Tuesday Poster Session
Category: Biliary/Pancreas
P4420 - Perforated Emphysematous Cholecystitis as a Complication of a Pancreaticoduodenal Artery Pseudoaneurysm
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Haseeb Mohideen, MD (he/him/his)
University of Tennessee Health Science Center
Chattanooga, TN
Presenting Author(s)
Haseeb Mohideen, MD, Noah Lubin, MD, Laxmi Parsa, MD
University of Tennessee Health Science Center, Chattanooga, TN
Introduction: A pseudoaneurysm is a false aneurysm that develops from an arterial breach resulting in a hematoma contained within the outermost layer of the arterial wall or surrounding perivascular soft tissue. Common etiologies of pseudoaneurysms include pancreatitis, trauma, vasculitis, and iatrogenic injury. While complications typically arise from rupture and hemorrhage, in rare instances, mass effect from a pseudoaneurysm can result in complications such as gastric outlet, duodenal, or biliary obstruction.
Case Description/
Methods: A 72-year-old male with a history of a pulmonary embolism on rivaroxaban presented to the hospital for abdominal pain. His vitals were stable, and his exam was notable for jaundice and epigastric tenderness. Labs demonstrated significantly elevated total bilirubin with associated transaminitis. CT revealed a pancreaticoduodenal artery (PDA) pseudoaneurysm with mass effect on the biliary tree, severe common bile duct dilatation, and marked gallbladder distension. He successfully underwent IR-guided coil embolization of the pseudoaneurysm and ERCP with placement of a plastic stent in the common bile duct. The patient then had rapid improvement of his total bilirubin and abdominal pain. Four days following his ERCP, the patient developed septic shock with rebound tenderness. A repeat CT showed appropriate positioning of the embolization coils and the biliary stent; however, perforated emphysematous cholecystitis was now observed. The patient subsequently underwent emergent open cholecystectomy, and following the surgery, he gradually improved with antibiotics before eventually being discharged from the hospital.
Discussion: A PDA pseudoaneurysm is a rare but serious etiology of biliary obstruction that has been known to lead to significant complications such as pancreatitis or cholangitis. In such cases, management typically involves endovascular or surgical intervention of the pseudoaneurysm and ERCP with stenting for biliary decompression. To the best of our knowledge, emphysematous or perforated cholecystitis has not been reported in the context of biliary obstruction secondary to a visceral pseudoaneurysm. This case highlights that even if adequate biliary decompression and endovascular intervention is achieved, patients may still be at risk for additional severe complications. Optimal management is unclear, but early cholecystectomy may be beneficial for patients who are at high risk for complicated cholecystitis to prevent adverse outcomes and improve survival.
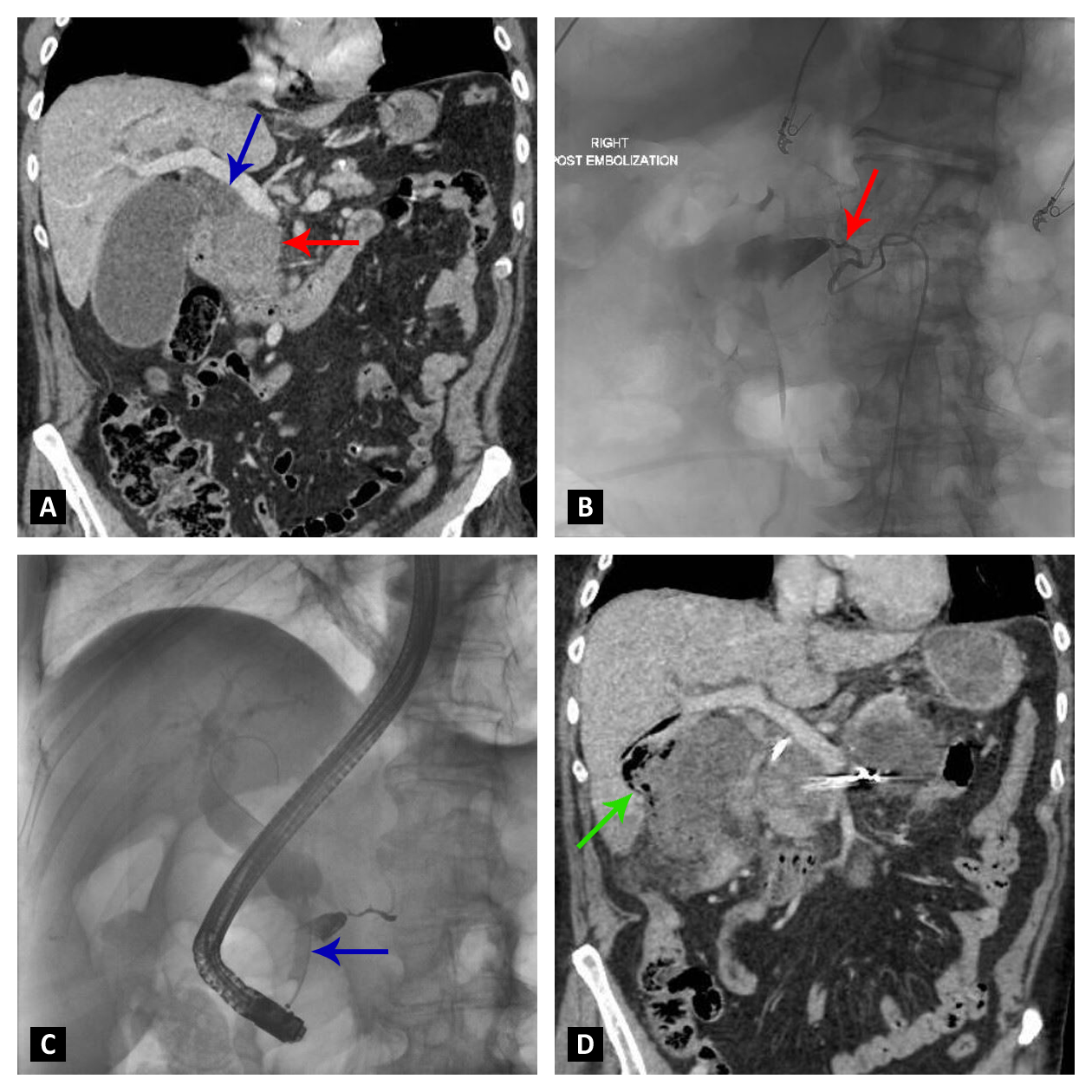
Figure: Figure A: Pre-procedure CT demonstrating a PDA pseudoaneurysm (red arrow) with adjacent mass effect on the biliary system resulting in significant biliary dilatation (blue arrow) and gallbladder distension.
Figure B: Angiogram demonstrating coil embolization (red arrow) of a PDA pseudoaneurysm.
