Tuesday Poster Session
Category: Biliary/Pancreas
P4423 - Chronicles of Veterans with Pancreatic Neuroendocrine Tumors
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Christine Son, MD (she/her/hers)
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Paul Roach, MD2
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL; 3Loyola University Chicago Stritch School of Medicine, Maywood, IL
Introduction: Pancreatic neuroendocrine tumors (pNETs) are rare type of pancreatic cancer, comprising less than 2% of all pancreatic malignancies. Pancreatic NETs make up about 7% of all GI NETs. Pancreatic NETs are identified as either functional, producing hormones and subsequently clinical symptoms, or non-functional. Surgical resection is the only curative therapeutic option for localized pNETs. However, combination of systemic and local therapies with somatostatin analogs and targeted therapies with everolimus and sunitinib for advanced pNETs have shown significant improvement in prognosis in the recent years. There are no studies dedicated to pNETs among Veterans. This case series presents 20 cases of pancreatic NETs in Veterans and review of the treatment course and management, highlighting the prognostic and predictive factors on overall survival and outcomes.
Case Description/
Methods: A total of 20 cases of pancreatic NETs were identified from Edward Hines Jr VA Hospital Cancer Registry from 2019–2024. We conducted a retrospective analysis of these cases focusing on survival, disease management, and outcomes compared with current literature.
Pancreas was the most common organ site of NETs at our institution, constituting 32.8% all GI NETs over the 5-year period (2019-2024). All 20 pNETs were non-functioning with no clinical symptoms from hormone production. Of 20 cases of pancreatic NETs reviewed, 55% (11 out of 20) had well differentiated, grade 1 disease with no metastases at the time of presentation. These patients had good clinical outcomes with continued surveillance. Patients with high-grade, metastatic disease at the time of presentation all passed within 1 year of presentation.
