Tuesday Poster Session
Category: Colon
P4598 - Safety and Predictors of Post-Polypectomy Bleeding in Cirrhotic Patients: A Retrospective Cohort Study
.jpg)
Wei Tang, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
1Westchester Medical Center, Valhalla, NY; 2Hackensack University Medical Center, Hackensack, NJ; 3Westchester Medical Center, Elmwood Park, NJ; 4Long Island Jewish Medical Center - Northwell Health, Great Neck, NY; 5New York Medical College, Valhalla, NY
Introduction:
Colonoscopy is the gold standard for colorectal cancer screening and surveillance. In cirrhotic patients, coagulopathy and portal hypertension heighten bleeding risk during endoscopic procedures. Colonoscopy is routinely performed during liver transplant evaluation, yet the safety of polypectomy and predictors of post-polypectomy bleeding (PPB) in this population remain poorly defined.
Methods:
We conducted a retrospective study of cirrhotic patients who underwent colonoscopy for transplant evaluation at a tertiary center (2020–2022). Demographic, clinical, and endoscopic data were reviewed, including polyp characteristics and adverse outcomes (immediate/delayed PPB, hospitalization, transfusion, perforation, death). Statistical comparisons used t-tests and chi-squared tests. Univariate and multivariate logistic regression identified predictors of PPB, with significance set at P ≤ 0.05.
Results:
