Tuesday Poster Session
Category: Biliary/Pancreas
P4486 - When an Ulcer Crosses the Line: A Rare Case of Biliary-Duodenal Fistula
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Celise Nardes Ferreira, MD (she/her/hers)
Saint Agnes Medical Center
Fresno, CA
Presenting Author(s)
Celise Nardes Ferreira, MD1, Hamna Javed, MD2, Nicholas S. Reyes, MD3, Ajaypreet Singh, MD1
1Saint Agnes Medical Center, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA, Fresno, CA; 3Saint Agnes medical center, Fresno, CA
Introduction: A choledochoduodenal fistula (CDF) is an abnormal connection between the common bile duct and duodenum [1,2]. These fistulas are rare, with limited case reports since first being described in 1840. The use of advanced hepatobiliary imaging such as ERCP and MRCP has improved their detection [3].
Case Description/
Methods: A 74-year-old female with a history of CKD, HFpEF, valvular disease, HTN, HLD, hypothyroidism, and an outpatient-treated leg ulcer presented after syncopal episode preceded by dizziness and weakness.
In the ED, she was hypotensive, HR 102, with WBC 28.5. She received IV fluids and Ancef for presumed cellulitis. EKG normal sinus rhythm, and chest x-ray showed no acute findings. Admitted for further workup, she later developed severe, non-radiating epigastric pain relieved by pantoprazole. CT A/P revealed extrahepatic biliary dilation (1.4 cm) and duodenal thickening. Blood cultures grew gram-negative rods, and Cefepime was started.
On day 4, she developed new-onset Afib with RVR, hypotension, anemia, and hypoxia. She received 2 units PRBCs and plasma. MRCP showed CBD dilation (10 mm), gallbladder distention, free fluid, duodenal/gastric thickening, and lung consolidations (Figure 1). ERCP identified a bleeding duodenal ulcer with suspected CDF; the ulcer was cauterized, and a biliary stent placed (Figure 2). NSAID deemed likely cause. Antibiotics escalated to Zosyn, and treated with pantoprazole and hydrocortisone.
Due to persistent hypoxia, she was intubated, transferred to ICU for septic shock. Meropenem was started, with improvement allowing extubation the next day. TPN initiated for poor oral intake.
Repeat CT showed improved duodenal thickening, early ileus, CDF, CBD stenosis with patent stent, intrahepatic pneumobilia, and free fluid. WBC rose to 31.5; Meropenem course given with plans for Levaquin on discharge. Despite improvement, she continued to require ICU-level care.
Discussion: This case highlights gram-negative bacteremia and septic shock secondary to a bleeding NSAID-induced duodenal ulcer complicated by CDF—a rare outcome of PUD. Though PUD is common, CDF is rare and may cause sepsis, cholangitis, and biliary obstruction [4,5].
The patient’s nonspecific symptoms initially masked the GI pathology. Imaging and ERCP were key in diagnosing the CDF and managing bleeding. Clinicians should maintain high suspicion for GI sources in elderly patients with sepsis and NSAID use [6]. ERCP remains the diagnostic and therapeutic gold standard [7].
