Tuesday Poster Session
Category: Biliary/Pancreas
P4495 - Resolution of Large Cystoduodenal Fistula With Conservative Management in a Patient Status Post Treatment of Walled-Off Necrotizing Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Derek Scholes, MD, RDN
University of Arizona College of Medicine, Phoenix
Phoenix, AZ
Presenting Author(s)
Derek Scholes, MD, RDN1, Sophie Nguyen, BS1, Diwanshu Soni, DO1, Kevin Liu, MD2
1University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 2Banner University Medical Center, Phoenix, AZ
Introduction: Spontaneous cystogastric and cystoduodenal fistulas are rare complications of pancreatitis. We present a case of an unusually large ( >7 cm) spontaneous cystoduodenal fistula in the setting of pancreatitis with complete resolution with conservative management.
Case Description/
Methods: A 41-year-old male with a prior history of necrotizing pancreatitis secondary to alcohol use complicated by walled-off necrosis in the pancreatic tail who underwent EUS-guided cystgastrostomy with serial necrosectomies and ERCP with pancreatic duct placement at our institution. He had his cystgastrostomy stent replaced with plastic double pigtail cystgastrostomy stents after resolution of necrosis but was lost to follow-up for >1 year before re-presenting with abdominal pain and recurrent pancreatitis.
On MRCP at that time, he had notable thickening of the duodenal sweep, acute on chronic pancreatitis changes with retained PD stent. He subsequently underwent ERCP, with a large >7 cm ulcerated fistula tract in the duodenal sweep. The pancreatic duct stent was removed, and a pancreatogram obtained showed direct communication with the ventral pancreatic duct in the neck of the pancreas to the fistula draining into the duodenum. Given adequate pancreatic duct drainage and absence of leak or stricture, no pancreatic duct stent was replaced. Fistula biopsies demonstrated ulcerative exudate without malignancy.
The patient was discharged, and on follow-up EGD and EUS six weeks later, he was noted to have complete resolution of the fistula tract with a small area of residual scarring in the duodenal wall. The patient underwent EUS celiac plexus block with significant improvement of his pain and was able to wean off pain medications.
Discussion: Spontaneous cystoduodenal fistula is a rare complication of pancreatitis. In the case presented, we suspect the patient had spontaneous rupture of a large pseudocyst into the duodenal wall, which resulted in the formation of an unusually large cystoduodenal fistula in the duodenal sweep. The management and long-term clinical outcomes remain ill-defined due to rarity of spontaneous pancreatitis-related fistula. Management of spontaneous cystogastric or cystoduodenal fistula should be individualized based on the size of the residual cystic cavity and the presence of necrosis. In the absence of significant necrosis or residual cyst cavities, these fistulae may heal with conservative management as demonstrated in our case.
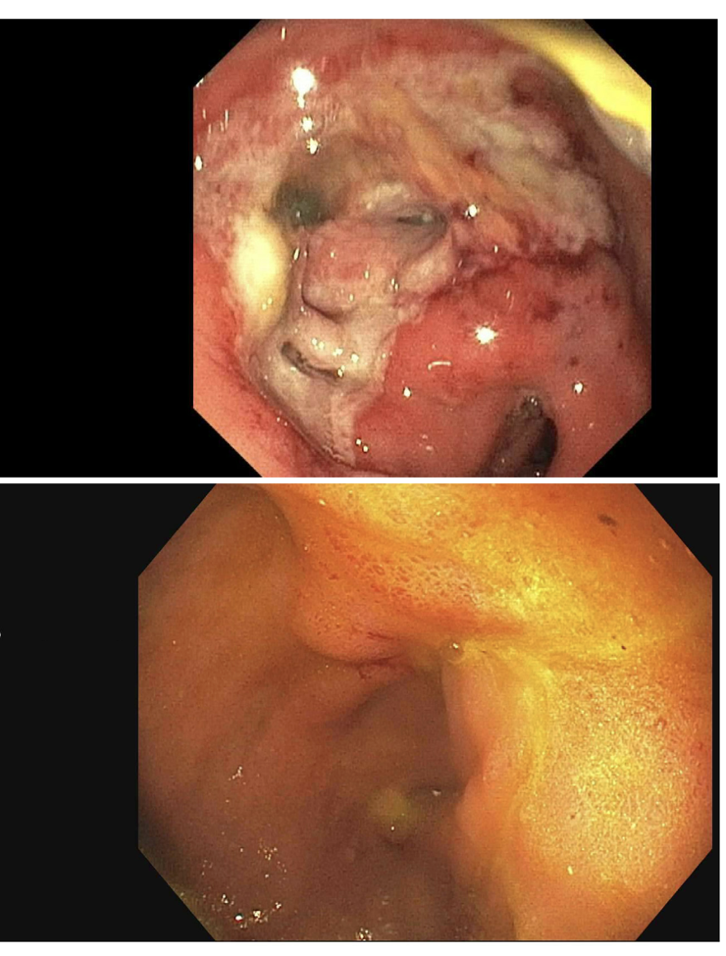
Figure: Cystoduodenal fistula at the duodenal bulb (above) and 6 weeks later complete resolution with conservative management (below)

Figure: Pancreatogram showing pancreaticoduodenal fistula with extravasation of contrast from the neck of the pancreas into the duodenal sweep
Disclosures:
Derek Scholes indicated no relevant financial relationships.
Sophie Nguyen indicated no relevant financial relationships.
Diwanshu Soni indicated no relevant financial relationships.
Kevin Liu indicated no relevant financial relationships.
