Tuesday Poster Session
Category: Colon
P4562 - Trends in Colorectal Cancer Screening and Surveillance Among Patients Diagnosed With Colorectal Cancer in a Tertiary Hospital
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gabriela Mendez, MD
University of Illinois College of Medicine
Chicago, IL
Presenting Author(s)
Gabriela Mendez, MD1, Michael Fayad, DO2, Bharathi Chinnakotla, MPH1, Jessica E. McClain, MD2, Hetal Patel, MD1, Keith Naylor, MD3
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL; 3University of Illinois at Chicago, Chicago, IL
Introduction: Colorectal cancer (CRC) incidence and mortality have declined in the United States over the past two decades, largely due to advances in screening and surveillance. However, these improvements have not been equitably experienced across all populations. Disparities in CRC outcomes persist across age, race, ethnicity, and other sociodemographic characteristics. For instance, Black individuals are more likely to be diagnosed at advanced stages compared to white individuals, while data on CRC outcomes among other racial and ethnic groups remain limited. Understanding the barriers to timely CRC detection is critical for developing targeted interventions. This study aims to evaluate the sociodemographic and clinical factors associated with CRC diagnosis in a diverse urban population.
Methods: We conducted a retrospective cross-sectional review of 308 patient records at a tertiary academic medical center. Data collected included demographics, clinical history, prior CRC screening, and diagnostic information. The primary outcome was stage at diagnosis, dichotomized into early stage (I–II) and late stage (III-IV). Descriptive statistics and logistic regression were performed using STATA (Windows).