Among 240 screened patients, 45 underwent 53 colonoscopies with 120 polyps removed (Fig. 1). Post-polypectomy bleeding (PPB) occurred in 8 cases: 7 immediate (5.8%) and 1 delayed (0.8%). All bleeding was managed endoscopically without major complications. One patient (1.9%) required hospitalization, and 4 (7.5%) underwent repeat colonoscopy. No perforations, transfusions, or deaths occurred.
As shown in Table 1, univariate analysis identified elevated bilirubin (0.7–53.8 mg/dL), INR >1.5, lower sodium level (120–147 mEq/L), esophageal varices, larger polyp size, right-sided location, and hot snare use as risk factors for PPB. On multivariate analysis, polyp size, elevated bilirubin, and hot snare use remained significant predictors.
No associations were found with age, sex, albumin, platelet count, creatinine, MELD 3.0, Child-Pugh score, hepatic encephalopathy, hepatocellular carcinoma, or prior GI bleeding. Polyp morphology and histology did not differ between bleeding and non-bleeding cases.
Discussion:
Polypectomy appears safe in cirrhotic patients, with a low risk of major complications. Consistent with prior studies, PPB risk was linked to INR, esophageal varices, right-sided lesions, and hot snare use.
Notably, elevated bilirubin and lower sodium level was also associated with PPB—potential novel markers requiring further validation. Traditional risk factors such as age, low platelets, or ascites were not significant in this cohort. Larger prospective studies are needed to refine risk stratification and improve procedural safety.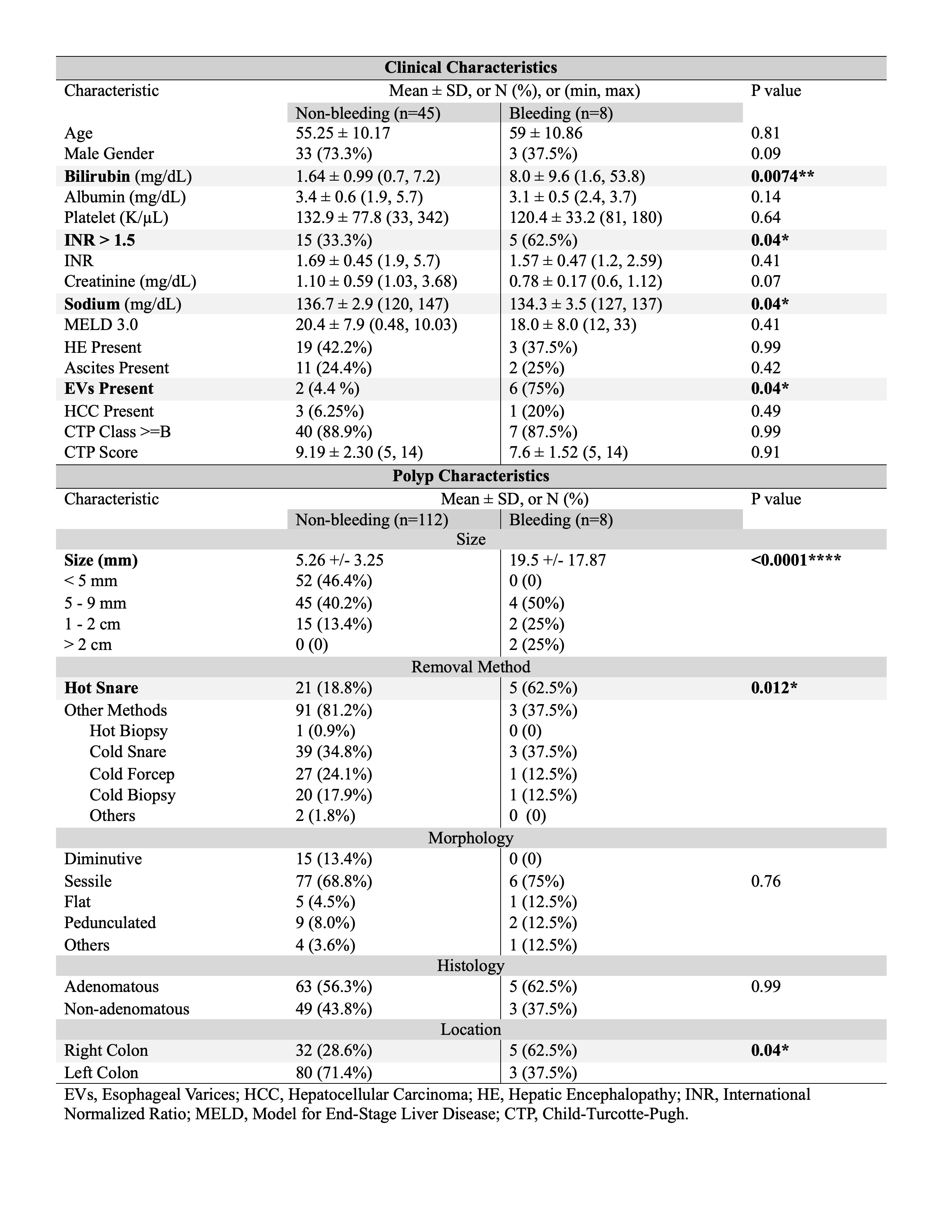
