Tuesday Poster Session
Category: Biliary/Pancreas
P4477 - Triple Trouble With Embedded Metal Biliary Stent: Rare Case of Coexisting Choledocholithiasis and Biliary Stricture Presenting as Acute Cholangitis - Complication Secondary to Embedded Metal Biliary Stent
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mahathi Kunduru, MD
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Mahathi Kunduru, MD1, Abdullah Sultany, MD2
1Guthrie Robert Packer Hospital, Sayre, PA; 2Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Endoscopic biliary stenting is also important to treat obstructive jaundice secondary to biliary strictures, postoperative biliary leaks. Complication range secondary to biliary stenting is between 8 to 10%. Complications noted with biliary stent placement include stent migration, perforation, infection, Stent fracture, rarely embedded stents. We describe a rare case of embedded metal stent resulting in biliary stricture, choledocholithiasis presenting with acute cholangitis
Case Description/
Methods: 40-year-old male with past medical history significant for recurrent pancreatitis presented to ER with right upper quadrant abdominal pain, nausea, and vomiting, jaundice and unintentional weight loss. Labs showed leukocytosis, elevated AST, ALT and ALP. Around 3 years back, he underwent EUS/ERCP as a follow up for necrotizing pancreatitis which showed pancreatic parenchymal atrophy with pancreatic pseudocyst, dilated CBD of 8 mm. Patient underwent sphincterotomy, CBD dilation and a covered metal stent was placed. ERCP for stent removal was planned later, but patient lost to follow-up. Patient now returned with features of obstructive jaundice and above-mentioned symptoms. CTAP showed upper CBD and intrahepatic biliary duct dilatation. He was started on IV fluids and broad-spectrum antibiotics. ERCP showed choledocholithiasis, biliary stricture in the middle third of main bile duct. Biliary stone was removed and a new covered metal stent was placed in the CBD. Previous metal stent could not be removed as it was embedded. Post ERCP, patient had a worsening of his condition characterized by worsening leukocytosis and elevated bilirubin levels. MRCP showed markedly distended gallbladder and biliary tree radicles. Repeat ERCP was tried but could not be finished due to decreased visibility.. Hepatobiliary surgery was consulted for hepatic enterostomy but was not planned as patient had high surgical risk. Underwent percutaneous biliary diversion with drain placement by IR and was discharged in a stable condition.
Discussion: Biliary stent left for a long period can result in chronic inflammation with ingrowth of tissue resulting in complications such as biliary stricture, bile stasis. Chronic stasis of bile could result in formation of sludge and stones in the CBD. Bacterial overgrowth in this environment can result in SIRS, and sepsis. Reimaging is advised if symptoms recur post stenting. The key take away is early stent exchange or removal with patient education for close follow-up for stent removal.
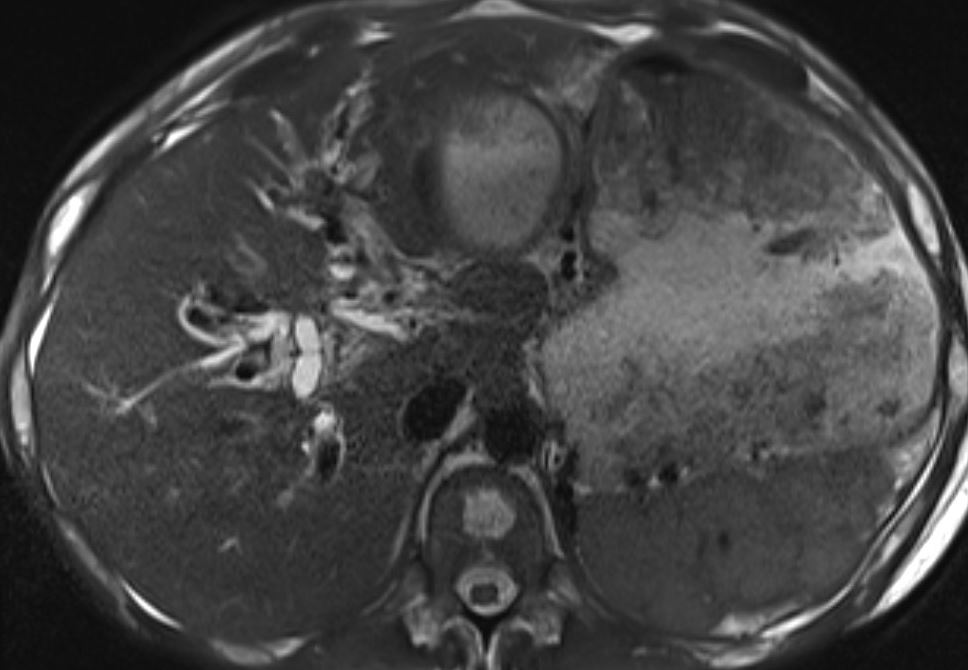
Figure: MRCP showing significant dilation of CBD, biliary radicles and markedly enlarged gallbladder