Results: There were no statistically significant differences in stage at diagnosis by age, sex assigned at birth, race, or ethnicity (Table 1). Patients without a primary care provider (PCP) in the health system performing the colonoscopy were more likely to be diagnosed at a late stage (OR 2.11), as were those without CRC screening in the past 10 years (OR 2.20) (Table 2). In addition, diagnostic colonoscopy was strongly associated with late-stage diagnosis compared to colonoscopy performed for screening (OR 6.5).
Discussion: Our findings underscore the critical role of consistent primary care and timely CRC screening in promoting early detection. As could be expected, patients who were not up to date with CRC screening or who underwent diagnostic colonoscopy were more likely to be diagnosed with late-stage disease. What is notable is the difference in stage at diagnosis based on if the patient had a PCP in the health system performing the colonoscopy. This finding may reflect factors such as adherence to follow-up with a PCP prior to diagnosis or delays in time to colonoscopy after referral. While no significant differences were found by age, sex, race, or ethnicity, further studies involving larger cohorts are needed to assess whether these factors are associated with CRC stage at diagnosis.
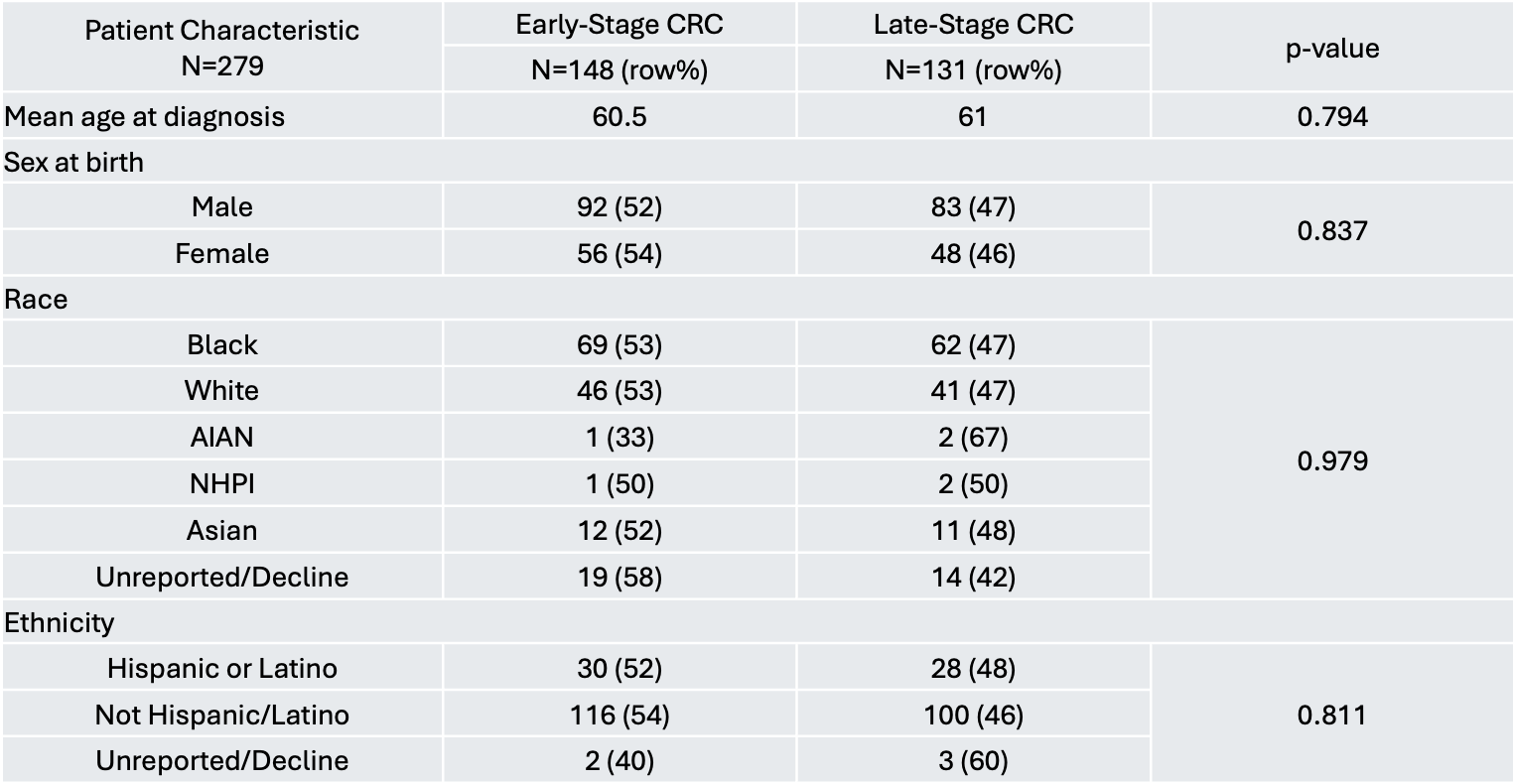
Figure: Table 1. Bivariate Analysis of Characteristics Associated with Early vs. Late Stage Diagnosis. AIAN = American Indian or Alaska Native, HHPI = Native Hawaiian or Other Pacific Islander.
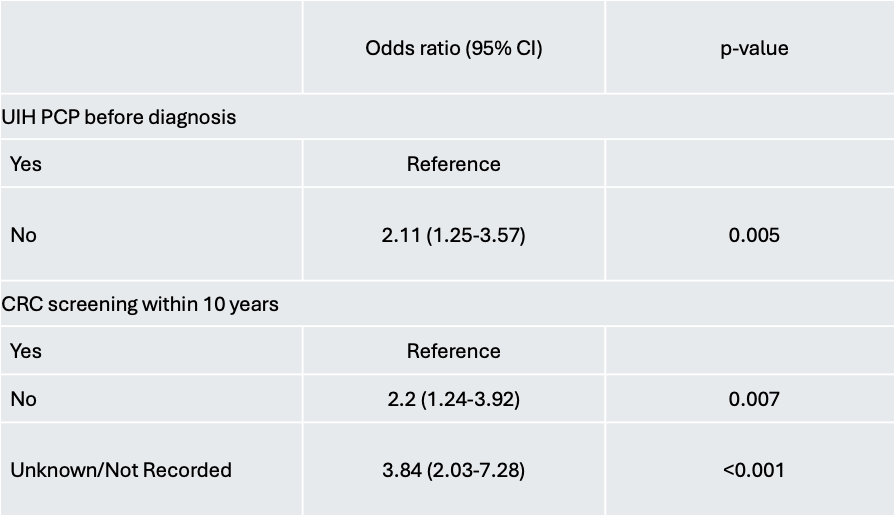
Figure: Table 2. Logistic Regression of Factors Associated with Late-Stage Colorectal Cancer Diagnosis.
Disclosures:
Gabriela Mendez indicated no relevant financial relationships.
Michael Fayad indicated no relevant financial relationships.
Bharathi Chinnakotla indicated no relevant financial relationships.
Jessica McClain indicated no relevant financial relationships.
Hetal Patel indicated no relevant financial relationships.
Keith Naylor indicated no relevant financial relationships.
