Tuesday Poster Session
Category: Biliary/Pancreas
P4421 - Duodenal Fistulization of Main Duct IPMN: A Rare Indicator of Invasive Transformation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amirali Tavangar, MD
University of California Irvine Digestive Health Institute
Orange, CA
Presenting Author(s)
Award: ACG Presidential Poster Award
Amirali Tavangar, MD1, Peter Nguyen, MD2, Frances Dang, MD, MSc3, Suhail Sidhu, MD2, Bryant Le, MD2, Momin Masroor, MD2, Jason Samarasena, MD, MBA, FACG2, Christopher Paiji, MD1
1University of California Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine, Orange, CA; 3University of California Irvine, Irvine, CA
Introduction: Main duct intraductal papillary mucinous neoplasms (MD-IPMNs) are a subtype of pancreatic cystic neoplasms with a well-established potential for malignant transformation. Although a rare finding, spontaneous fistulization of IPMNs into the gastrointestinal (GI) tract may indicate advanced histologic progression. We present a case of an MD-IPMN fistulizing into the duodenum, ultimately found to be invasive mucinous adenocarcinoma following surgical resection.
Case Description/
Methods: A 70-year-old male with a known history of pancreatic cystic lesion presented with abdominal pain, nausea and weight loss. CT imaging showed a heterogeneous 5.5 × 3.8 × 4.5 cm cystic mass lesion with pancreatic duct dilation (up to 12 mm), parenchymal atrophy, and scattered calcifications within the pancreatic body, likely due to chronic pancreatitis (figure 1). Endoscopic ultrasound was performed, and a 4.1 x 3.3 cm heterogeneous cystic lesion was identified in the pancreatic head with ill-defined borders and communication with the pancreatic duct (figure 2A). Fine-needle aspiration (FNA) revealed a mucinous neoplasm with low- to intermediate-grade dysplasia. Furthermore, a 2 cm excavated area containing mucinous material was seen endoscopically in the distal duodenal bulb (figure 2B). Biopsy of this area showed mucinous columnar epithelium with papillary architecture and low-grade dysplasia, concerning for MD-IPMN with spontaneous fistulization. Patient underwent a Whipple procedure. Final pathology showed moderately differentiated invasive mucinous adenocarcinoma arising from IPMN. At six-month follow-up, he remained asymptomatic and was tolerating adjuvant chemotherapy.
Discussion: Fistula formation of MD-IPMNs into adjacent organs may signal more aggressive disease biology and is often associated with high-grade dysplasia or invasive carcinoma1. Proposed mechanisms for fistula formation include mucin hypersecretion, chronic inflammation, and enzymatic autodigestion2. Presence of tumor cells near the fistula tract may reflect direct invasion and a worse prognosis. Extended resection, such as pancreaticoduodenectomy, is often necessary for margin clearance. This case highlights the importance of recognizing GI fistulization as a marker of advanced MD-IPMN, warranting early evaluation for surgical resection even when cytology from FNA suggests low or intermediate-grade dysplasia.
References

Figure: Figure 1: Axial CT image demonstrating a heterogeneous cystic mass lesion in the pancreatic head.
