Tuesday Poster Session
Category: Colon
P4721 - Intentional Nail Ingestion With Cecal Impaction: Successful Colonoscopic Removal Using a Cap-Assisted Technique

Rachael Hagen, DO (she/her/hers)
University of Connecticut Health
Farmington, CT
Presenting Author(s)
1University of Connecticut Health, Farmington, CT; 2Hospital of Central Connecticut, New Britian, CT
Introduction:
Foreign body ingestion (FBI) is typically seen in patients with psychiatric disorders, intoxication, advanced age, developmental delays, or incarceration. Sharp objects pose a particular challenge due to the increased risk for perforation, necessitating extreme caution during removal. Nails are especially difficult to remove endoscopically due to their sharp, irregular shapes, which can make them hard to grasp and may require surgical intervention. Here, we present a case of FBI involving multiple nails, successfully removed using a colonoscope fitted with a distal cap.
Case Description/
Methods:
A 37-year-old female with a history of depression presented with abdominal pain after intentionally swallowing nails. This was her sixth episode of FBI in the past year. She was hemodynamically stable with unremarkable laboratory results. Abdominal examination revealed diffuse tenderness without peritoneal signs.
An abdominal x-ray showed multiple nails in the upper abdomen (Fig. 1A). CT abdomen and pelvis confirmed multiple nails in the duodenum and cecum, without pneumoperitoneum. She was managed conservatively with serial abdominal x-rays every 12 hours and continued polyethylene glycol therapy. Initial imaging showed eight nails, with progressive migration from the mid-abdomen to the right lower quadrant and ultimately clustering near the ileocecal valve (Fig. 1B-D). After four days without progression, colonoscopy was performed using a hard cap at the distal end of the scope. Removal of all eight nails from the cecum was accomplished using a snare, with care taken to hold the sharp end under the cap (Fig. 2A-B). Post-procedural inspection of the colonic mucosa revealed only minor superficial abrasions.
Discussion:
Our experience supports the use of a colonoscope cap to minimize injury of colonic mucosa during removal of sharp foreign bodies. The management of distally migrated foreign objects is not well-documented. The endoscopist should grab the sharpest edge of the object with forceps or a grasper and maintain it within the cap, cautiously withdrawing the scope. A conservative approach with serial imaging and abdominal exams remains cornerstone of initial management. However, if the object fails to pass after three days, endoscopic removal should be considered in clinically stable patients. This case highlights the feasibility and safety of colonoscopic removal in such scenarios, offering a minimally invasive alternative to surgery while effectively mitigating the risk of perforation.
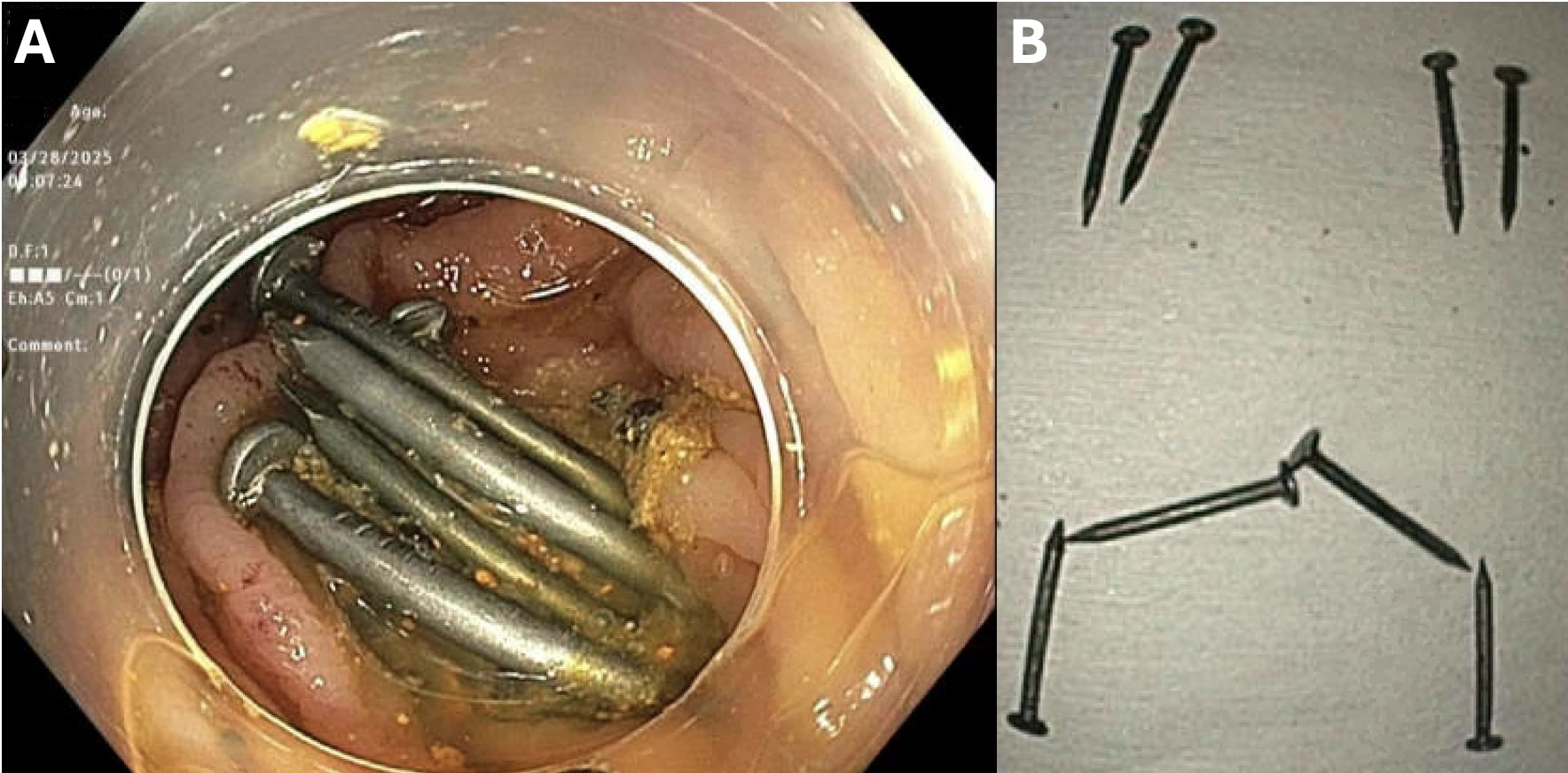
Figure: Figure 1. A. Imaging demonstrated nails within the mid-upper abdomen. B. After 24 hours, nails began progressing towards the colon. C. Nails are seen projecting over the right side at L4, the right hemi-sacrum, as well as the right iliac crest. D. Eight nails seen in a cluster at the ileocecal valve.

Figure: Figure 2. A. Eight nails were found in the cecum. B. Eight nails after successful removal.
Disclosures:
Rachael Hagen indicated no relevant financial relationships.
Aaron Kahlam indicated no relevant financial relationships.
Alexander Potashinsky indicated no relevant financial relationships.
Rachael Hagen, DO1, Aaron Kahlam, MD1, Alexander Potashinsky, MD2. P4721 - Intentional Nail Ingestion With Cecal Impaction: Successful Colonoscopic Removal Using a Cap-Assisted Technique, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