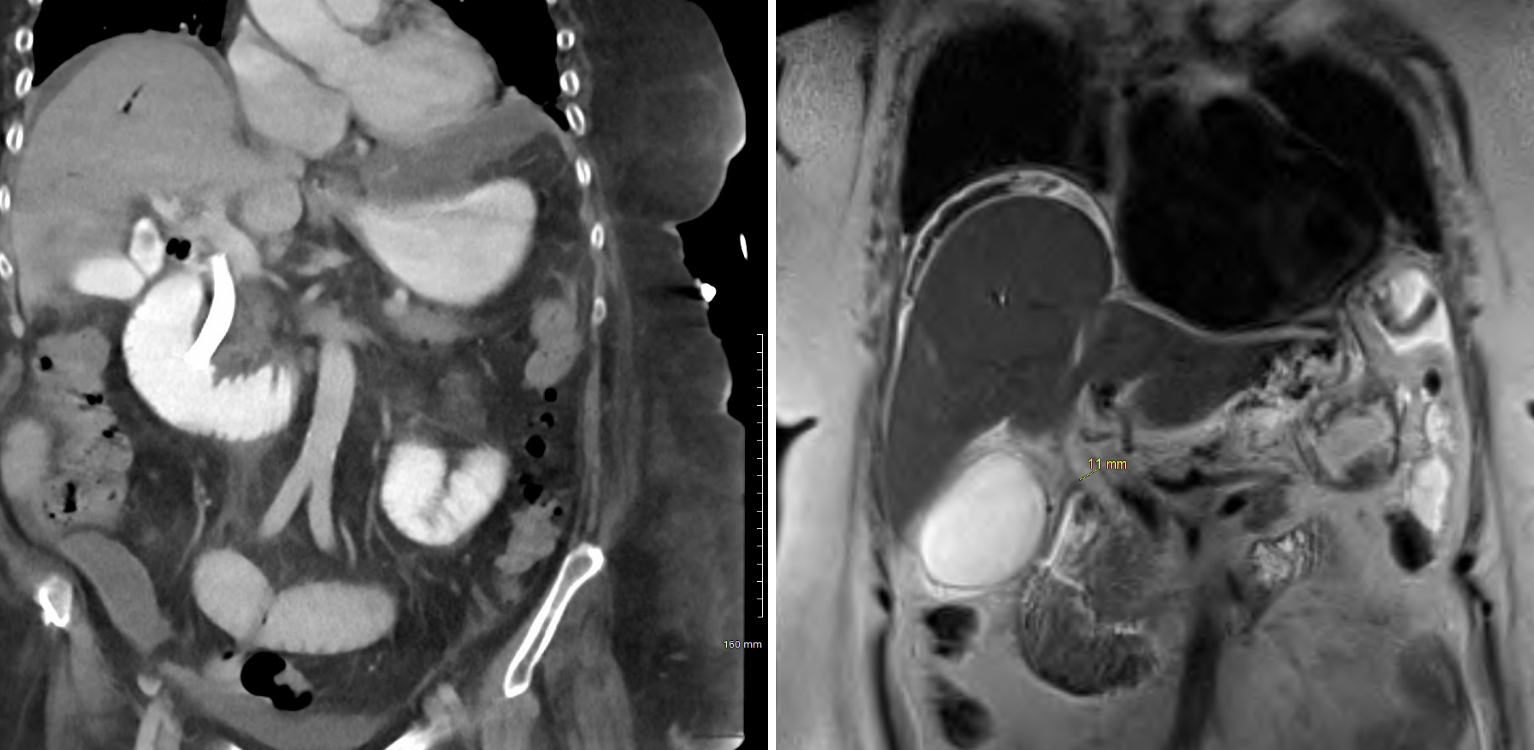
Figure: MRCP showed moderate extrahepatic biliary ductal dilatation with the common duct measuring up to 10 mm, distended gallbladder, small-moderate perihepatic and perisplenic free fluid, thickening of the proximal duodenum and possible gastric antrum and consolidation of the bilateral lower lobes of the lungs
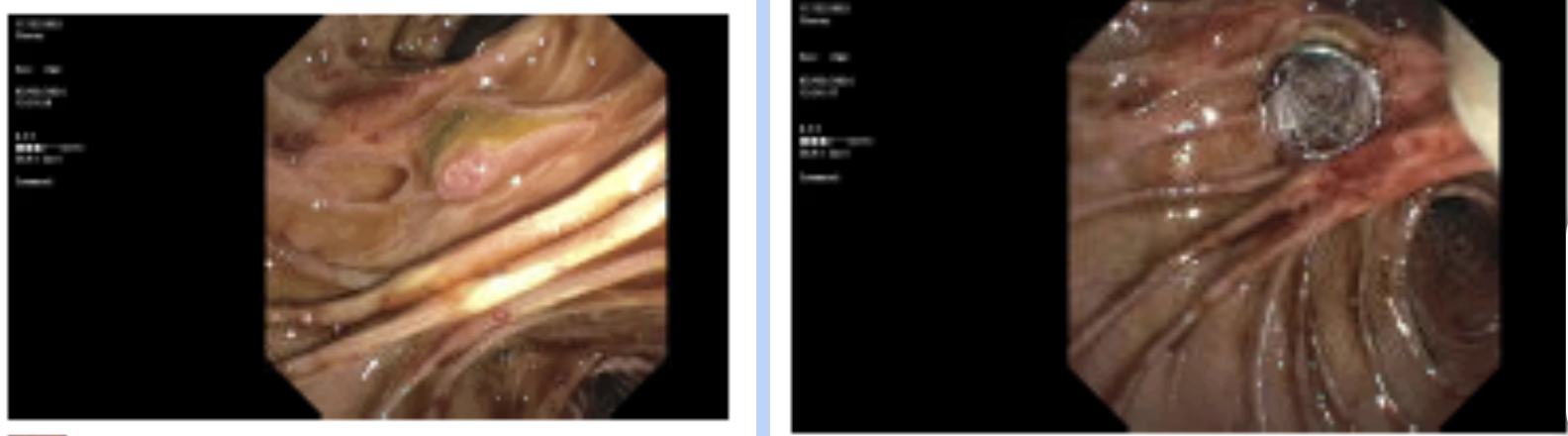
Figure: ERCP showing ulceration of the major papilla, biliary papillary stenosis, and biliary fistula in the middle third of the main bile duct for which a sphincterotomy was done.
Disclosures:
Celise Nardes Ferreira indicated no relevant financial relationships.
Hamna Javed indicated no relevant financial relationships.
Nicholas Reyes indicated no relevant financial relationships.
Ajaypreet Singh indicated no relevant financial relationships.
Celise Nardes Ferreira, MD1, Hamna Javed, MD2, Nicholas S. Reyes, MD3, Ajaypreet Singh, MD1. P4486 - When an Ulcer Crosses the Line: A Rare Case of Biliary-Duodenal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Agnes Medical Center, Fresno, CA; 2Saint Agnes Medical Center, Fresno, CA, Fresno, CA; 3Saint Agnes medical center, Fresno, CA
Introduction: A choledochoduodenal fistula (CDF) is an abnormal connection between the common bile duct and duodenum [1,2]. These fistulas are rare, with limited case reports since first being described in 1840. The use of advanced hepatobiliary imaging such as ERCP and MRCP has improved their detection [3].
