financial relationships.
Taiwo Ajani, MD1, Jose Loayza Pintado, MD1, Jorge Aboytes Trevino, MD1, Ivan Mogollon, MD2, Calderon Aura, MD1, Ismael Cantú, MD2. P4430 - When the Flow Stops: Functional Biliary Obstruction Secondary to Chronic Opioid Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
