Tuesday Poster Session
Category: Colon
P4554 - Single Center Initiative to Standardize and Correct Discrepancies in Bowel Preparation Administration for Inpatient Colonoscopy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KT
Kimberly Tena Diaz, DO (she/her/hers)
Cooper University Health Care
Camden, NJ
Presenting Author(s)
Kimberly Tena Diaz, DO1, Ian Dale, DO2, Kathy Williams, MD, MS3, Tonia T. Liu, BS4, Rachel Frank, MD5
1Cooper University Health Care, Camden, NJ; 2Cooper University Hospital, Camden, NJ; 3Digestive Health Institute at Cooper University Hospital, Camden, NJ; 4Cooper Medical School of Rowan University, Camden, NJ; 5Cooper University Hospital, Philadelphia, PA
Introduction: Inpatient colonoscopy has diagnostic and therapeutic utility in a wide array of pathologies. Optimal visualization is crucial for evaluation of underlying abnormalities, while poor visualization leads to delayed or repeated procedures resulting in increased hospital costs, resource utilization, and delay of patient care. The purpose of our quality improvement study was to identify and overcome barriers to inpatient colonoscopy preparation administration to improve overall visualization quality.
Methods: This is a single center study consisting of a pre-intervention phase evaluating nursing practices and inpatient colonoscopy quality over a 3-month period (1/2/24 - 3/29/24) followed by the creation of an Epic Order-Set to clarify preparation timing and a 3-month post-intervention analysis (2/1/25- 4/30/25). Primary outcomes include quality of colonoscopy preparation as measured via Boston Bowel Preparation Score (BBPS) of the total colon and right colon. Secondary outcomes include the rates at which the cecum is reached, the need for additional preparation on the day of the procedure, the need for multi-day preparation, and the need for repeat inpatient colonoscopy. Outcomes between the pre- and post-intervention phases were compared utilizing Pearson chi-square.
