Tuesday Poster Session
Category: Esophagus
P4885 - Metabolic Syndrome as Risk Factor for Esophageal Cancer
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Julton Tomanguillo Chumbe, MD
Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Julton Tomanguillo, MD, Jennifer Collins, PhD, Nisar Amin, MD, Ebubekir Daglilar, MD, Harleen Chela, MD
Charleston Area Medical Center, Charleston, WV
Introduction: Metabolic syndrome (MetS) is associated with an increased risk of malignancy, representing a significant health burden. This study aims to assess whether MetS significantly increases the risk of esophageal cancer (EC) and whether this relationship varies across sex, age, race, and ethnicity. It further investigates whether the association is amplified when Barrett’s esophagus(BE) is included as part of a combined endpoint.
Methods: This retrospective cohort study utilized the TriNetX Analytics Platform to analyze patients aged ≥18 years to look at the annual incidence proportions for EC from 2018-2024. Poisson regression models with log-population offsets were used to estimate adjusted risk ratios (RRs). Models included year, race, sex, age group, ethnicity, and interaction terms to evaluate the differences in the effect of MetS across subgroups. A secondary analysis evaluated if patients with MetS and BE increase further the risk of EC.
Results: The analysis included a total of 109,877,044 patients, with 10,327,978 having MetS and 99,549,066 without. MetS was associated with a significantly higher incidence of EC (RR: 2.84, p < 0.0001). When BE was included as a combined endpoint, the risk associated with MetS further increased (RR: 5.23, p < 0.0001). EC increased significantly over time, with a steeper rise among MetS patients (p < 0.0001). The MetS associated risk was higher across all sex and age groups, peaking in patients aged 65-69 (RR: 9.88, p < 0.0001). Males and White patients had the highest baseline prevalence. Interaction models revealed that the effect of MetS was weaker among Asian (RR: 0.70), Black (RR: 0.78), and other race groups (RR: 0.72) compared to White patients. Hispanic patients had a significantly lower baseline incidence (RR: 0.053), but the relative effect of MetS did not differ significantly between Hispanic and Non-Hispanic patients (p = 0.789) (Figure A and Table 1).
Discussion: MetS significantly increases the risk of EC, more than doubling its incidence. Furthermore, the presence of BE amplifies this association. EC incidence demonstrates a significant increase over time, with a steeper rise observed among patients with metabolic syndrome.
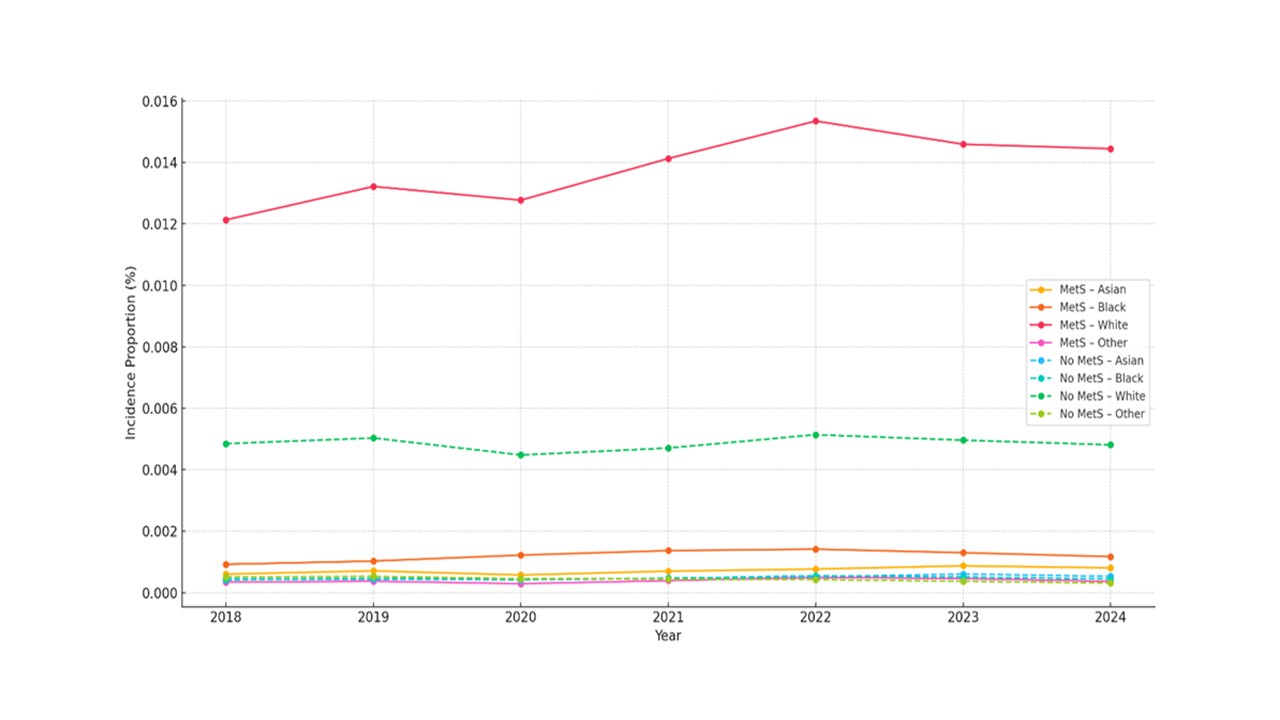
Figure: Figure A: Incidence Proportion of Esophageal Cancer by Race and Group in Patients with Metabolic Syndrome