Derek Scholes, MD, RDN1, Sophie Nguyen, BS1, Diwanshu Soni, DO1, Kevin Liu, MD2. P4495 - Resolution of Large Cystoduodenal Fistula With Conservative Management in a Patient Status Post Treatment of Walled-Off Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, Phoenix, AZ; 2Banner University Medical Center, Phoenix, AZ
Introduction: Spontaneous cystogastric and cystoduodenal fistulas are rare complications of pancreatitis. We present a case of an unusually large ( >7 cm) spontaneous cystoduodenal fistula in the setting of pancreatitis with complete resolution with conservative management.
Case Description/
Methods: A 41-year-old male with a prior history of necrotizing pancreatitis secondary to alcohol use complicated by walled-off necrosis in the pancreatic tail who underwent EUS-guided cystgastrostomy with serial necrosectomies and ERCP with pancreatic duct placement at our institution. He had his cystgastrostomy stent replaced with plastic double pigtail cystgastrostomy stents after resolution of necrosis but was lost to follow-up for >1 year before re-presenting with abdominal pain and recurrent pancreatitis.
On MRCP at that time, he had notable thickening of the duodenal sweep, acute on chronic pancreatitis changes with retained PD stent. He subsequently underwent ERCP, with a large >7 cm ulcerated fistula tract in the duodenal sweep. The pancreatic duct stent was removed, and a pancreatogram obtained showed direct communication with the ventral pancreatic duct in the neck of the pancreas to the fistula draining into the duodenum. Given adequate pancreatic duct drainage and absence of leak or stricture, no pancreatic duct stent was replaced. Fistula biopsies demonstrated ulcerative exudate without malignancy.
The patient was discharged, and on follow-up EGD and EUS six weeks later, he was noted to have complete resolution of the fistula tract with a small area of residual scarring in the duodenal wall. The patient underwent EUS celiac plexus block with significant improvement of his pain and was able to wean off pain medications.
Discussion: Spontaneous cystoduodenal fistula is a rare complication of pancreatitis. In the case presented, we suspect the patient had spontaneous rupture of a large pseudocyst into the duodenal wall, which resulted in the formation of an unusually large cystoduodenal fistula in the duodenal sweep. The management and long-term clinical outcomes remain ill-defined due to rarity of spontaneous pancreatitis-related fistula. Management of spontaneous cystogastric or cystoduodenal fistula should be individualized based on the size of the residual cystic cavity and the presence of necrosis. In the absence of significant necrosis or residual cyst cavities, these fistulae may heal with conservative management as demonstrated in our case.
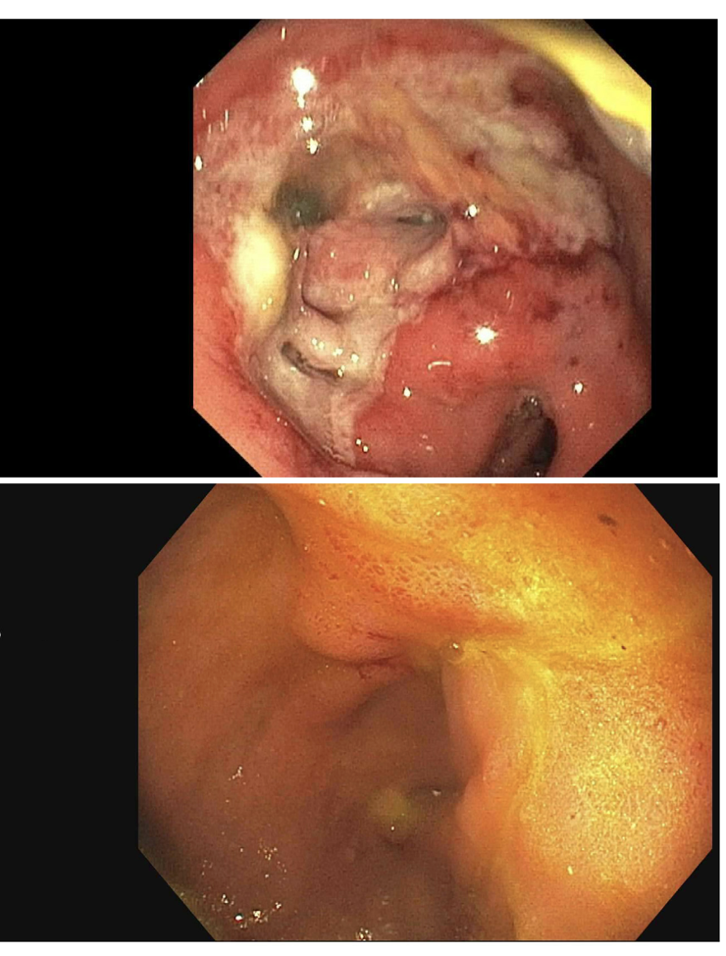
Figure: Cystoduodenal fistula at the duodenal bulb (above) and 6 weeks later complete resolution with conservative management (below)

Figure: Pancreatogram showing pancreaticoduodenal fistula with extravasation of contrast from the neck of the pancreas into the duodenal sweep
Disclosures:
Derek Scholes indicated no relevant financial relationships.
Sophie Nguyen indicated no relevant financial relationships.
Diwanshu Soni indicated no relevant financial relationships.
Kevin Liu indicated no relevant financial relationships.
Derek Scholes, MD, RDN1, Sophie Nguyen, BS1, Diwanshu Soni, DO1, Kevin Liu, MD2. P4495 - Resolution of Large Cystoduodenal Fistula With Conservative Management in a Patient Status Post Treatment of Walled-Off Necrotizing Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
