Tuesday Poster Session
Category: Colon
P4556 - Hot-EMR vs Cold-EMR for Large Non-Pedunculated Colorectal Polyps: A Cost-Effectiveness Analysis
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2St. Mary Medical Center, Langhorne, PA; 3Mercy Catholic Medical Center, Darby, PA; 4Monmouth Medical Center, Long Branch, NJ; 5University of Kansas School of Medicine, Kansas City, KS; 6Geisinger Health System, Danville, PA; 7Orlando Gastroenterology PA, Orlando, FL
Introduction:
Hot endoscopic mucosal resection (H-EMR) is the standard approach for resecting large non-pedunculated colorectal polyps (LNPCPs), offering deeper tissue excision and lower recurrence rates. However, H-EMR is also associated with higher adverse event risks, particularly delayed post-polypectomy bleeding (DPPB). Cold EMR (C-EMR) has emerged as a safer, non-thermal alternative with reduced bleeding risk, yet its higher recurrence rates remain a concern. Given these trade-offs, this study assesses the cost-effectiveness of H-EMR vs C-EMR for LNPCPs using pooled data from randomized controlled trials and decision modeling.
Methods:
We conducted an incremental cost-effectiveness analysis over a 6 month time horizon using a decision tree model informed by the pooled data of four randomized studies evaluating H-EMR vs C-EMR. Costs—including those for EMR, delayed bleeding and hospitalization, as well as repeat colonoscopy with polypectomy in case of recurrence—were derived from CMS reimbursement data and published sources. Incremental Cost-Effectiveness Ratio (ICER) was determined for the base patient undergoing H-EMR vs C-EMR for ≥20 mm LNPCPs. Analysis was performed using TreeAge Pro Healthcare 2024.
Results:
DPPB was defined as overt bleeding post-procedure, often necessitating transfusion and/or endoscopic intervention. For the Cost-effectiveness analysis of LNPCPs, data from four RCTs comprising 1516 LNPCPs (750 H-EMR; 766 C-EMR) in 1442 patients was utilized. In the base case of a 66.8-year-old patient undergoing endoscopic resection for LNPCPs, Hot-EMR was associated with an incremental cost of -$39.61 and an incremental effectiveness of 0.0001435 QALYs, yielding an ICER of -$275,905 per QALY, indicating cost-savings with H-EMR compared C-EMR at the accepted willingness-to-pay (WTP) threshold of $100,000 per QALY. Based on one-way sensitivity analyses, H-EMR remained cost-effective if the (a) rate of DPPB following H-EMR remains below 4.67% (b) recurrence rate following H-EMR remains below 13.49%.
Discussion:
At the WTP threshold of $100,000 per QALY, our analysis indicates that H-EMR is cost-effective compared to C-EMR for the resection of LNPCPs. While H-EMR carries a modestly higher risk of DPPB, its substantially lower recurrence rate leads to considerable economic benefits. Given the favorable economic profile of H-EMR, it may be the preferred strategy in appropriate patients undergoing resection of LNPCPs. 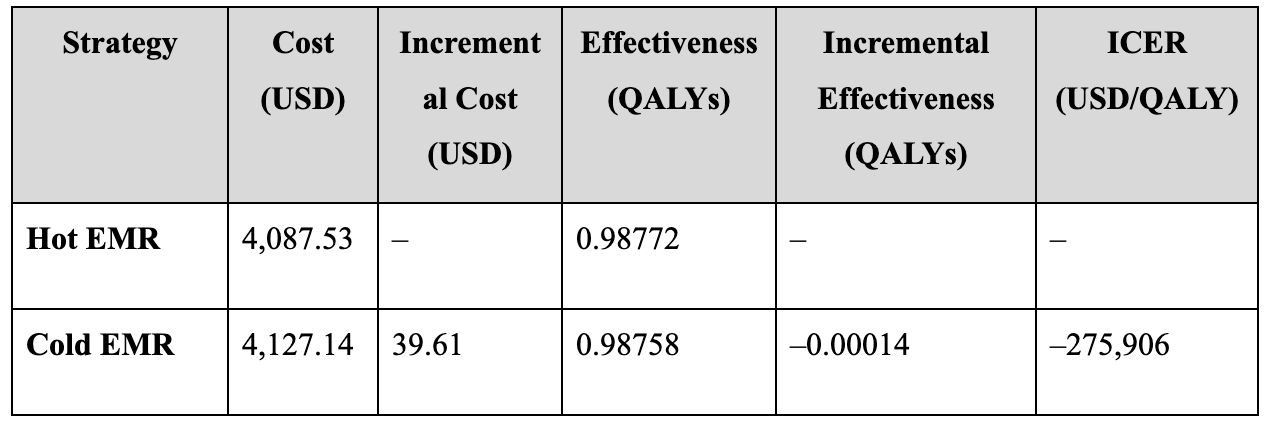
Figure: Table 1: Cost-effectiveness analysis comparing Hot Endoscopic Mucosal Resection (H-EMR) and Cold Endoscopic Mucosal Resection (C-EMR) for the management of large non-pedunculated colorectal polyps (LNPCPs) over a 6-month time horizon. All costs are reported in 2024 USD, and effectiveness is measured in quality-adjusted life years (QALYs). The incremental cost-effectiveness ratio (ICER) reflects the additional cost per QALY gained when comparing H-EMR to C-EMR. A negative ICER indicates cost savings with H-EMR compared to C-EMR at a willingness-to-pay threshold of $100,000 per QALY.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Raj H. Patel, MD2, Charmy Parikh, MD3, Karan Yagnik, MD4, Dushyant S. Dahiya, MD5, Pranav Patel, MD6, Babu P. Mohan, MD7. P4556 - Hot-EMR vs Cold-EMR for Large Non-Pedunculated Colorectal Polyps: A Cost-Effectiveness Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