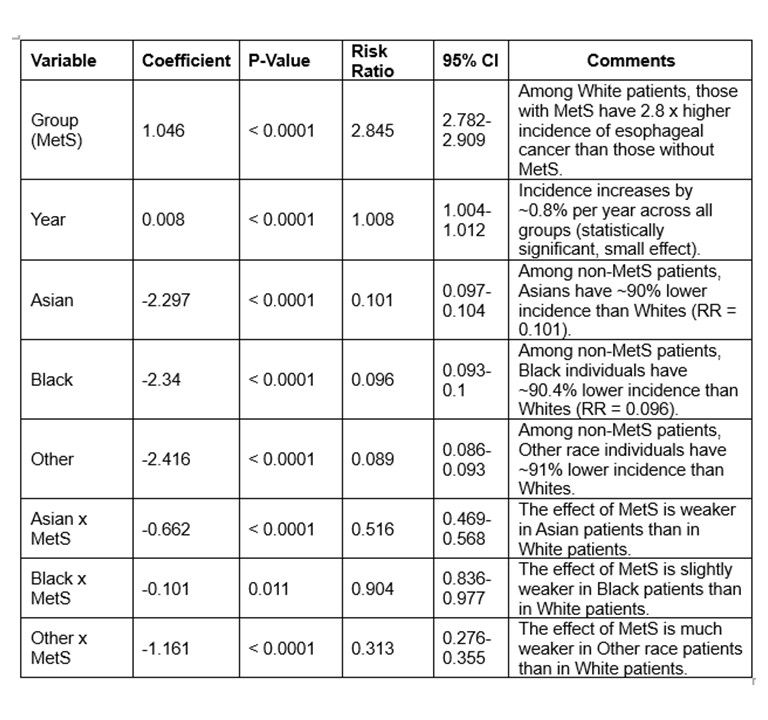
Figure: Table 1: Risk Ratio of Esophageal Cancer by Group, Year, and Race among Patients with Metabolic Syndrome
Disclosures:
Julton Tomanguillo indicated no relevant financial relationships.
Jennifer Collins indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Julton Tomanguillo, MD, Jennifer Collins, PhD, Nisar Amin, MD, Ebubekir Daglilar, MD, Harleen Chela, MD. P4885 - Metabolic Syndrome as Risk Factor for Esophageal Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Charleston Area Medical Center, Charleston, WV
Introduction: Metabolic syndrome (MetS) is associated with an increased risk of malignancy, representing a significant health burden. This study aims to assess whether MetS significantly increases the risk of esophageal cancer (EC) and whether this relationship varies across sex, age, race, and ethnicity. It further investigates whether the association is amplified when Barrett’s esophagus(BE) is included as part of a combined endpoint.
Methods: This retrospective cohort study utilized the TriNetX Analytics Platform to analyze patients aged ≥18 years to look at the annual incidence proportions for EC from 2018-2024. Poisson regression models with log-population offsets were used to estimate adjusted risk ratios (RRs). Models included year, race, sex, age group, ethnicity, and interaction terms to evaluate the differences in the effect of MetS across subgroups. A secondary analysis evaluated if patients with MetS and BE increase further the risk of EC.
Results: The analysis included a total of 109,877,044 patients, with 10,327,978 having MetS and 99,549,066 without. MetS was associated with a significantly higher incidence of EC (RR: 2.84, p < 0.0001). When BE was included as a combined endpoint, the risk associated with MetS further increased (RR: 5.23, p < 0.0001). EC increased significantly over time, with a steeper rise among MetS patients (p < 0.0001). The MetS associated risk was higher across all sex and age groups, peaking in patients aged 65-69 (RR: 9.88, p < 0.0001). Males and White patients had the highest baseline prevalence. Interaction models revealed that the effect of MetS was weaker among Asian (RR: 0.70), Black (RR: 0.78), and other race groups (RR: 0.72) compared to White patients. Hispanic patients had a significantly lower baseline incidence (RR: 0.053), but the relative effect of MetS did not differ significantly between Hispanic and Non-Hispanic patients (p = 0.789) (Figure A and Table 1).
Discussion: MetS significantly increases the risk of EC, more than doubling its incidence. Furthermore, the presence of BE amplifies this association. EC incidence demonstrates a significant increase over time, with a steeper rise observed among patients with metabolic syndrome.