Discussion: Higher prevalence of pancreatic NET was seen at our institution (32.8%) compared to 7% pNETs reported in literature. Grade 1 was the most common grade, as is currently known in publications. Most patients with low grade, localized disease had good clinical outcomes with surgical resection and continued surveillance with imaging up to 10 years after the time of initial presentation. This was consistent with literature finding that tumor grade may be the most important prognostic factor. For 6 of the pNETs who passed, veterans with higher stage at presentation passed from metastatic pNETs while patients with lower stage passed from cardiac complications (Table 1). This warrants further investigation of factors associated with high prevalence of pNETs in Veteran populations.
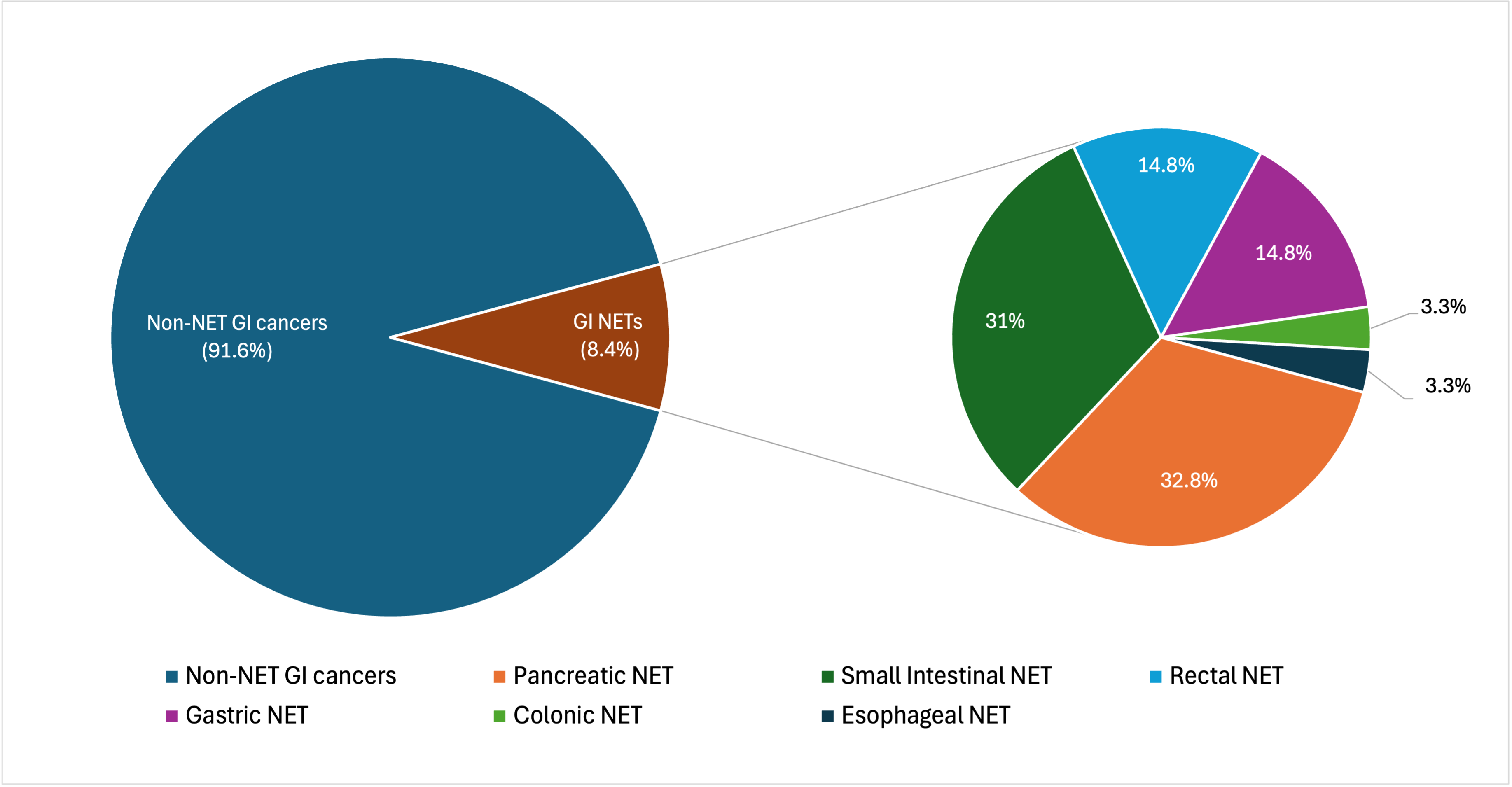
Figure: Figure 1. Distribution of GI Tumors 2019 - 2024.
From 2019 to 2024, a total of 723 GI system cancers were identified. Of these 723 cancers, 61 (8.4%) were neuroendocrine tumors. The NETs comprised 20 pancreatic (32.8%), 19 small intestinal (31%), 9 rectal (14.8%), 9 gastric (14.8%), 2 colon (3.3%), and 2 esophageal NET (3.3%) cases.
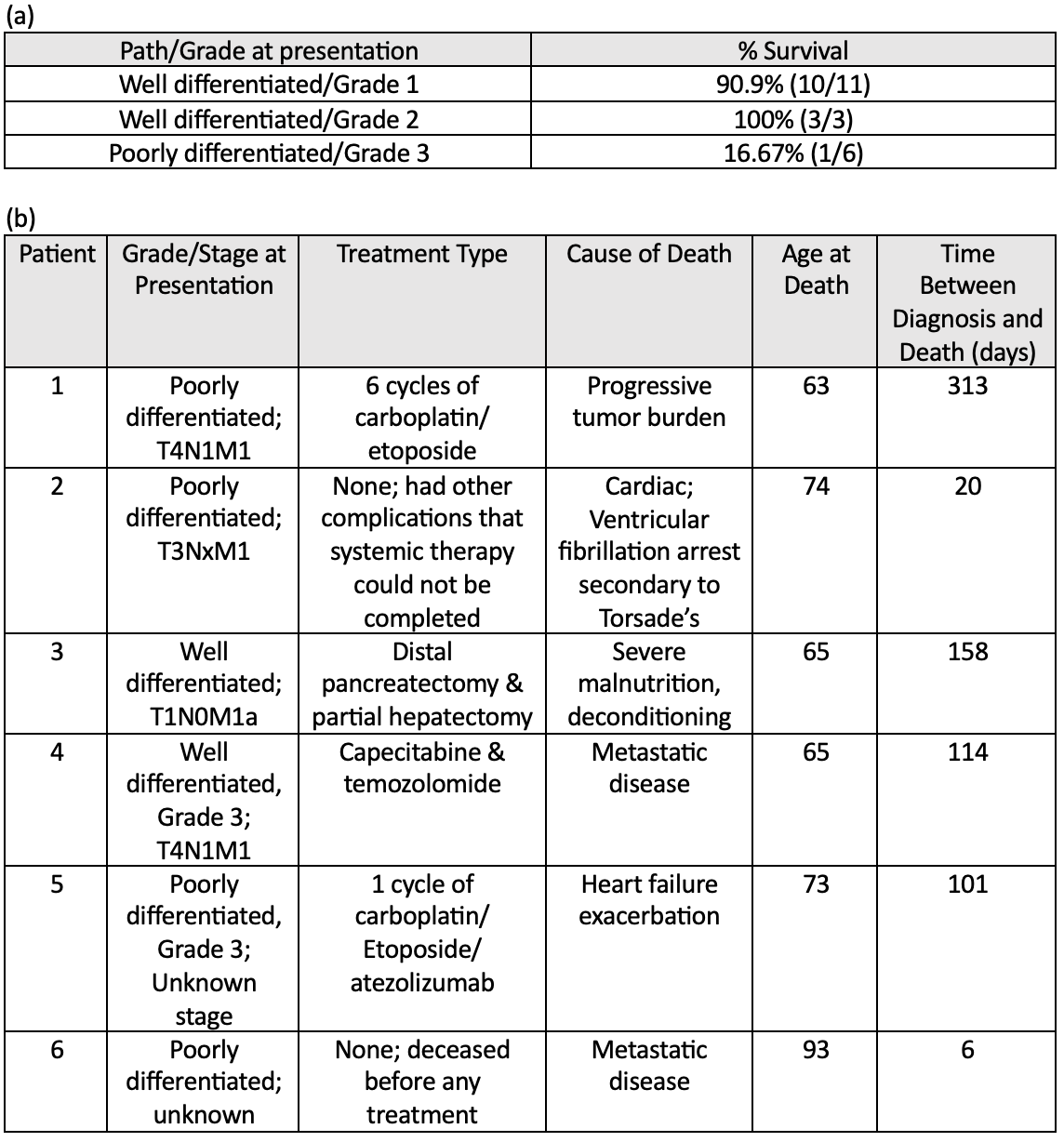
Figure: (a) Survival data by pathology/grade at presentation
(b) Mortality data for six patients
Disclosures:
Christine Son indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Joshua Kalapala indicated no relevant financial relationships.
Paul Roach indicated no relevant financial relationships.
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Paul Roach, MD2. P4423 - Chronicles of Veterans with Pancreatic Neuroendocrine Tumors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Paul Roach, MD2
1Loyola University Medical Center, Maywood, IL; 2Edward Hines Jr. Veterans Affairs Hospital, Hines, IL; 3Loyola University Chicago Stritch School of Medicine, Maywood, IL
Introduction: Pancreatic neuroendocrine tumors (pNETs) are rare type of pancreatic cancer, comprising less than 2% of all pancreatic malignancies. Pancreatic NETs make up about 7% of all GI NETs. Pancreatic NETs are identified as either functional, producing hormones and subsequently clinical symptoms, or non-functional. Surgical resection