Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4787 - Tracking Competence in Real Time: A Fellow-Reported Study of Colonoscopy Success Factors
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joshua Musalia, MD (he/him/his)
University of Cincinnati College of Medicine
Cincinnati, OH
Presenting Author(s)
Joshua Musalia, MD1, John Musalia, PhD2, Patrick J. Carey, MD3, Emad Aljahdaly, MD, MBBS, ABIM4, Moamen Gabr, MD, MSc3
1University of Cincinnati College of Medicine, Cincinnati, OH; 2Western Kentucky University, Bowling Green, KY; 3University of Cincinnati, Cincinnati, OH; 4king abdulaziz University, Jeddah, Makkah, Saudi Arabia
Introduction: Assessing trainee performance in endoscopy remains challenging due to limited data on real-time involvement and procedural skill. Existing tools like ProVation document performed interventions but often fail to reflect a fellow's autonomy or actual contribution. Without standardized, fellow-specific metrics, programs struggle to deliver targeted feedback and improve training outcomes. To address this, we developed a novel, fellow-led data collection system that allowed trainees to record procedural details directly. This study analyzes outcomes from one institution utilizing this method to identify predictors of colonoscopy success over a single academic year (2023 to 2024).
Methods: We analyzed 341 colonoscopies recorded by fellows across three levels of training (Year 1 to 3). Fellows documented their training year, degree of autonomy (50% vs. 100%), and perceived case difficulty (0 to 100 scale). The primary outcome was successful ileal intubation. Logistic regression was used to assess predictors of success.
Results: 91% (n = 309) of colonoscopies were successful. Most procedures were performed by Year 2 (53%) and Year 3 (40%) fellows; Year 1 fellows performed 6.5%. Full autonomy was reported in 95% of cases. Perceived difficulty was overall low (mean = 1.3; SD = 5.1). Autonomy was significantly associated with success; fellows with 100% autonomy had over five times the odds of success compared to those with 50% autonomy (OR = 5.54; 95% CI: 0.98 to 26.6; p = 0.036). Training level and perceived difficulty were not statistically significant predictors.
Discussion: Autonomy was the only significant predictor of successful ileal intubation. However, this may reflect supervision bias, as fellows likely received full autonomy only when deemed competent. While Year 2 fellows appeared to have lower odds of success, the small number of Year 1 cases limits meaningful comparison and suggests possible confounding. Despite these limitations, this fellow-led data tool provides valuable insight into procedural competence and supports the use of real-time trainee-reported metrics in gastroenterology education.
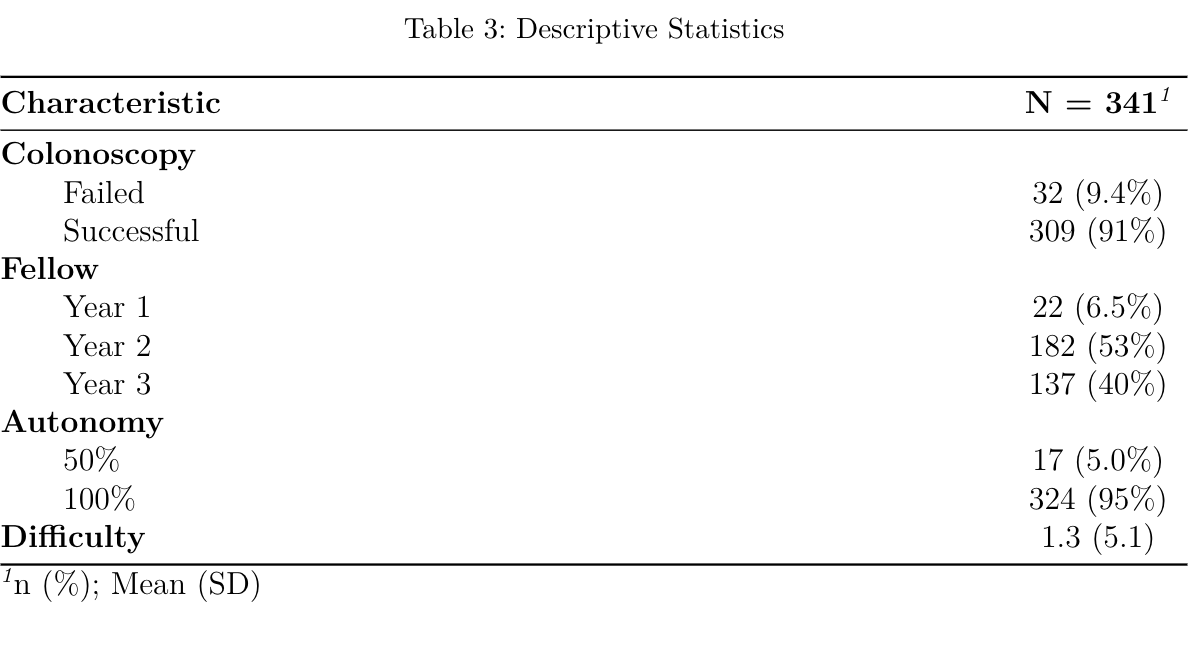
Figure: Descriptive statistics of our study
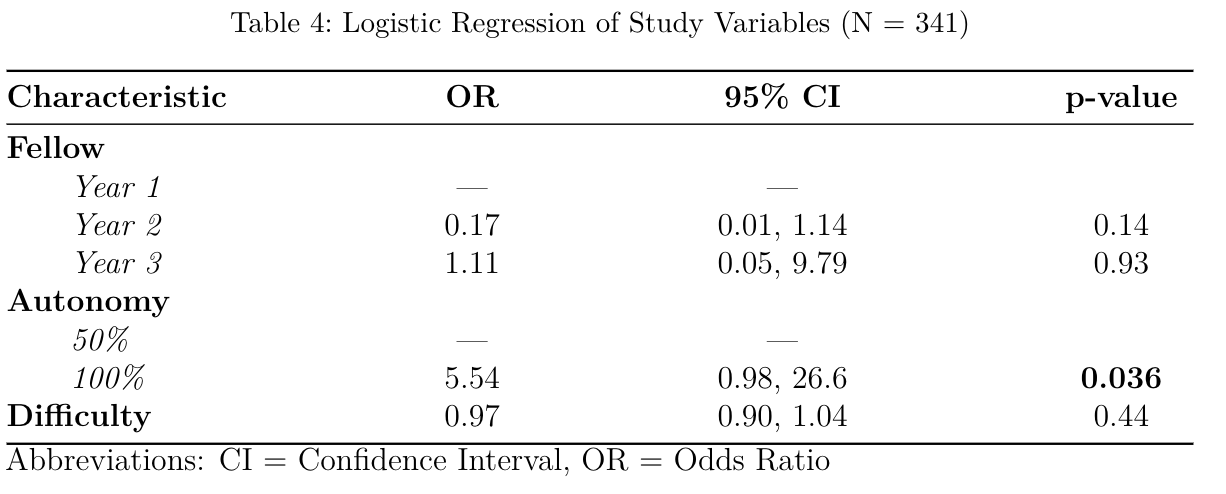
Figure: Results of a logistic regression
