Tuesday Poster Session
Category: Biliary/Pancreas
P4483 - Spontaneous Cystoduodenostomy From Pancreatic Pseudocyst Erosion into Duodenum
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hira Hanif, MD
Reading Hospital - Tower Health
Reading, PA
Presenting Author(s)
Hira Hanif, MD1, Iman Waheed, MD1, Arooj Mian, MD1, Farah Harmouch, MD1, John Altomare, MD2
1Reading Hospital - Tower Health, Reading, PA; 2Reading Hospital - Tower Health, Wyomissing, PA
Introduction: Pancreatic pseudocysts are a common complication of severe acute pancreatitis. A spontaneous cystoduodenostomy or cystogastrostomy from a pancreatic pseudocyst erosion into the stomach or duodenum is a rare but serious complication. We present a case of spontaneous cystoduodenal fistula formation resulting in spontaneous decompression of pancreatic pseudocyst.
Case Description/
Methods: 61 y.o.male with past medical history of acute pancreatitis complicated by development of pseudocysts was undergoing outpatient preoperative blood work prior to undergoing surgical cystogastrostomy and was sent to the emergency department due to a low hemoglobin of 5.9. He denied any melena and NSAID use. He reported left-sided abdominal pain from his pancreatic pseudocysts. Physical exam was significant for left sided abdominal tenderness. Labs were remarkable for normocytic anemia with a Hb of 5.9 g/dl. CT scan of the abdomen and pelvis showed necrotic and abscessed pancreas head, body and tail and the abscess was inseparable from the antepyloric region of the stomach. Patient underwent an EGD which showed a large duodenal bulb ulcer with a fistula draining purulent foul smelling fluid and a large amount of necrotic pancreatic tissue in the stomach. The patient subsequently underwent IR guided retroperitoneal drainage of the pseudocyst and abscess.
Discussion: The incidence of pancreatic pseudocysts ranges from 1.0%-4.5% among patients with pancreatitis. Patients can present with postprandial epigastric pain, early satiety, nausea or vomiting. Pseudocysts can be complicated by infection, rupture, hemorrhage, portal hypertension and biliary obstruction. Spontaneous rupture complicates less than 3% of pancreatic pseudocysts. In general, the American College of Gastroenterology and the International Association of Pancreatology/American Pancreatic Association guidelines recommend no intervention if asymptomatic and an absence of infected necrosis, regardless of the size, location, and extension of the pancreatic fluid collection. Surgery, traditionally the mainstay of treatment for pancreatic pseudocysts, is now reserved only for select cases. If drainage is indicated, endoscopic drainage under EUS guidance is preferred. Here we present a case of pancreatic pseudocyst with spontaneous cystoduodenal and possible cystogastric fistula formation resulting in spontaneous decompression of the pseudocyst that was ultimately drained by IR with eventual plan for outpatient surgical cystogastrostomy.
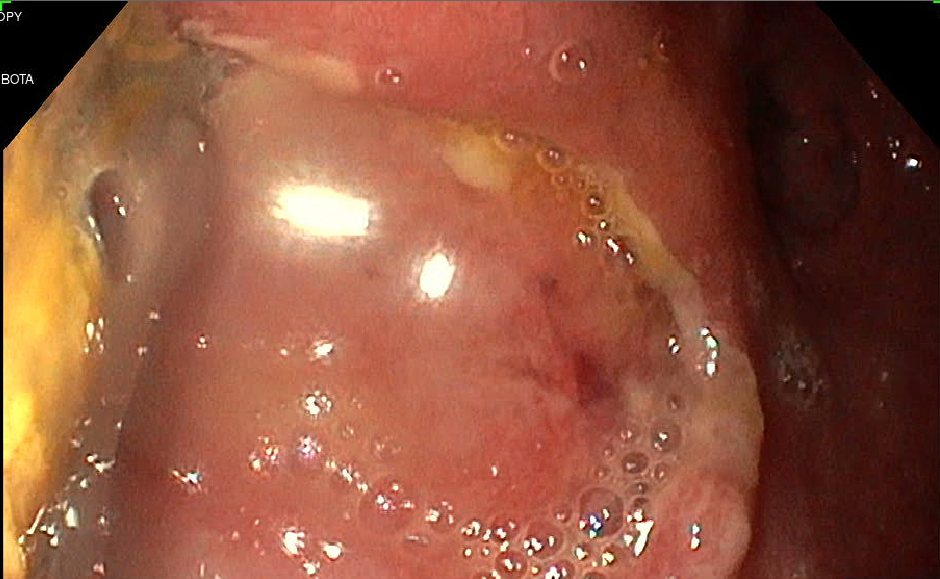
Figure: Duodenal bulb ulcer with fistula formation
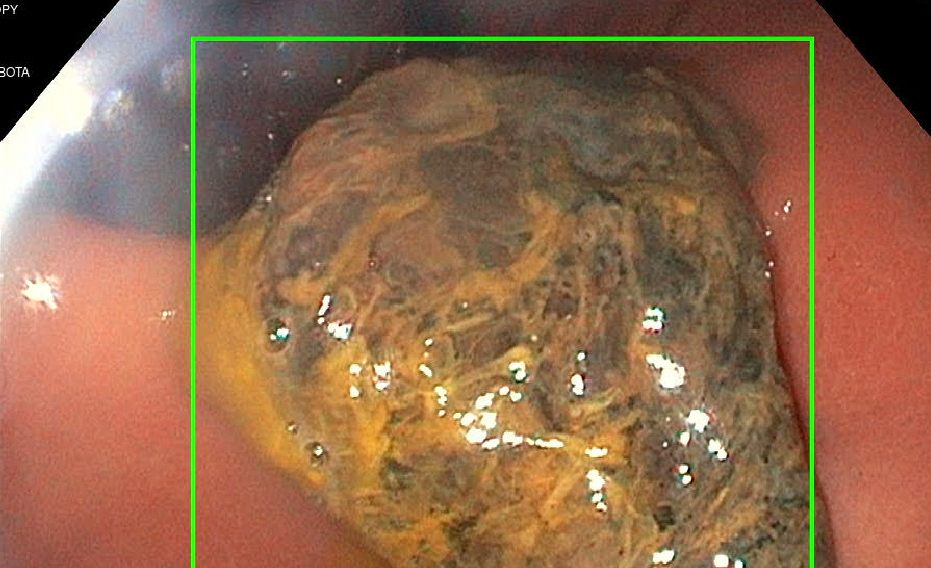