Case Description/
Methods: A 74-year-old female with a history of CKD, HFpEF, valvular disease, HTN, HLD, hypothyroidism, and an outpatient-treated leg ulcer presented after syncopal episode preceded by dizziness and weakness.
In the ED, she was hypotensive, HR 102, with WBC 28.5. She received IV fluids and Ancef for presumed cellulitis. EKG normal sinus rhythm, and chest x-ray showed no acute findings. Admitted for further workup, she later developed severe, non-radiating epigastric pain relieved by pantoprazole. CT A/P revealed extrahepatic biliary dilation (1.4 cm) and duodenal thickening. Blood cultures grew gram-negative rods, and Cefepime was started.
On day 4, she developed new-onset Afib with RVR, hypotension, anemia, and hypoxia. She received 2 units PRBCs and plasma. MRCP showed CBD dilation (10 mm), gallbladder distention, free fluid, duodenal/gastric thickening, and lung consolidations (Figure 1). ERCP identified a bleeding duodenal ulcer with suspected CDF; the ulcer was cauterized, and a biliary stent placed (Figure 2). NSAID deemed likely cause. Antibiotics escalated to Zosyn, and treated with pantoprazole and hydrocortisone.
Due to persistent hypoxia, she was intubated, transferred to ICU for septic shock. Meropenem was started, with improvement allowing extubation the next day. TPN initiated for poor oral intake.