Results: There was a total of 209 patients included in the study, 113 in the pre-intervention phase and 95 in the post-intervention phase. 30 nurses responded to the pre-intervention survey with 83.3% stating that they do not currently administer preparation past midnight. There were no statistically significant differences amongst the pre- and post-intervention groups when comparing total colonoscopy BBPS (p=0.995), right colon BBPS (p=0.290), rates of cecum being reached (p=0.621), frequency at which more bowel preparation was required in the morning (p=0.983), frequency at which repeat inpatient colonoscopies were required (p=0.647) or frequency at which patients required multi-day preparation (p=0.284).
Discussion: Though our study did not reveal statistically significant differences amongst the pre- and post-intervention patients, we found that several other factors may be impacting preparation administration, including patient refusal, intolerability of large volume, variance in which instructions to follow for bowel preparation administration and more. Eliminating additional modifiable factors may contribute to improvement in administration preparation, and additional prospective studies are needed for further evaluation.
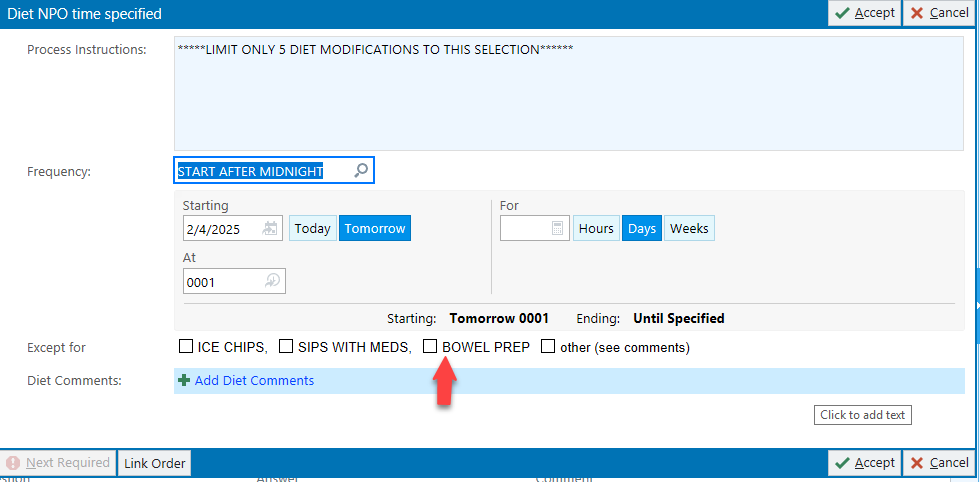
Figure: Figure 1: Nursing survey
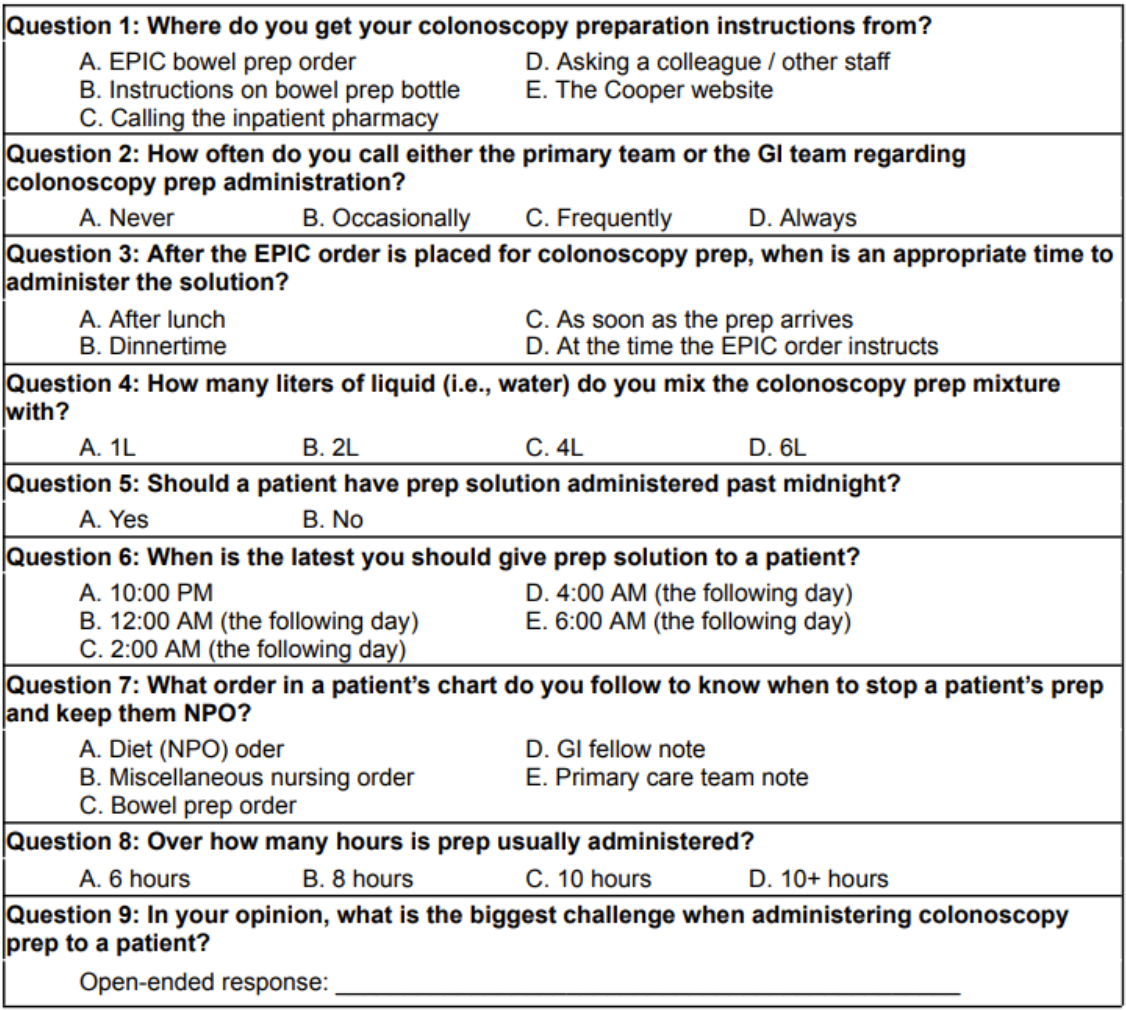
Figure: Figure 2: Epic order-set
Disclosures:
Kimberly Tena Diaz indicated no relevant financial relationships.
Ian Dale indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Tonia Liu indicated no relevant financial relationships.
Rachel Frank indicated no relevant financial relationships.