Disclosures:
Joshua Musalia indicated no relevant financial relationships.
John Musalia indicated no relevant financial relationships.
Patrick Carey indicated no relevant financial relationships.
Emad Aljahdaly indicated no relevant financial relationships.
Moamen Gabr indicated no relevant financial relationships.
Joshua Musalia, MD1, John Musalia, PhD2, Patrick J. Carey, MD3, Emad Aljahdaly, MD, MBBS, ABIM4, Moamen Gabr, MD, MSc3. P4787 - Tracking Competence in Real Time: A Fellow-Reported Study of Colonoscopy Success Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Cincinnati College of Medicine, Cincinnati, OH; 2Western Kentucky University, Bowling Green, KY; 3University of Cincinnati, Cincinnati, OH; 4king abdulaziz University, Jeddah, Makkah, Saudi Arabia
Introduction: Assessing trainee performance in endoscopy remains challenging due to limited data on real-time involvement and procedural skill. Existing tools like ProVation document performed interventions but often fail to reflect a fellow's autonomy or actual contribution. Without standardized, fellow-specific metrics, programs struggle to deliver targeted feedback and improve training outcomes. To address this, we developed a novel, fellow-led data collection system that allowed trainees to record procedural details directly. This study analyzes outcomes from one institution utilizing this method to identify predictors of colonoscopy success over a single academic year (2023 to 2024).
Methods: We analyzed 341 colonoscopies recorded by fellows across three levels of training (Year 1 to 3). Fellows documented their training year, degree of autonomy (50% vs. 100%), and perceived case difficulty (0 to 100 scale). The primary outcome was successful ileal intubation. Logistic regression was used to assess predictors of success.
Results: 91% (n = 309) of colonoscopies were successful. Most procedures were performed by Year 2 (53%) and Year 3 (40%) fellows; Year 1 fellows performed 6.5%. Full autonomy was reported in 95% of cases. Perceived difficulty was overall low (mean = 1.3; SD = 5.1). Autonomy was significantly associated with success; fellows with 100% autonomy had over five times the odds of success compared to those with 50% autonomy (OR = 5.54; 95% CI: 0.98 to 26.6; p = 0.036). Training level and perceived difficulty were not statistically significant predictors.
Discussion: Autonomy was the only significant predictor of successful ileal intubation. However, this may reflect supervision bias, as fellows likely received full autonomy only when deemed competent. While Year 2 fellows appeared to have lower odds of success, the small number of Year 1 cases limits meaningful comparison and suggests possible confounding. Despite these limitations, this fellow-led data tool provides valuable insight into procedural competence and supports the use of real-time trainee-reported metrics in gastroenterology education.