Repeat CT showed improved duodenal thickening, early ileus, CDF, CBD stenosis with patent stent, intrahepatic pneumobilia, and free fluid. WBC rose to 31.5; Meropenem course given with plans for Levaquin on discharge. Despite improvement, she continued to require ICU-level care.
Discussion: This case highlights gram-negative bacteremia and septic shock secondary to a bleeding NSAID-induced duodenal ulcer complicated by CDF—a rare outcome of PUD. Though PUD is common, CDF is rare and may cause sepsis, cholangitis, and biliary obstruction [4,5].
The patient’s nonspecific symptoms initially masked the GI pathology. Imaging and ERCP were key in diagnosing the CDF and managing bleeding. Clinicians should maintain high suspicion for GI sources in elderly patients with sepsis and NSAID use [6]. ERCP remains the diagnostic and therapeutic gold standard [7].
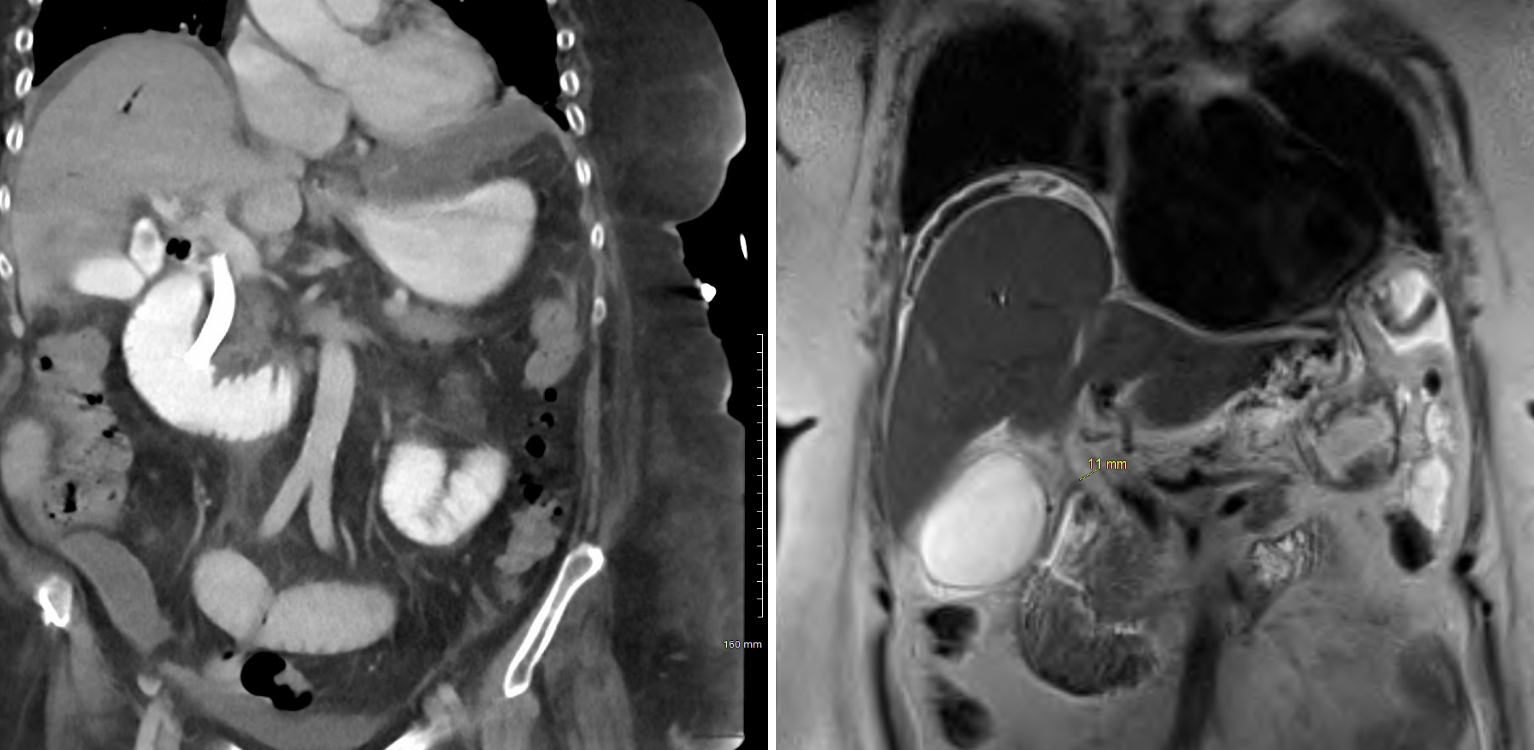