Figure C: Cholangiogram demonstrating severe stenosis of the distal common bile duct (blue arrow) with marked upstream dilatation.
Figure D: Post-procedure CT demonstrating appropriate placement of embolization coils and biliary stent. Emphysematous cholecystitis with perforation and gallbladder contents contained within the hepatic parenchyma is now visualized (green arrow).
Disclosures:
Haseeb Mohideen indicated no relevant financial relationships.
Noah Lubin indicated no relevant financial relationships.
Laxmi Parsa indicated no relevant financial relationships.
Haseeb Mohideen, MD, Noah Lubin, MD, Laxmi Parsa, MD. P4420 - Perforated Emphysematous Cholecystitis as a Complication of a Pancreaticoduodenal Artery Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Tennessee Health Science Center, Chattanooga, TN
Introduction: A pseudoaneurysm is a false aneurysm that develops from an arterial breach resulting in a hematoma contained within the outermost layer of the arterial wall or surrounding perivascular soft tissue. Common etiologies of pseudoaneurysms include pancreatitis, trauma, vasculitis, and iatrogenic injury. While complications typically arise from rupture and hemorrhage, in rare instances, mass effect from a pseudoaneurysm can result in complications such as gastric outlet, duodenal, or biliary obstruction.
Case Description/
Methods: A 72-year-old male with a history of a pulmonary embolism on rivaroxaban presented to the hospital for abdominal pain. His vitals were stable, and his exam was notable for jaundice and epigastric tenderness. Labs demonstrated significantly elevated total bilirubin with associated transaminitis. CT revealed a pancreaticoduodenal artery (PDA) pseudoaneurysm with mass effect on the biliary tree, severe common bile duct dilatation, and marked gallbladder distension. He successfully underwent IR-guided coil embolization of the pseudoaneurysm and ERCP with placement of a plastic stent in the common bile duct. The patient then had rapid improvement of his total bilirubin and abdominal pain. Four days following his ERCP, the patient developed septic shock with rebound tenderness. A repeat CT showed appropriate positioning of the embolization coils and the biliary stent; however, perforated emphysematous cholecystitis was now observed. The patient subsequently underwent emergent open cholecystectomy, and following the surgery, he gradually improved with antibiotics before eventually being discharged from the hospital.
Discussion: A PDA pseudoaneurysm is a rare but serious etiology of biliary obstruction that has been known to lead to significant complications such as pancreatitis or cholangitis. In such cases, management typically involves endovascular or surgical intervention of the pseudoaneurysm and ERCP with stenting for biliary decompression. To the best of our knowledge, emphysematous or perforated cholecystitis has not been reported in the context of biliary obstruction secondary to a visceral pseudoaneurysm. This case highlights that even if adequate biliary decompression and endovascular intervention is achieved, patients may still be at risk for additional severe complications. Optimal management is unclear, but early cholecystectomy may be beneficial for patients who are at high risk for complicated cholecystitis to prevent adverse outcomes and improve survival.