Gabriela Mendez, MD1, Michael Fayad, DO2, Bharathi Chinnakotla, MPH1, Jessica E. McClain, MD2, Hetal Patel, MD1, Keith Naylor, MD3. P4562 - Trends in Colorectal Cancer Screening and Surveillance Among Patients Diagnosed With Colorectal Cancer in a Tertiary Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Chicago, IL; 2University of Illinois Chicago, Chicago, IL; 3University of Illinois at Chicago, Chicago, IL
Introduction: Colorectal cancer (CRC) incidence and mortality have declined in the United States over the past two decades, largely due to advances in screening and surveillance. However, these improvements have not been equitably experienced across all populations. Disparities in CRC outcomes persist across age, race, ethnicity, and other sociodemographic characteristics. For instance, Black individuals are more likely to be diagnosed at advanced stages compared to white individuals, while data on CRC outcomes among other racial and ethnic groups remain limited. Understanding the barriers to timely CRC detection is critical for developing targeted interventions. This study aims to evaluate the sociodemographic and clinical factors associated with CRC diagnosis in a diverse urban population.
Methods: We conducted a retrospective cross-sectional review of 308 patient records at a tertiary academic medical center. Data collected included demographics, clinical history, prior CRC screening, and diagnostic information. The primary outcome was stage at diagnosis, dichotomized into early stage (I–II) and late stage (III-IV). Descriptive statistics and logistic regression were performed using STATA (Windows).
Results: There were no statistically significant differences in stage at diagnosis by age, sex assigned at birth, race, or ethnicity (Table 1). Patients without a primary care provider (PCP) in the health system performing the colonoscopy were more likely to be diagnosed at a late stage (OR 2.11), as were those without CRC screening in the past 10 years (OR 2.20) (Table 2). In addition, diagnostic colonoscopy was strongly associated with late-stage diagnosis compared to colonoscopy performed for screening (OR 6.5).