Figure: MRCP showed moderate extrahepatic biliary ductal dilatation with the common duct measuring up to 10 mm, distended gallbladder, small-moderate perihepatic and perisplenic free fluid, thickening of the proximal duodenum and possible gastric antrum and consolidation of the bilateral lower lobes of the lungs
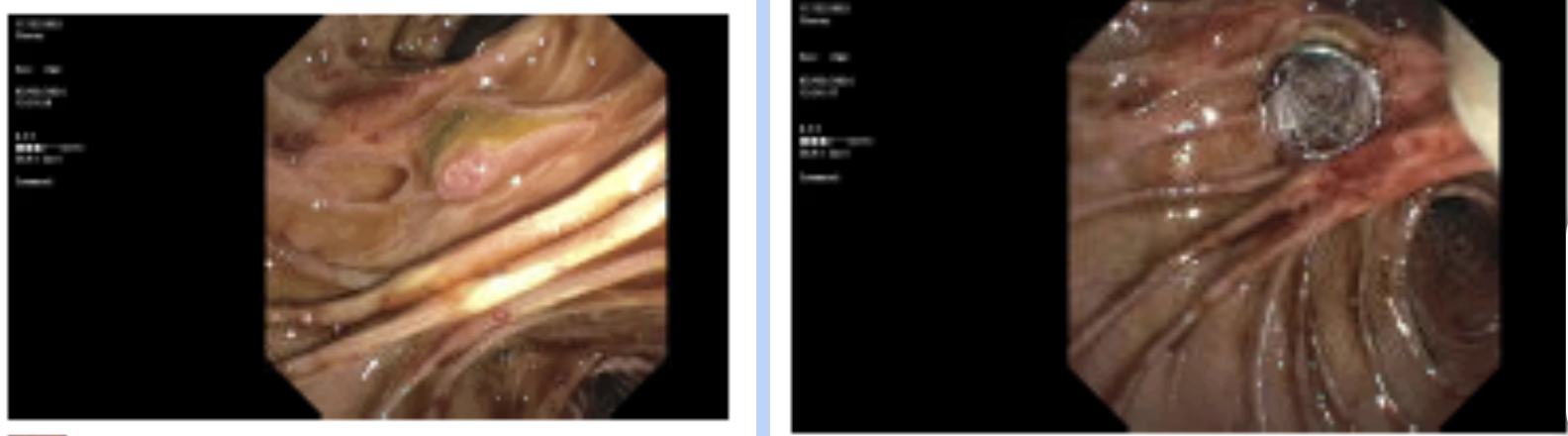
Figure: ERCP showing ulceration of the major papilla, biliary papillary stenosis, and biliary fistula in the middle third of the main bile duct for which a sphincterotomy was done.
Disclosures:
Celise Nardes Ferreira indicated no relevant financial relationships.
Hamna Javed indicated no relevant financial relationships.
Nicholas Reyes indicated no relevant financial relationships.
Ajaypreet Singh indicated no relevant financial relationships.
Celise Nardes Ferreira, MD1, Hamna Javed, MD2, Nicholas S. Reyes, MD3, Ajaypreet Singh, MD1. P4486 - When an Ulcer Crosses the Line: A Rare Case of Biliary-Duodenal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
