Tuesday Poster Session
Category: Colon
P4719 - A Rare Case of a Pelvic Hematoma Following an Outpatient Colonoscopy

Sean Rangwani, MD, MBA
NewYork-Presbyterian / Weill Cornell Medical Center
New Albany, OH
Presenting Author(s)
1NewYork-Presbyterian / Weill Cornell Medical Center, New Albany, OH; 2NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medicine, New York, NY; 4NewYork-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction:
The main complications of colonoscopies are perforation and major bleeding, occurring at rates of 4 and 8 per 10,000 respectively. Bleeding is typically intraluminal; however, we present a case of a pelvic hematoma following an outpatient colonoscopy.
Case Description/
Methods:
A 58-year-old man with Stage D HFrEF due to cardiac sarcoid with an LVAD (on warfarin), hypertension, and CKD, presented for a colonoscopy for evaluation of chronic iron deficiency anemia. He was asymptomatic. His last colonoscopy, nine months prior, showed a small polyp and diverticula. He stopped warfarin five days and enoxaparin one day before the procedure. The colonoscopy showed one polyp that was removed, extensive diverticulosis, and a non-bleeding, mucosal tear in the descending colon that did not require intervention. There was resistance in the left colon due to benign-appearing, intrinsic moderate stenoses in the sigmoid and descending colon from diverticular disease. Six days later, he presented to the ED with abdominal pain and hematochezia. A CT showed a 12 cm pelvic hematoma near the rectosigmoid colon without perforation. He remained hemodynamically stable. The next day, CTA of the abdomen showed interval increase of the hematoma, new moderate to large hemoperitoneum, and two small, arterial branches feeding into the hematoma (Figure 1). He underwent embolization of two superior rectal arteries with IR, complicated by renal failure and flash pulmonary edema, requiring CRRT and intubation. He improved, was extubated, weaned off RRT, and discharged on warfarin after two weeks. He remained asymptomatic on follow-up.
Discussion:
Pelvic hematomas are a rare, but serious, potential complication of colonoscopies. This case highlights the intersection of procedural risk and patient-specific factors, chronic anticoagulation, and anatomic abnormalities such as colonic stenoses. These stenoses may have contributed to mechanical traction from the colonoscope, causing vascular injury to small rectal arteries. Extraluminal hemorrhagic complications of colonoscopy are exceedingly uncommon, but reported examples include splenic injury, mesenteric and hepatic tears, and retroperitoneal hemorrhage. This case adds to the limited literature on pelvic hematomas as a post-colonoscopy complication and underscores the importance of pre-procedural risk stratification. Early recognition through CTA and timely embolization can be lifesaving and should be considered when managing atypical post-procedural bleeding.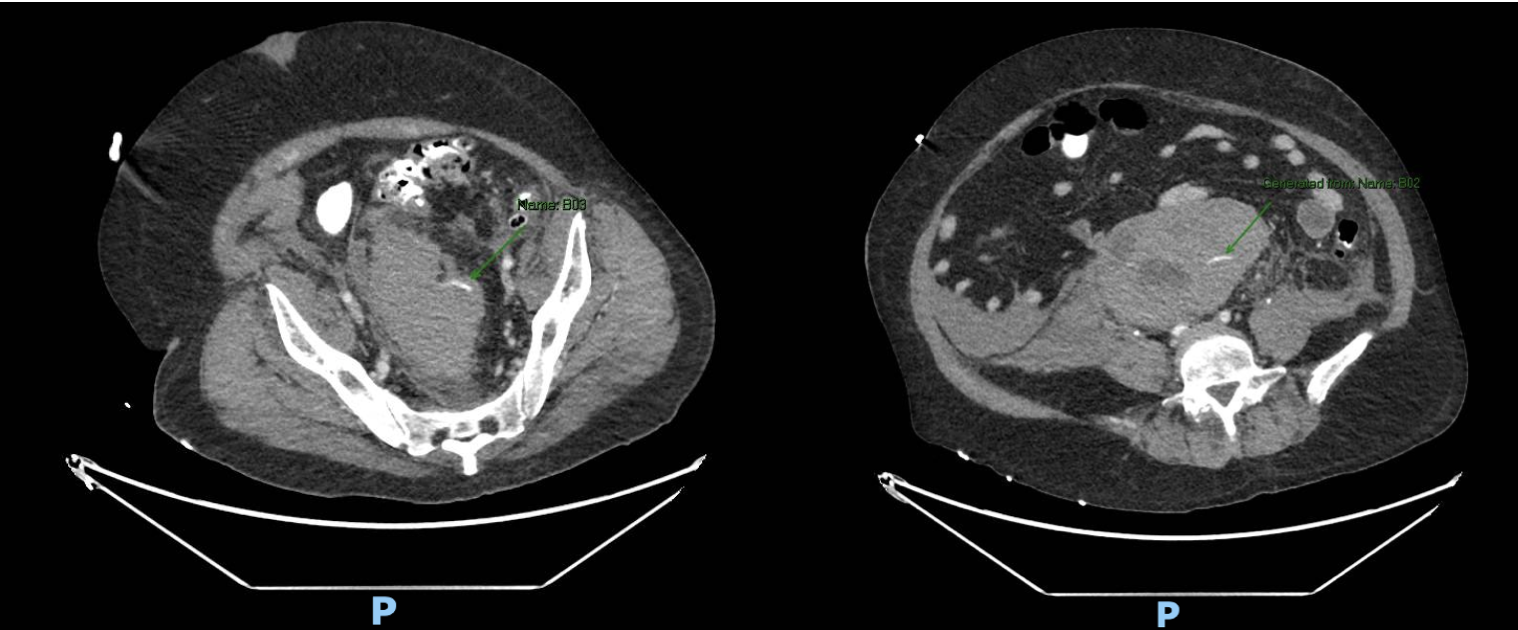
Figure: Figure 1: Two Rectal Artery Branches Feeding into the Pelvic Hematoma
Disclosures:
Sean Rangwani indicated no relevant financial relationships.
Deirdre Reidy indicated no relevant financial relationships.
Lauren Callans indicated no relevant financial relationships.
Lillian Zhang indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Adeyinka Adejumo indicated no relevant financial relationships.
David Wan: Medtronic – Data Monitoring Committee.
David Carr-Locke: Boston Scientific – Consultant. Steris Corporation – Royalties.
Evan Grossman indicated no relevant financial relationships.
Sean Rangwani, MD, MBA1, Deirdre Reidy, MD2, Lauren Callans, MD3, Lillian F. Zhang, MD, PhD2, Emily S. Smith, MD2, Adeyinka Adejumo, MD3, David Wan, MD4, David Carr-Locke, MD, FACG3, Evan Grossman, MD2. P4719 - A Rare Case of a Pelvic Hematoma Following an Outpatient Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