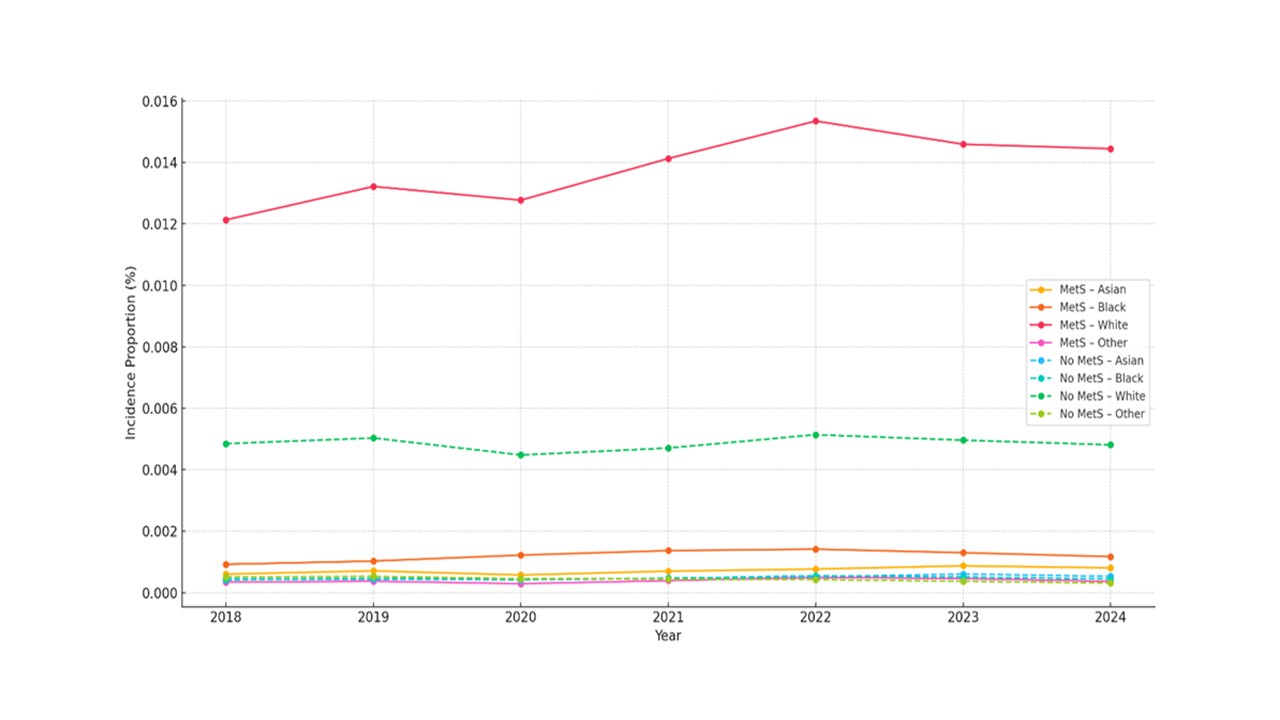
Figure: Figure A: Incidence Proportion of Esophageal Cancer by Race and Group in Patients with Metabolic Syndrome
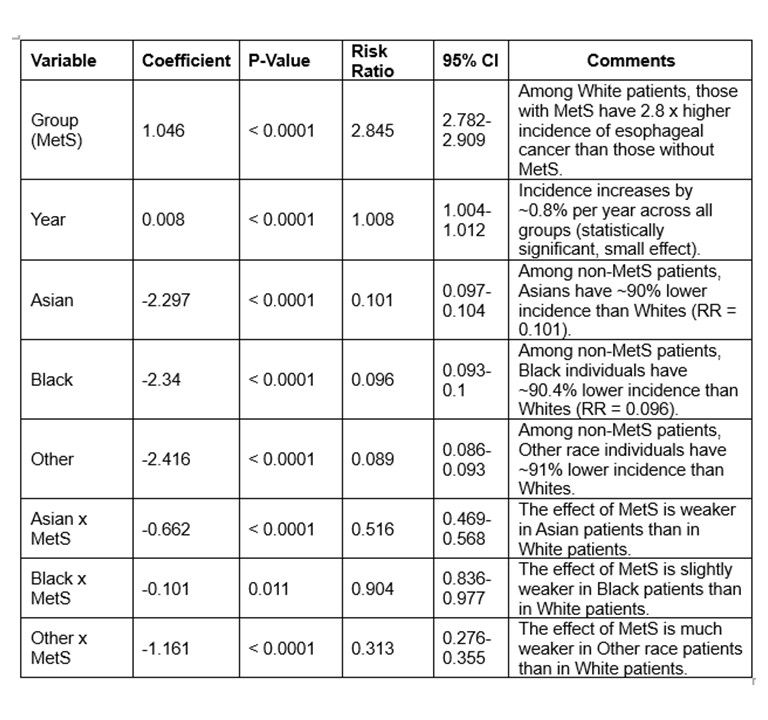
Figure: Table 1: Risk Ratio of Esophageal Cancer by Group, Year, and Race among Patients with Metabolic Syndrome
Disclosures:
Julton Tomanguillo indicated no relevant financial relationships.
Jennifer Collins indicated no relevant financial relationships.
Nisar Amin indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Julton Tomanguillo, MD, Jennifer Collins, PhD, Nisar Amin, MD, Ebubekir Daglilar, MD, Harleen Chela, MD. P4885 - Metabolic Syndrome as Risk Factor for Esophageal Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