is the only curative therapeutic option for localized pNETs. However, combination of systemic and local therapies with somatostatin analogs and targeted therapies with everolimus and sunitinib for advanced pNETs have shown significant improvement in prognosis in the recent years. There are no studies dedicated to pNETs among Veterans. This case series presents 20 cases of pancreatic NETs in Veterans and review of the treatment course and management, highlighting the prognostic and predictive factors on overall survival and outcomes.
Case Description/
Methods: A total of 20 cases of pancreatic NETs were identified from Edward Hines Jr VA Hospital Cancer Registry from 2019–2024. We conducted a retrospective analysis of these cases focusing on survival, disease management, and outcomes compared with current literature.
Pancreas was the most common organ site of NETs at our institution, constituting 32.8% all GI NETs over the 5-year period (2019-2024). All 20 pNETs were non-functioning with no clinical symptoms from hormone production. Of 20 cases of pancreatic NETs reviewed, 55% (11 out of 20) had well differentiated, grade 1 disease with no metastases at the time of presentation. These patients had good clinical outcomes with continued surveillance. Patients with high-grade, metastatic disease at the time of presentation all passed within 1 year of presentation.
Discussion: Higher prevalence of pancreatic NET was seen at our institution (32.8%) compared to 7% pNETs reported in literature. Grade 1 was the most common grade, as is currently known in publications. Most patients with low grade, localized disease had good clinical outcomes with surgical resection and continued surveillance with imaging up to 10 years after the time of initial presentation. This was consistent with literature finding that tumor grade may be the most important prognostic factor. For 6 of the pNETs who passed, veterans with higher stage at presentation passed from metastatic pNETs while patients with lower stage passed from cardiac complications (Table 1). This warrants further investigation of factors associated with high prevalence of pNETs in Veteran populations.