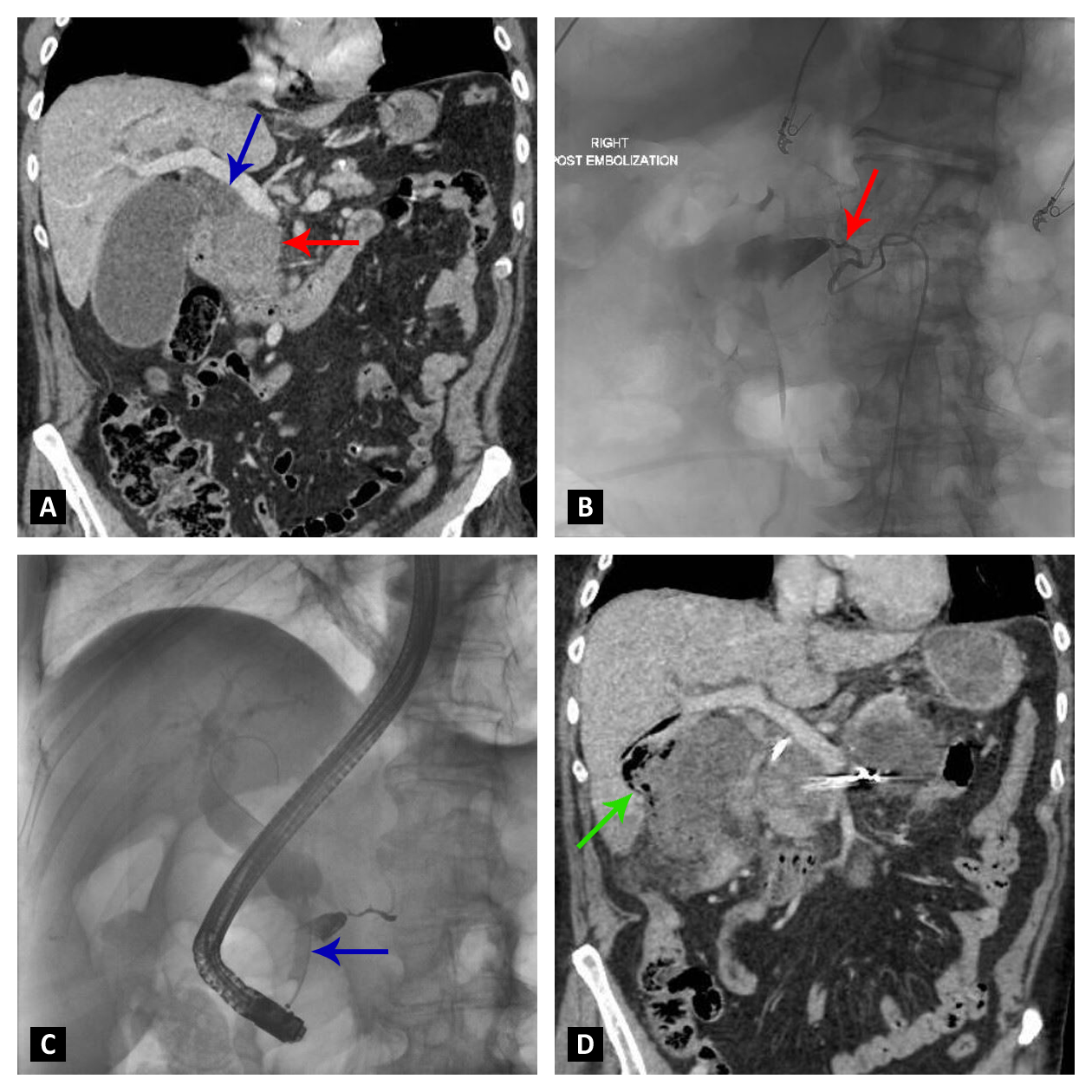
Figure: Figure A: Pre-procedure CT demonstrating a PDA pseudoaneurysm (red arrow) with adjacent mass effect on the biliary system resulting in significant biliary dilatation (blue arrow) and gallbladder distension.
Figure B: Angiogram demonstrating coil embolization (red arrow) of a PDA pseudoaneurysm.
Figure C: Cholangiogram demonstrating severe stenosis of the distal common bile duct (blue arrow) with marked upstream dilatation.
Figure D: Post-procedure CT demonstrating appropriate placement of embolization coils and biliary stent. Emphysematous cholecystitis with perforation and gallbladder contents contained within the hepatic parenchyma is now visualized (green arrow).
Disclosures:
Haseeb Mohideen indicated no relevant financial relationships.
Noah Lubin indicated no relevant financial relationships.
Laxmi Parsa indicated no relevant financial relationships.
Haseeb Mohideen, MD, Noah Lubin, MD, Laxmi Parsa, MD. P4420 - Perforated Emphysematous Cholecystitis as a Complication of a Pancreaticoduodenal Artery Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