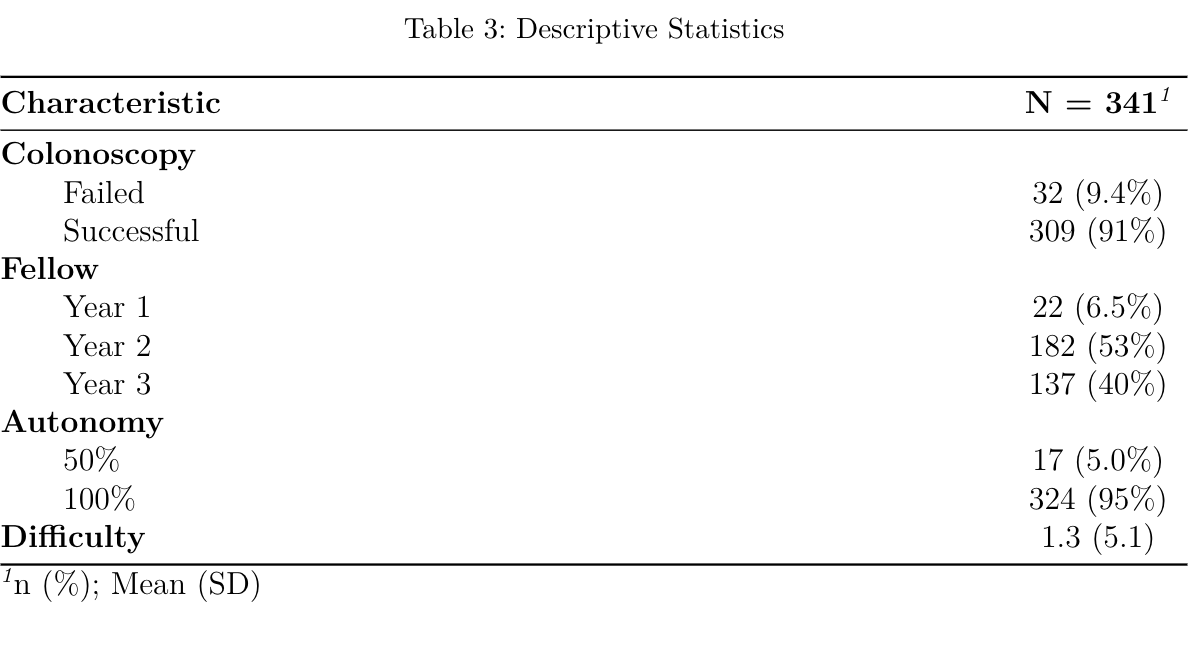
Figure: Descriptive statistics of our study
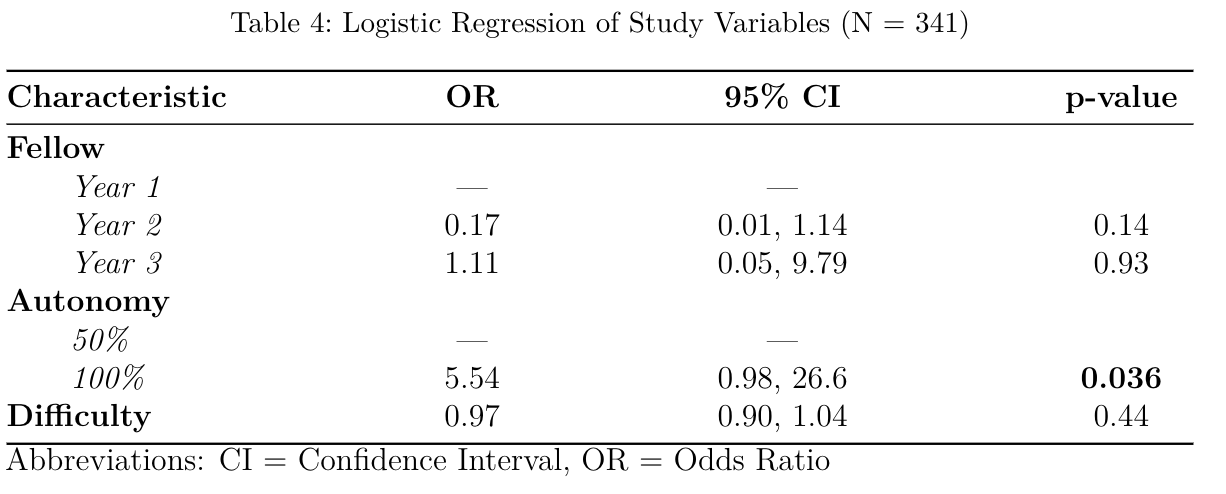
Figure: Results of a logistic regression
Disclosures:
Joshua Musalia indicated no relevant financial relationships.
John Musalia indicated no relevant financial relationships.
Patrick Carey indicated no relevant financial relationships.
Emad Aljahdaly indicated no relevant financial relationships.
Moamen Gabr indicated no relevant financial relationships.
Joshua Musalia, MD1, John Musalia, PhD2, Patrick J. Carey, MD3, Emad Aljahdaly, MD, MBBS, ABIM4, Moamen Gabr, MD, MSc3. P4787 - Tracking Competence in Real Time: A Fellow-Reported Study of Colonoscopy Success Factors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
