Tuesday Poster Session
Category: Colon
P4557 - Characteristics, Management, and Outcomes of Gastrointestinal Neuroendocrine Tumors in a Community Hospital Setting With a Predominantly Hispanic Population
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Oyedotun Babajide, MD (he/him/his)
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Oyedotun Babajide, MD1, Julio C. Valencia-Manrique, MD1, Beishi Zheng, MD1, Pushkar Kumar, MD1, Oladimeji E. Oluaderounmu, MD1, Gulce Karaca, MD2, Karan J.. Yagnik, MD3, Jennifer Harley, MD1
1NYC Health + Hospitals/Metropolitan, New York, NY; 2NYC Health + Hospitals/Woodhull, Brooklyn, NY; 3Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ
Introduction: The incidence of gastrointestinal neuroendocrine tumors (GI-NETs) has increased with the broader use of advanced imaging and endoscopy. Despite this rise, variability exists in how these tumors are managed and surveilled. We aimed to evaluate the clinical features, treatment strategies, and outcomes of patients with GI-NETs at a single community hospital with a predominantly Hispanic population.
Methods: We conducted a retrospective review of 44 patients diagnosed with GI-NETs between 2019 and 2024. Demographics, tumor characteristics, treatments, surveillance patterns, and clinical outcomes were analyzed. Categorical variables were summarized as frequencies and percentages; continuous variables were reported as means with standard deviations. Fisher’s exact test was used to assess the association between WHO tumor grade and recurrence.
Results: The cohort included 44 patients with a mean age of 51.9 years (SD ± 13.42), 56.8% female, and 72.7% Hispanic/Latino. Rectal NETs were the most common, accounting for 65.9% (n=29), with 84.1% (n=37) of all tumors measuring ≤1 cm. WHO Grade 1 tumors predominated at 72.7% (n=32), and metastases were observed in 14.6% (n=6). Endoscopic resection was the primary treatment, with Endoscopic full thickness resection (EFTR) in 39.5% (n=15) and Endoscopic mucosal resection (EMR) in 23.7% (n=9). Locoregional therapies were used in 9.1% (n=4) of cases, while systemic therapies were used in 4.5% (n=2). Surveillance was conducted in 70.5% (n=31) of patients, primarily through endoscopy (51.2%, n=22), with a mean duration of 1.53 years (SD ± 0.94). Recurrence occurred in 10.3% (n=3) of patients and was more frequent in higher-grade tumors (5.0% in G1, 14.3% in G2, and 100% in NEC; p = 0.056). The five-year survival rate among patients with available long-term data was 80%.
Discussion: In this predominantly Hispanic cohort, most tumors were low grade and small, with excellent outcomes following endoscopic treatment. Recurrence was uncommon but was more frequently observed in cases with higher tumor grade, supporting the need for risk-adapted surveillance strategies.
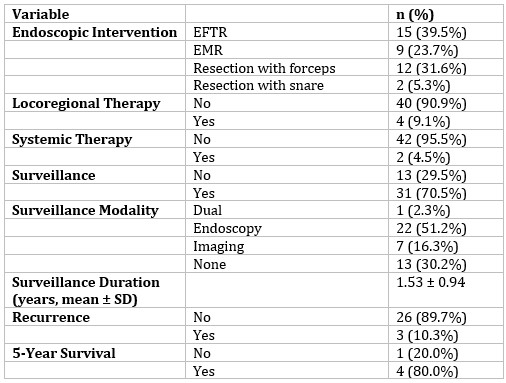
Figure: Table 1: Demographics and Tumor Characteristics of Gastrointestinal Neuroendocrine Tumor Patients
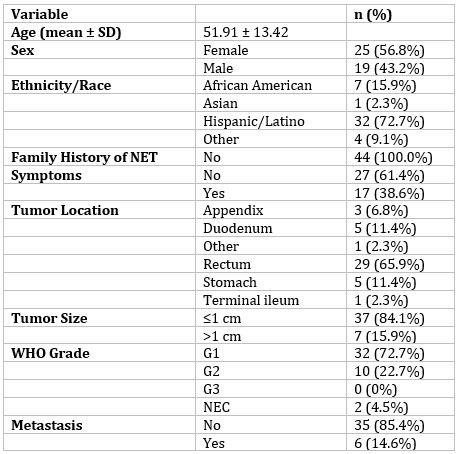
Figure: Table 2. Treatment and Outcomes of Gastrointestinal Neuroendocrine Tumor Patients
Disclosures:
Oyedotun Babajide indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Beishi Zheng indicated no relevant financial relationships.
Pushkar Kumar indicated no relevant financial relationships.
Oladimeji Oluaderounmu indicated no relevant financial relationships.