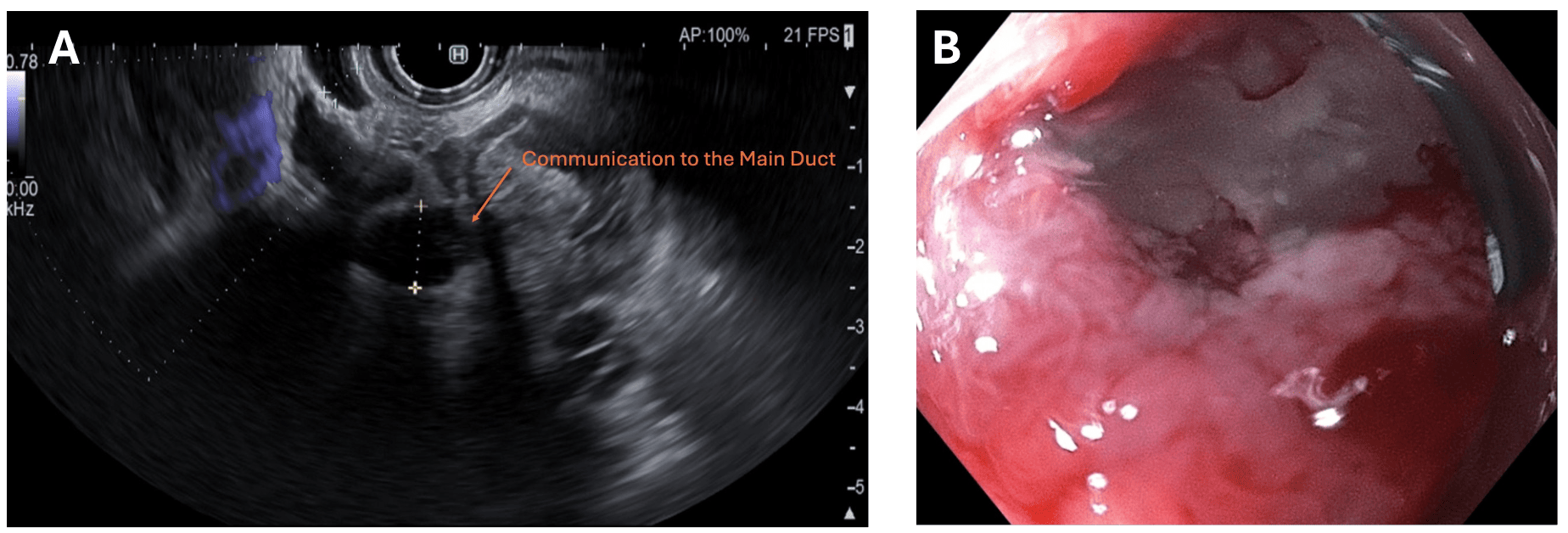
Figure: Figure 2: (A) Endoscopic ultrasound (EUS) showing a cystic lesion with hypoechoic components and ill-defined borders in the pancreatic head communicating to a dilated main pancreatic duct, consistent with MD-IPMN. (B) Upper endoscopy revealing an excavated area containing mucinous material in the duodenal bulb, later confirmed on biopsy to contain mucinous epithelium with papillary architecture and low-grade dysplasia, consistent with fistulization from the IPMN.
Disclosures:
Amirali Tavangar indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Suhail Sidhu indicated no relevant financial relationships.
Bryant Le indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Christopher Paiji indicated no relevant financial relationships.
Amirali Tavangar, MD1, Peter Nguyen, MD2, Frances Dang, MD, MSc3, Suhail Sidhu, MD2, Bryant Le, MD2, Momin Masroor, MD2, Jason Samarasena, MD, MBA, FACG2, Christopher Paiji, MD1. P4421 - Duodenal Fistulization of Main Duct IPMN: A Rare Indicator of Invasive Transformation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Amirali Tavangar, MD1, Peter Nguyen, MD2, Frances Dang, MD, MSc3, Suhail Sidhu, MD2, Bryant Le, MD2, Momin Masroor, MD2, Jason Samarasena, MD, MBA, FACG2, Christopher Paiji, MD1
1University of California Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine, Orange, CA; 3University of California Irvine, Irvine, CA
Introduction: Main duct intraductal papillary mucinous neoplasms (MD-IPMNs) are a subtype of pancreatic cystic neoplasms with a well-established potential for malignant transformation. Although a rare finding, spontaneous fistulization of IPMNs into the gastrointestinal (GI) tract may indicate advanced histologic progression. We present a case of an MD-IPMN fistulizing into the duodenum, ultimately found to be invasive mucinous adenocarcinoma following surgical resection.
Case Description/
Methods: A 70-year-old male with a known history of pancreatic cystic lesion presented with abdominal pain, nausea and weight loss. CT imaging showed a heterogeneous 5.5 × 3.8 × 4.5 cm cystic mass lesion with pancreatic duct dilation (up to 12 mm), parenchymal atrophy, and scattered calcifications within the pancreatic body, likely due to chronic pancreatitis (figure 1). Endoscopic ultrasound was performed, and a 4.1 x 3.3 cm heterogeneous cystic lesion was identified in the pancreatic head with ill-defined borders and communication with the pancreatic duct (figure 2A). Fine-needle aspiration (FNA) revealed a mucinous neoplasm with low- to intermediate-grade dysplasia. Furthermore, a 2 cm excavated area containing mucinous material was seen endoscopically in the distal duodenal bulb (figure 2B). Biopsy of this area showed mucinous columnar epithelium with papillary architecture and low-grade dysplasia, concerning for MD-IPMN with spontaneous fistulization. Patient underwent a Whipple procedure. Final pathology showed moderately differentiated invasive mucinous adenocarcinoma arising from IPMN. At six-month follow-up, he remained asymptomatic and was tolerating adjuvant chemotherapy.