Discussion: Our findings underscore the critical role of consistent primary care and timely CRC screening in promoting early detection. As could be expected, patients who were not up to date with CRC screening or who underwent diagnostic colonoscopy were more likely to be diagnosed with late-stage disease. What is notable is the difference in stage at diagnosis based on if the patient had a PCP in the health system performing the colonoscopy. This finding may reflect factors such as adherence to follow-up with a PCP prior to diagnosis or delays in time to colonoscopy after referral. While no significant differences were found by age, sex, race, or ethnicity, further studies involving larger cohorts are needed to assess whether these factors are associated with CRC stage at diagnosis.
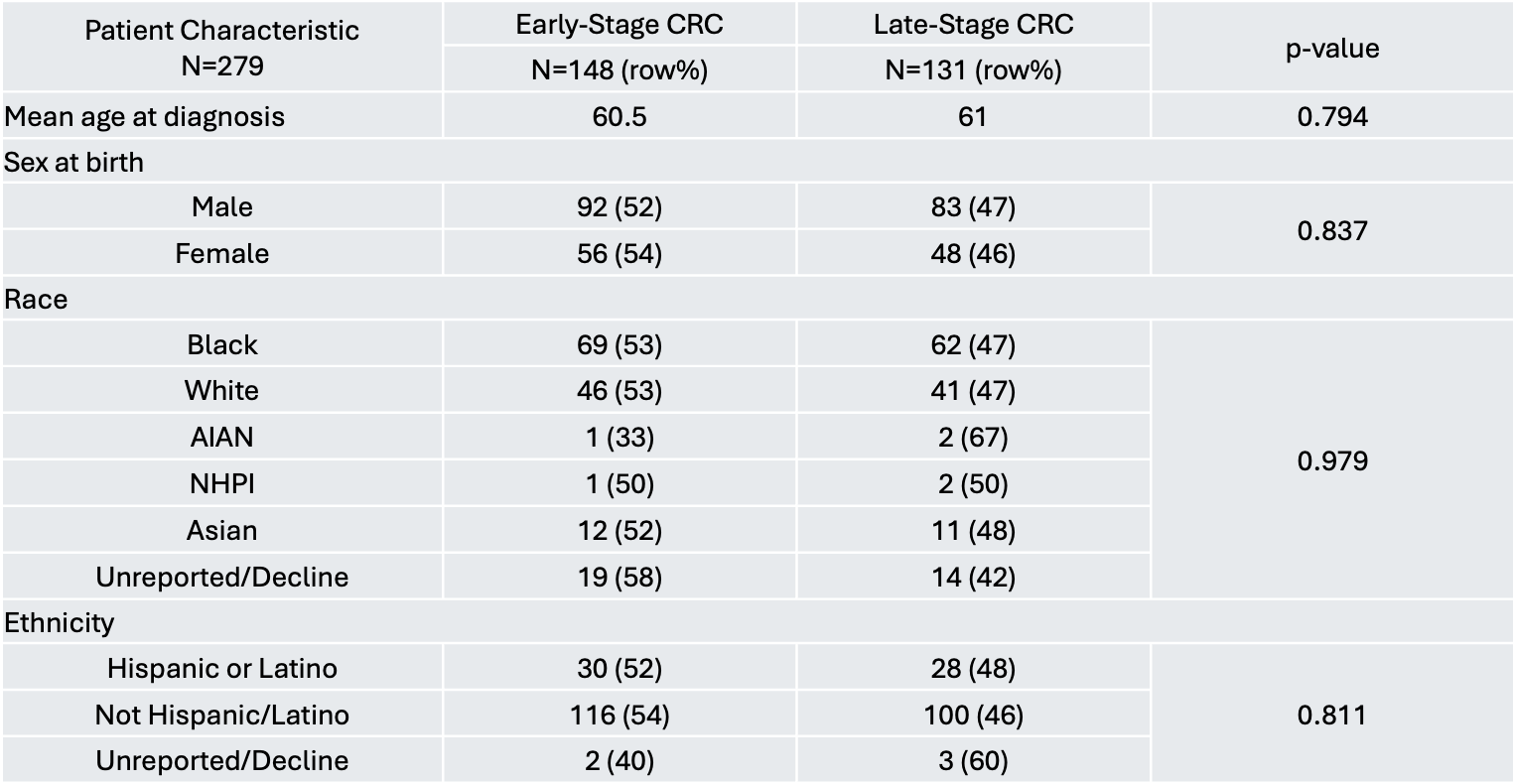
Figure: Table 1. Bivariate Analysis of Characteristics Associated with Early vs. Late Stage Diagnosis. AIAN = American Indian or Alaska Native, HHPI = Native Hawaiian or Other Pacific Islander.
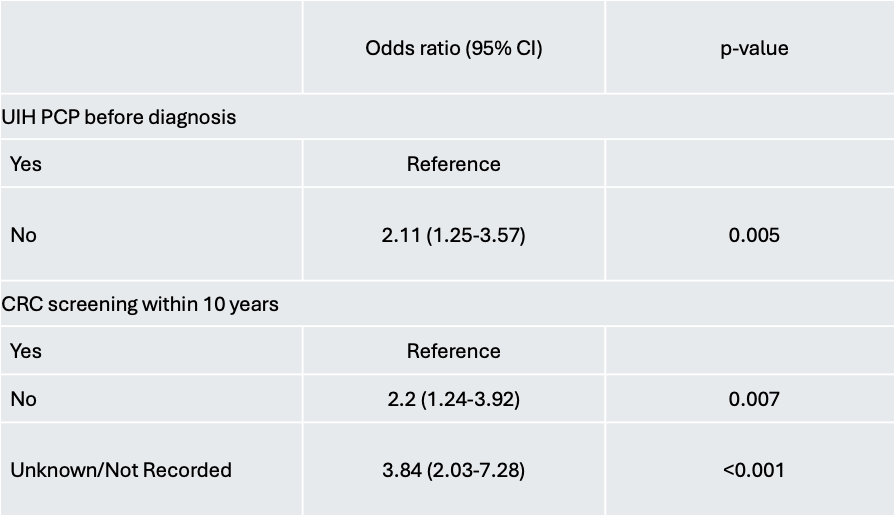
Figure: Table 2. Logistic Regression of Factors Associated with Late-Stage Colorectal Cancer Diagnosis.
Disclosures:
Gabriela Mendez indicated no relevant financial relationships.
Michael Fayad indicated no relevant financial relationships.
Bharathi Chinnakotla indicated no relevant financial relationships.
Jessica McClain indicated no relevant financial relationships.
Hetal Patel indicated no relevant financial relationships.
Keith Naylor indicated no relevant financial relationships.
Gabriela Mendez, MD1, Michael Fayad, DO2, Bharathi Chinnakotla, MPH1, Jessica E. McClain, MD2, Hetal Patel, MD1, Keith Naylor, MD3. P4562 - Trends in Colorectal Cancer Screening and Surveillance Among Patients Diagnosed With Colorectal Cancer in a Tertiary Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