Kimberly Tena Diaz, DO1, Ian Dale, DO2, Kathy Williams, MD, MS3, Tonia T. Liu, BS4, Rachel Frank, MD5. P4554 - Single Center Initiative to Standardize and Correct Discrepancies in Bowel Preparation Administration for Inpatient Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Health Care, Camden, NJ; 2Cooper University Hospital, Camden, NJ; 3Digestive Health Institute at Cooper University Hospital, Camden, NJ; 4Cooper Medical School of Rowan University, Camden, NJ; 5Cooper University Hospital, Philadelphia, PA
Introduction: Inpatient colonoscopy has diagnostic and therapeutic utility in a wide array of pathologies. Optimal visualization is crucial for evaluation of underlying abnormalities, while poor visualization leads to delayed or repeated procedures resulting in increased hospital costs, resource utilization, and delay of patient care. The purpose of our quality improvement study was to identify and overcome barriers to inpatient colonoscopy preparation administration to improve overall visualization quality.
Methods: This is a single center study consisting of a pre-intervention phase evaluating nursing practices and inpatient colonoscopy quality over a 3-month period (1/2/24 - 3/29/24) followed by the creation of an Epic Order-Set to clarify preparation timing and a 3-month post-intervention analysis (2/1/25- 4/30/25). Primary outcomes include quality of colonoscopy preparation as measured via Boston Bowel Preparation Score (BBPS) of the total colon and right colon. Secondary outcomes include the rates at which the cecum is reached, the need for additional preparation on the day of the procedure, the need for multi-day preparation, and the need for repeat inpatient colonoscopy. Outcomes between the pre- and post-intervention phases were compared utilizing Pearson chi-square.