Figure: necrotic pancreatic tissue in stomach
Disclosures:
Hira Hanif indicated no relevant financial relationships.
Iman Waheed indicated no relevant financial relationships.
Arooj Mian indicated no relevant financial relationships.
Farah Harmouch indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Hira Hanif, MD1, Iman Waheed, MD1, Arooj Mian, MD1, Farah Harmouch, MD1, John Altomare, MD2. P4483 - Spontaneous Cystoduodenostomy From Pancreatic Pseudocyst Erosion into Duodenum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Reading Hospital - Tower Health, Reading, PA; 2Reading Hospital - Tower Health, Wyomissing, PA
Introduction: Pancreatic pseudocysts are a common complication of severe acute pancreatitis. A spontaneous cystoduodenostomy or cystogastrostomy from a pancreatic pseudocyst erosion into the stomach or duodenum is a rare but serious complication. We present a case of spontaneous cystoduodenal fistula formation resulting in spontaneous decompression of pancreatic pseudocyst.
Case Description/
Methods: 61 y.o.male with past medical history of acute pancreatitis complicated by development of pseudocysts was undergoing outpatient preoperative blood work prior to undergoing surgical cystogastrostomy and was sent to the emergency department due to a low hemoglobin of 5.9. He denied any melena and NSAID use. He reported left-sided abdominal pain from his pancreatic pseudocysts. Physical exam was significant for left sided abdominal tenderness. Labs were remarkable for normocytic anemia with a Hb of 5.9 g/dl. CT scan of the abdomen and pelvis showed necrotic and abscessed pancreas head, body and tail and the abscess was inseparable from the antepyloric region of the stomach. Patient underwent an EGD which showed a large duodenal bulb ulcer with a fistula draining purulent foul smelling fluid and a large amount of necrotic pancreatic tissue in the stomach. The patient subsequently underwent IR guided retroperitoneal drainage of the pseudocyst and abscess.
Discussion: The incidence of pancreatic pseudocysts ranges from 1.0%-4.5% among patients with pancreatitis. Patients can present with postprandial epigastric pain, early satiety, nausea or vomiting. Pseudocysts can be complicated by infection, rupture, hemorrhage, portal hypertension and biliary obstruction. Spontaneous rupture complicates less than 3% of pancreatic pseudocysts. In general, the American College of Gastroenterology and the International Association of Pancreatology/American Pancreatic Association guidelines recommend no intervention if asymptomatic and an absence of infected necrosis, regardless of the size, location, and extension of the pancreatic fluid collection. Surgery, traditionally the mainstay of treatment for pancreatic pseudocysts, is now reserved only for select cases. If drainage is indicated, endoscopic drainage under EUS guidance is preferred. Here we present a case of pancreatic pseudocyst with spontaneous cystoduodenal and possible cystogastric fistula formation resulting in spontaneous decompression of the pseudocyst that was ultimately drained by IR with eventual plan for outpatient surgical cystogastrostomy.