Discussion: Fistula formation of MD-IPMNs into adjacent organs may signal more aggressive disease biology and is often associated with high-grade dysplasia or invasive carcinoma1. Proposed mechanisms for fistula formation include mucin hypersecretion, chronic inflammation, and enzymatic autodigestion2. Presence of tumor cells near the fistula tract may reflect direct invasion and a worse prognosis. Extended resection, such as pancreaticoduodenectomy, is often necessary for margin clearance. This case highlights the importance of recognizing GI fistulization as a marker of advanced MD-IPMN, warranting early evaluation for surgical resection even when cytology from FNA suggests low or intermediate-grade dysplasia.
References
- Shishido Y, et al. Medicine. 2023 Jul 7; 102(27): e34288.
- Yamada Y, et al. Abdom Imaging. 2012 Feb; 37: 100–109.

Figure: Figure 1: Axial CT image demonstrating a heterogeneous cystic mass lesion in the pancreatic head.
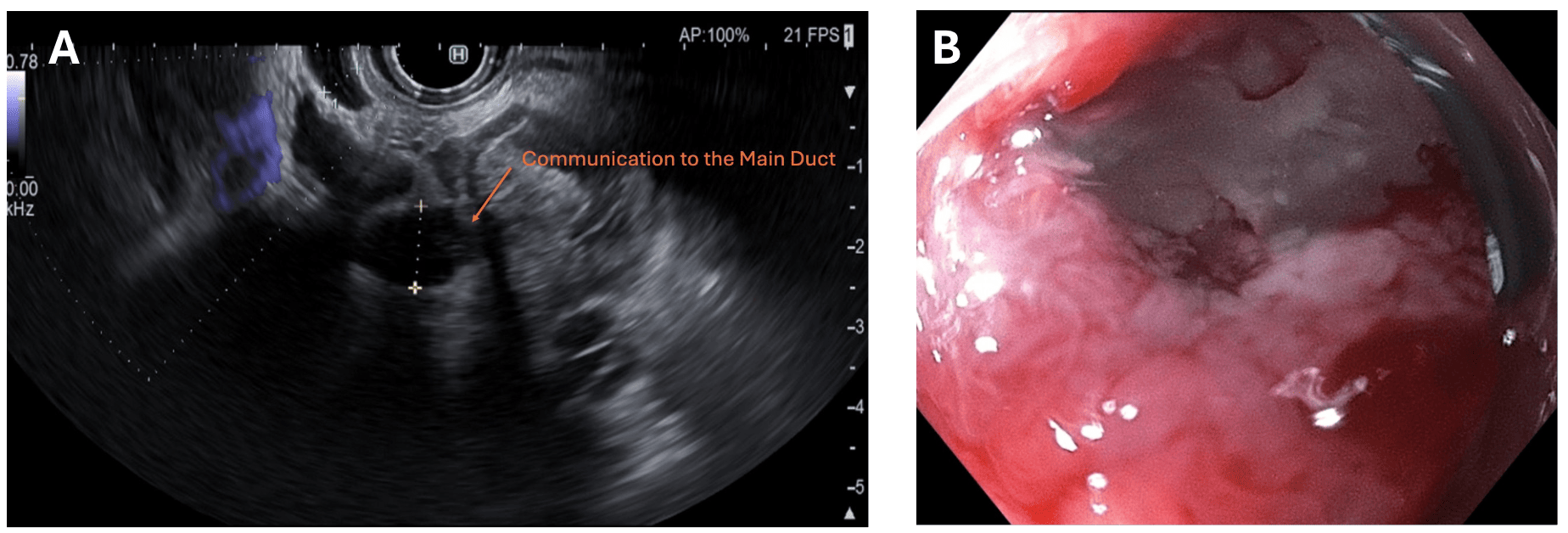
Figure: Figure 2: (A) Endoscopic ultrasound (EUS) showing a cystic lesion with hypoechoic components and ill-defined borders in the pancreatic head communicating to a dilated main pancreatic duct, consistent with MD-IPMN. (B) Upper endoscopy revealing an excavated area containing mucinous material in the duodenal bulb, later confirmed on biopsy to contain mucinous epithelium with papillary architecture and low-grade dysplasia, consistent with fistulization from the IPMN.
Disclosures:
Amirali Tavangar indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Suhail Sidhu indicated no relevant financial relationships.
Bryant Le indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Christopher Paiji indicated no relevant financial relationships.
Amirali Tavangar, MD1, Peter Nguyen, MD2, Frances Dang, MD, MSc3, Suhail Sidhu, MD2, Bryant Le, MD2, Momin Masroor, MD2, Jason Samarasena, MD, MBA, FACG2, Christopher Paiji, MD1. P4421 - Duodenal Fistulization of Main Duct IPMN: A Rare Indicator of Invasive Transformation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