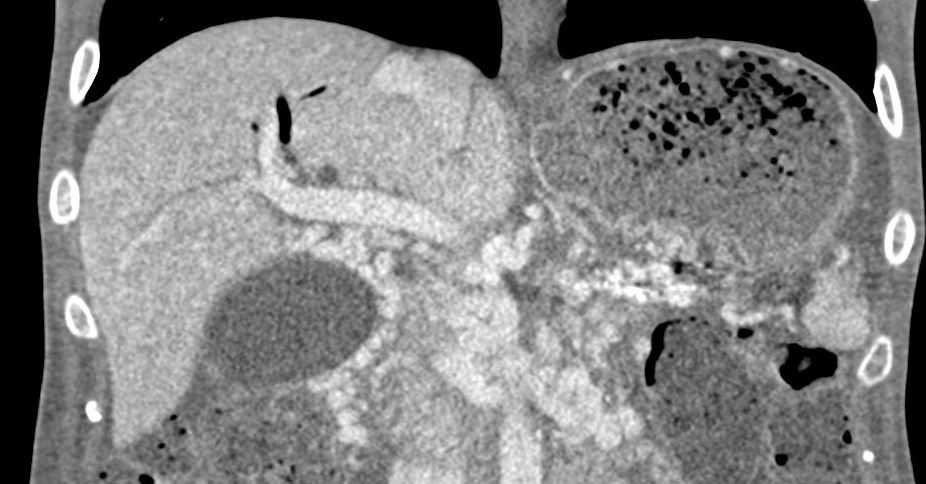
Figure: Coronal Section of CT Abdomen on presentation showing marked CBD dilation, enlarged Gallbladder.
Disclosures:
Mahathi Kunduru indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Mahathi Kunduru, MD1, Abdullah Sultany, MD2. P4477 - Triple Trouble With Embedded Metal Biliary Stent: Rare Case of Coexisting Choledocholithiasis and Biliary Stricture Presenting as Acute Cholangitis - Complication Secondary to Embedded Metal Biliary Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Sayre, PA; 2Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA
Introduction: Endoscopic biliary stenting is also important to treat obstructive jaundice secondary to biliary strictures, postoperative biliary leaks. Complication range secondary to biliary stenting is between 8 to 10%. Complications noted with biliary stent placement include stent migration, perforation, infection, Stent fracture, rarely embedded stents. We describe a rare case of embedded metal stent resulting in biliary stricture, choledocholithiasis presenting with acute cholangitis
Case Description/
Methods: 40-year-old male with past medical history significant for recurrent pancreatitis presented to ER with right upper quadrant abdominal pain, nausea, and vomiting, jaundice and unintentional weight loss. Labs showed leukocytosis, elevated AST, ALT and ALP. Around 3 years back, he underwent EUS/ERCP as a follow up for necrotizing pancreatitis which showed pancreatic parenchymal atrophy with pancreatic pseudocyst, dilated CBD of 8 mm. Patient underwent sphincterotomy, CBD dilation and a covered metal stent was placed. ERCP for stent removal was planned later, but patient lost to follow-up. Patient now returned with features of obstructive jaundice and above-mentioned symptoms. CTAP showed upper CBD and intrahepatic biliary duct dilatation. He was started on IV fluids and broad-spectrum antibiotics. ERCP showed choledocholithiasis, biliary stricture in the middle third of main bile duct. Biliary stone was removed and a new covered metal stent was placed in the CBD. Previous metal stent could not be removed as it was embedded. Post ERCP, patient had a worsening of his condition characterized by worsening leukocytosis and elevated bilirubin levels. MRCP showed markedly distended gallbladder and biliary tree radicles. Repeat ERCP was tried but could not be finished due to decreased visibility.. Hepatobiliary surgery was consulted for hepatic enterostomy but was not planned as patient had high surgical risk. Underwent percutaneous biliary diversion with drain placement by IR and was discharged in a stable condition.
Discussion: Biliary stent left for a long period can result in chronic inflammation with ingrowth of tissue resulting in complications such as biliary stricture, bile stasis. Chronic stasis of bile could result in formation of sludge and stones in the CBD. Bacterial overgrowth in this environment can result in SIRS, and sepsis. Reimaging is advised if symptoms recur post stenting. The key take away is early stent exchange or removal with patient education for close follow-up for stent removal.