Gulce Karaca indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Oyedotun Babajide, MD1, Julio C. Valencia-Manrique, MD1, Beishi Zheng, MD1, Pushkar Kumar, MD1, Oladimeji E. Oluaderounmu, MD1, Gulce Karaca, MD2, Karan J.. Yagnik, MD3, Jennifer Harley, MD1. P4557 - Characteristics, Management, and Outcomes of Gastrointestinal Neuroendocrine Tumors in a Community Hospital Setting With a Predominantly Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Metropolitan, New York, NY; 2NYC Health + Hospitals/Woodhull, Brooklyn, NY; 3Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ
Introduction: The incidence of gastrointestinal neuroendocrine tumors (GI-NETs) has increased with the broader use of advanced imaging and endoscopy. Despite this rise, variability exists in how these tumors are managed and surveilled. We aimed to evaluate the clinical features, treatment strategies, and outcomes of patients with GI-NETs at a single community hospital with a predominantly Hispanic population.
Methods: We conducted a retrospective review of 44 patients diagnosed with GI-NETs between 2019 and 2024. Demographics, tumor characteristics, treatments, surveillance patterns, and clinical outcomes were analyzed. Categorical variables were summarized as frequencies and percentages; continuous variables were reported as means with standard deviations. Fisher’s exact test was used to assess the association between WHO tumor grade and recurrence.
Results: The cohort included 44 patients with a mean age of 51.9 years (SD ± 13.42), 56.8% female, and 72.7% Hispanic/Latino. Rectal NETs were the most common, accounting for 65.9% (n=29), with 84.1% (n=37) of all tumors measuring ≤1 cm. WHO Grade 1 tumors predominated at 72.7% (n=32), and metastases were observed in 14.6% (n=6). Endoscopic resection was the primary treatment, with Endoscopic full thickness resection (EFTR) in 39.5% (n=15) and Endoscopic mucosal resection (EMR) in 23.7% (n=9). Locoregional therapies were used in 9.1% (n=4) of cases, while systemic therapies were used in 4.5% (n=2). Surveillance was conducted in 70.5% (n=31) of patients, primarily through endoscopy (51.2%, n=22), with a mean duration of 1.53 years (SD ± 0.94). Recurrence occurred in 10.3% (n=3) of patients and was more frequent in higher-grade tumors (5.0% in G1, 14.3% in G2, and 100% in NEC; p = 0.056). The five-year survival rate among patients with available long-term data was 80%.
Discussion: In this predominantly Hispanic cohort, most tumors were low grade and small, with excellent outcomes following endoscopic treatment. Recurrence was uncommon but was more frequently observed in cases with higher tumor grade, supporting the need for risk-adapted surveillance strategies.
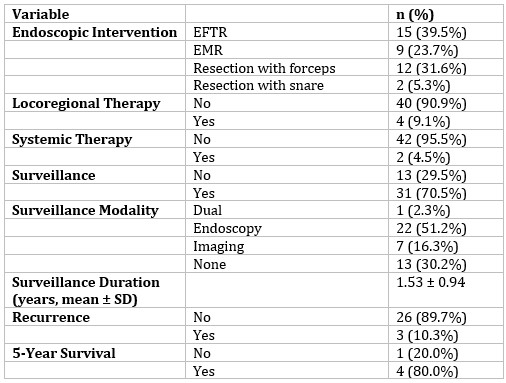
Figure: Table 1: Demographics and Tumor Characteristics of Gastrointestinal Neuroendocrine Tumor Patients
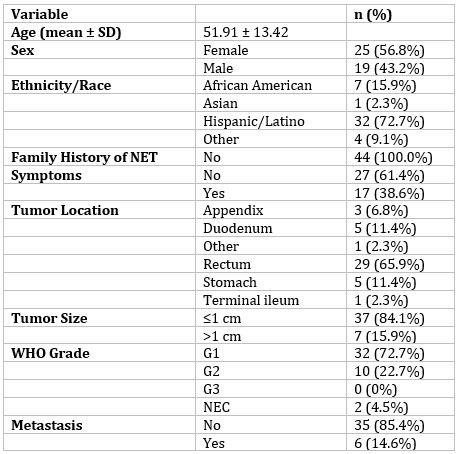
Figure: Table 2. Treatment and Outcomes of Gastrointestinal Neuroendocrine Tumor Patients
Disclosures:
Oyedotun Babajide indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Beishi Zheng indicated no relevant financial relationships.
Pushkar Kumar indicated no relevant financial relationships.
Oladimeji Oluaderounmu indicated no relevant financial relationships.
Gulce Karaca indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Oyedotun Babajide, MD1, Julio C. Valencia-Manrique, MD1, Beishi Zheng, MD1, Pushkar Kumar, MD1, Oladimeji E. Oluaderounmu, MD1, Gulce Karaca, MD2, Karan J.. Yagnik, MD3, Jennifer Harley, MD1. P4557 - Characteristics, Management, and Outcomes of Gastrointestinal Neuroendocrine Tumors in a Community Hospital Setting With a Predominantly Hispanic Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