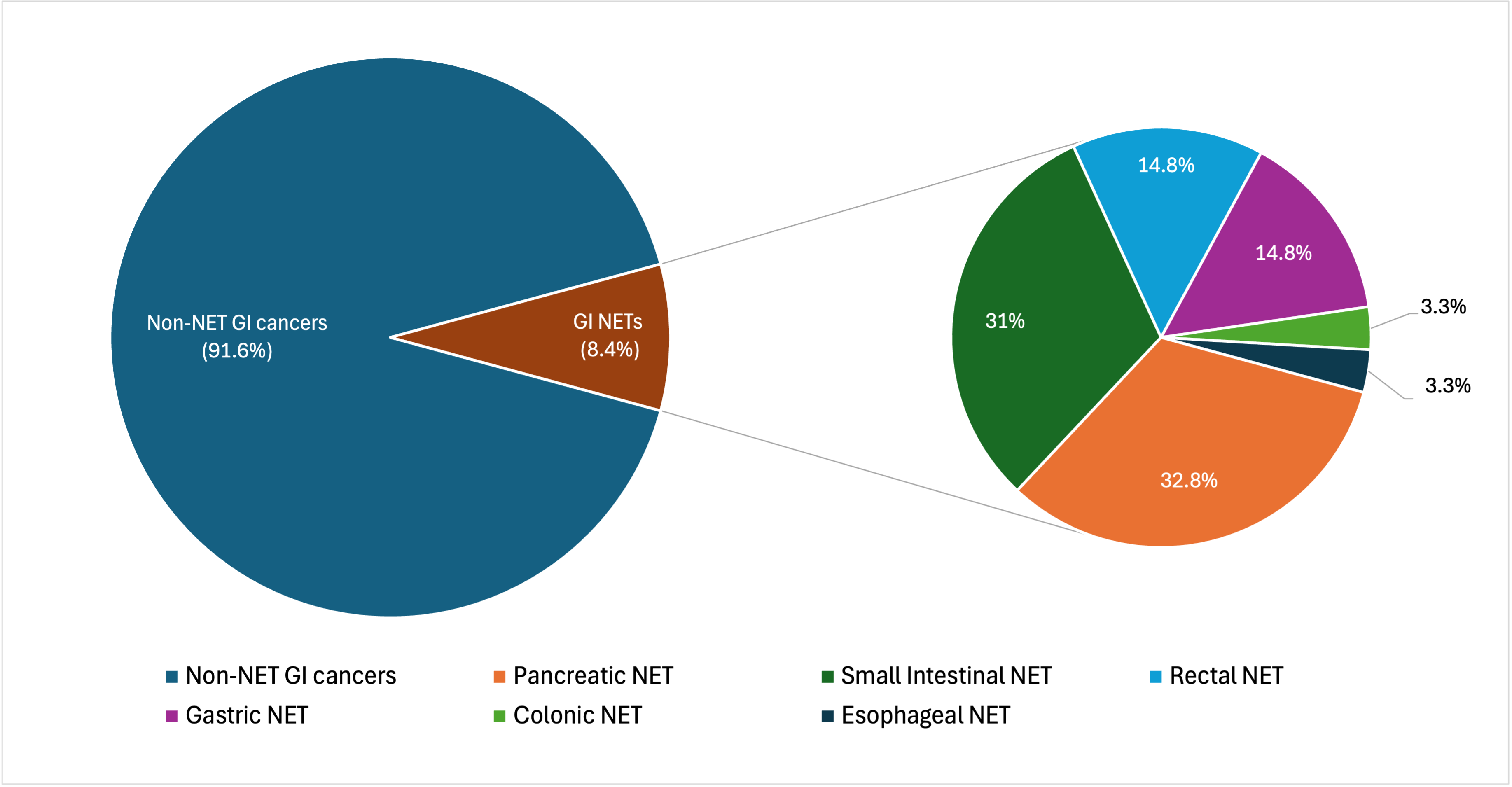
Figure: Figure 1. Distribution of GI Tumors 2019 - 2024.
From 2019 to 2024, a total of 723 GI system cancers were identified. Of these 723 cancers, 61 (8.4%) were neuroendocrine tumors. The NETs comprised 20 pancreatic (32.8%), 19 small intestinal (31%), 9 rectal (14.8%), 9 gastric (14.8%), 2 colon (3.3%), and 2 esophageal NET (3.3%) cases.