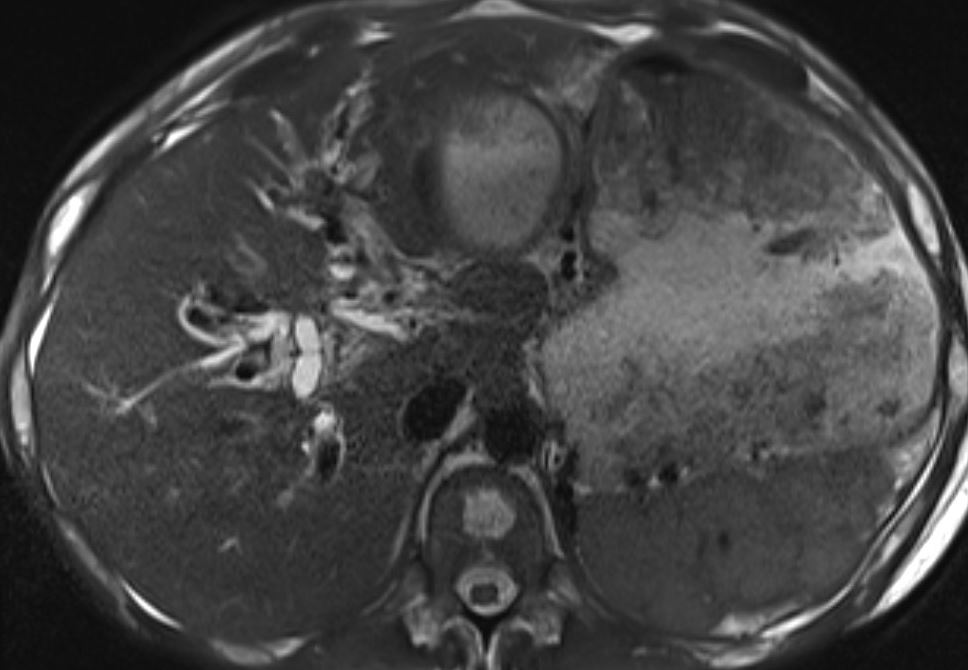
Figure: MRCP showing significant dilation of CBD, biliary radicles and markedly enlarged gallbladder
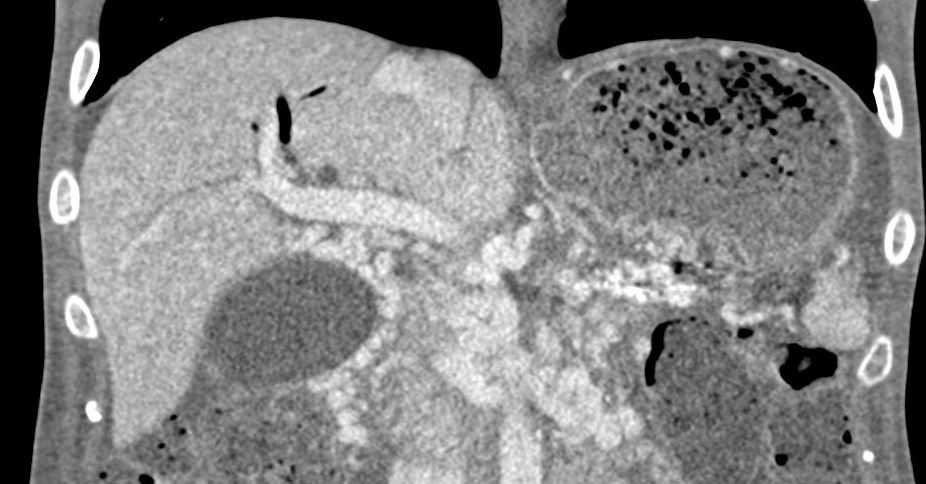
Figure: Coronal Section of CT Abdomen on presentation showing marked CBD dilation, enlarged Gallbladder.
Disclosures:
Mahathi Kunduru indicated no relevant financial relationships.
Abdullah Sultany indicated no relevant financial relationships.
Mahathi Kunduru, MD1, Abdullah Sultany, MD2. P4477 - Triple Trouble With Embedded Metal Biliary Stent: Rare Case of Coexisting Choledocholithiasis and Biliary Stricture Presenting as Acute Cholangitis - Complication Secondary to Embedded Metal Biliary Stent, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