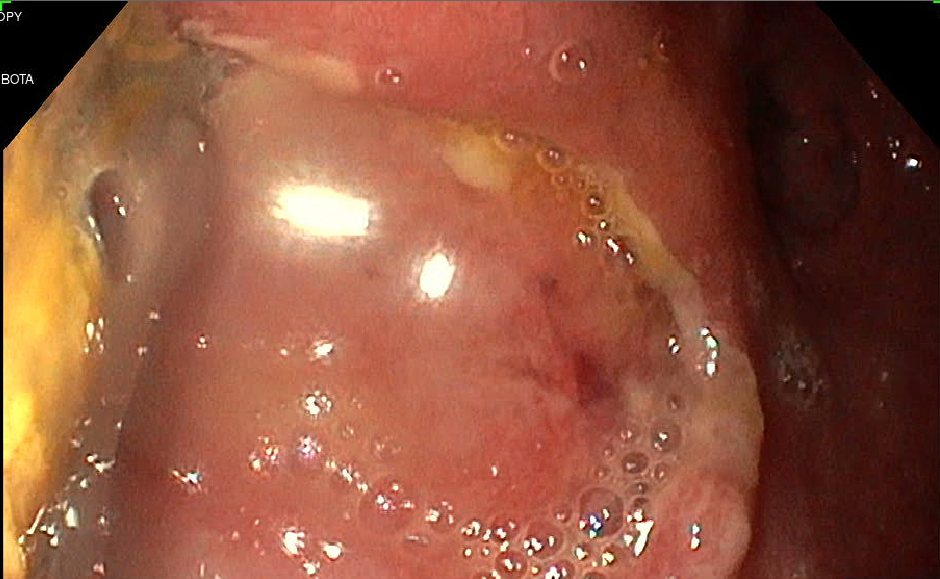
Figure: Duodenal bulb ulcer with fistula formation
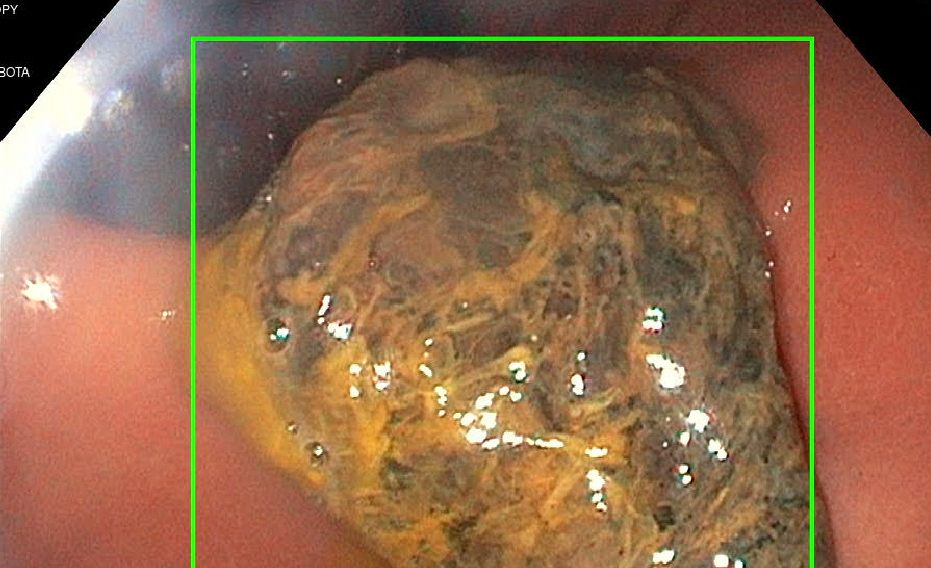
Figure: necrotic pancreatic tissue in stomach
Disclosures:
Hira Hanif indicated no relevant financial relationships.
Iman Waheed indicated no relevant financial relationships.
Arooj Mian indicated no relevant financial relationships.
Farah Harmouch indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Hira Hanif, MD1, Iman Waheed, MD1, Arooj Mian, MD1, Farah Harmouch, MD1, John Altomare, MD2. P4483 - Spontaneous Cystoduodenostomy From Pancreatic Pseudocyst Erosion into Duodenum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