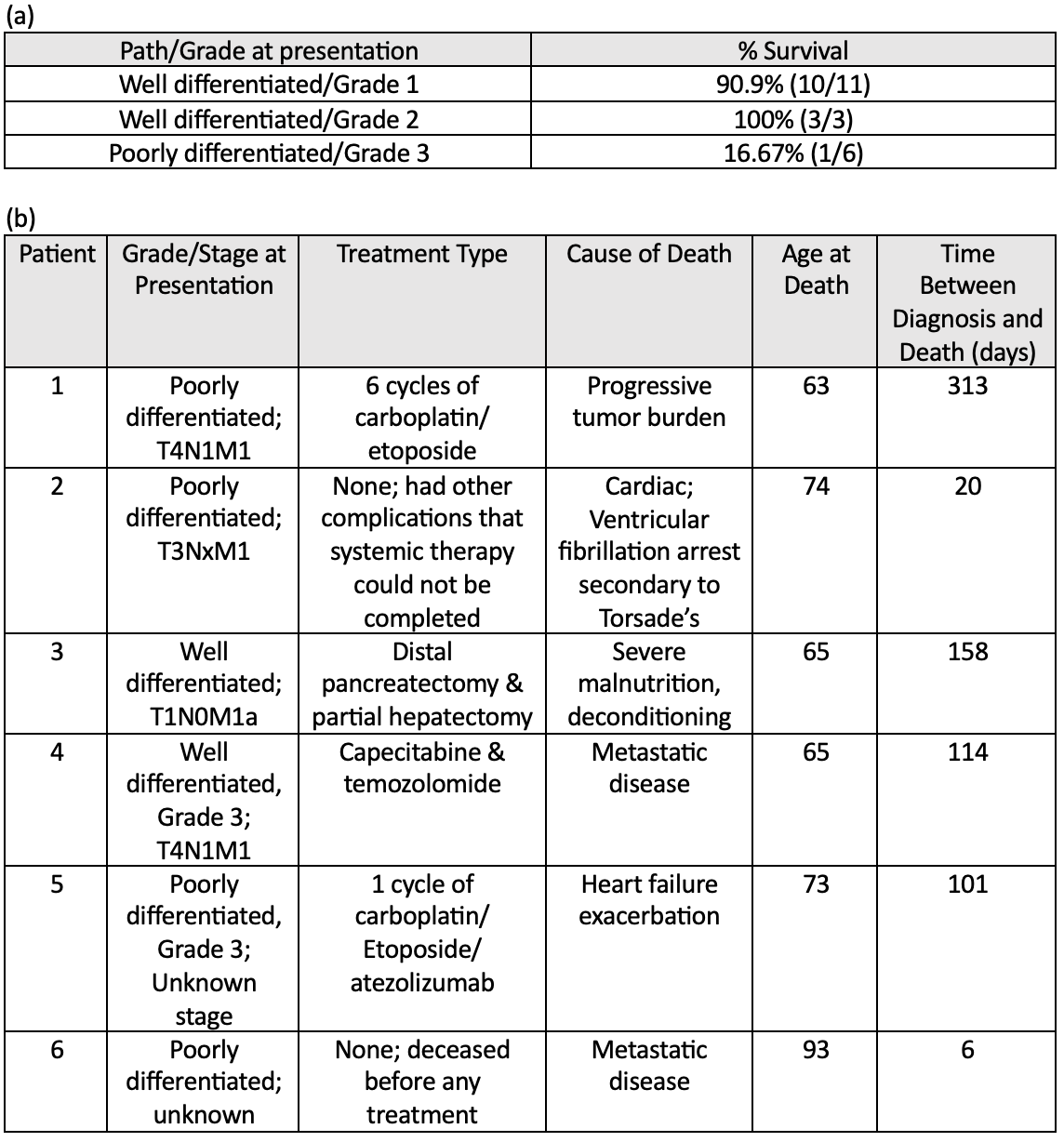
Figure: (a) Survival data by pathology/grade at presentation
(b) Mortality data for six patients
Disclosures:
Christine Son indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Joshua Kalapala indicated no relevant financial relationships.
Paul Roach indicated no relevant financial relationships.
Christine Son, MD1, Promila Banerjee, MD, FACG2, Joshua Kalapala, MD3, Paul Roach, MD2. P4423 - Chronicles of Veterans with Pancreatic Neuroendocrine Tumors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