Results: There was a total of 209 patients included in the study, 113 in the pre-intervention phase and 95 in the post-intervention phase. 30 nurses responded to the pre-intervention survey with 83.3% stating that they do not currently administer preparation past midnight. There were no statistically significant differences amongst the pre- and post-intervention groups when comparing total colonoscopy BBPS (p=0.995), right colon BBPS (p=0.290), rates of cecum being reached (p=0.621), frequency at which more bowel preparation was required in the morning (p=0.983), frequency at which repeat inpatient colonoscopies were required (p=0.647) or frequency at which patients required multi-day preparation (p=0.284).
Discussion: Though our study did not reveal statistically significant differences amongst the pre- and post-intervention patients, we found that several other factors may be impacting preparation administration, including patient refusal, intolerability of large volume, variance in which instructions to follow for bowel preparation administration and more. Eliminating additional modifiable factors may contribute to improvement in administration preparation, and additional prospective studies are needed for further evaluation.
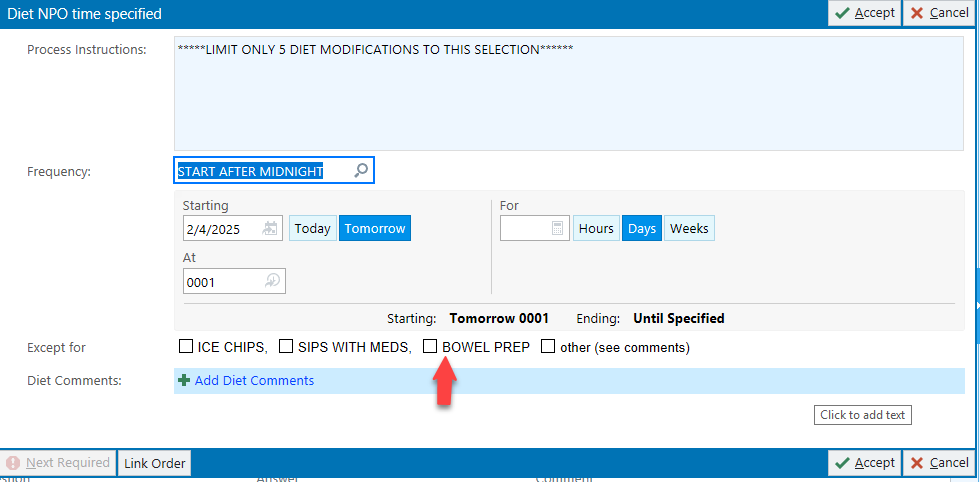
Figure: Figure 1: Nursing survey
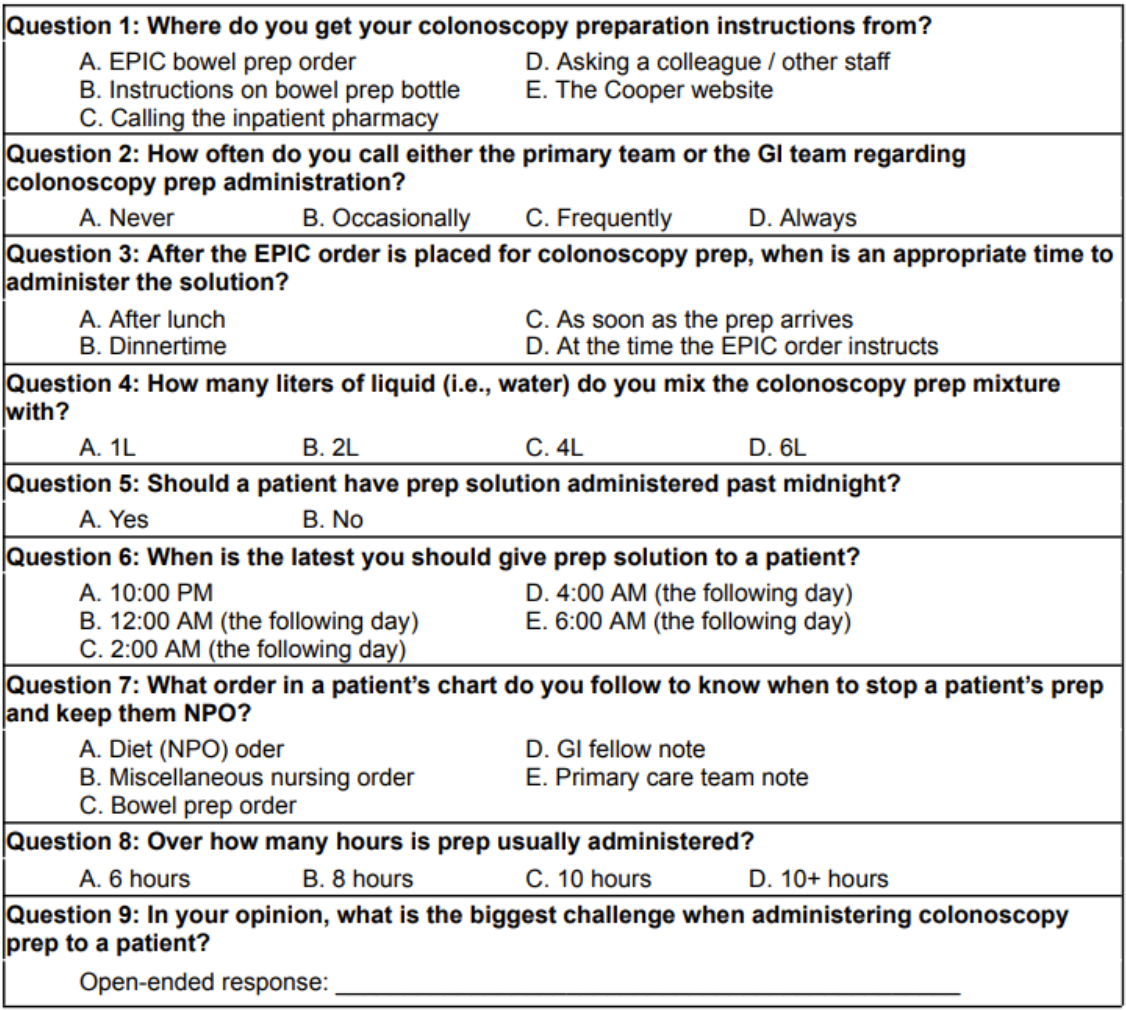
Figure: Figure 2: Epic order-set
Disclosures:
Kimberly Tena Diaz indicated no relevant financial relationships.
Ian Dale indicated no relevant financial relationships.
Kathy Williams indicated no relevant financial relationships.
Tonia Liu indicated no relevant financial relationships.
Rachel Frank indicated no relevant financial relationships.
Kimberly Tena Diaz, DO1, Ian Dale, DO2, Kathy Williams, MD, MS3, Tonia T. Liu, BS4, Rachel Frank, MD5. P4554 - Single Center Initiative to Standardize and Correct Discrepancies in Bowel Preparation Administration for Inpatient Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