Figure: Figure 1. Identification of Patients, Colonoscopies and Polyps Included in the Analysis. 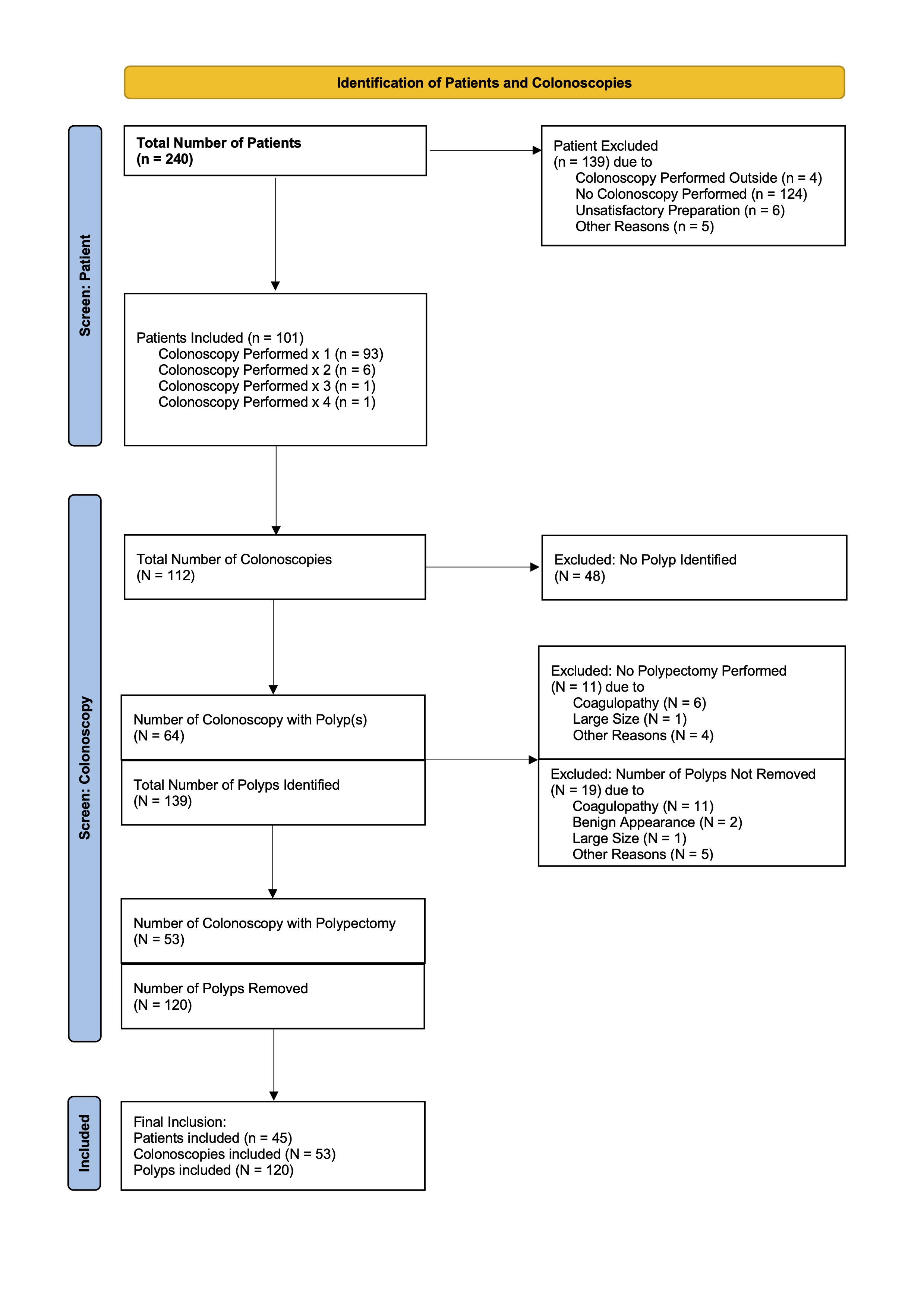
Figure: Table 1. Clinical and Endoscopic Characteristics Associated With Post-Polypectomy Bleeding in Cirrhotic Patients.
Comparison of baseline demographics, liver disease parameters, and polyp features between patients with and without post-polypectomy bleeding (PPB). Statistically significant variables (P ≤ 0.05) are noted, including elevated bilirubin, INR >1.5, lower sodium level, esophageal varices, larger polyp size, right-sided location, and hot snare use; hot snare use and elevated bilirubin remain significant on multivariate analysis.
Disclosures:
Wei Tang indicated no relevant financial relationships.
Aaron Schluger indicated no relevant financial relationships.
Anila Kumar indicated no relevant financial relationships.
Elona Poltiyelova indicated no relevant financial relationships.
Daniel Basta indicated no relevant financial relationships.
Maxwell Charlat indicated no relevant financial relationships.
Shirley Eng indicated no relevant financial relationships.
Nikki Chati indicated no relevant financial relationships.
Shireen Pais indicated no relevant financial relationships.
Wei Tang, MD1, Aaron Schluger, MD1, Anila Kumar, DO2, Elona Poltiyelova, DO1, Daniel Basta, MD3, Maxwell Charlat, MD1, Shirley Eng, MD4, Nikki Chati, MD5, Shireen Pais, MD1. P4598 - Safety and Predictors of Post-Polypectomy Bleeding in Cirrhotic Patients: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
