Tuesday Poster Session
Category: Esophagus
P4882 - Prevalence of Dysphagia After Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy: A National Propensity Score Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Sherif Saleh, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Sherif Saleh, MD1, Michael Kurin, MD1, Mayada Ismail, MD2, Raj Shah, MD3, Steve D'Souza, MD1, Katarina Greer, MD4
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Louis Stokes Cleveland VA Medical Center, Cleveland, OH
Introduction: Bariatric surgery is increasingly performed, with Laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (RYGB) being the most common procedures. The comparative incidence of dysphagia after LSG and RYGB is not well-studied. We aimed to determine the incidence of dysphagia following LSG and RYGB using a large database.
Methods: Utilizing the US Collaborative Network within TriNetX, which brings together data from 66 health care organizations from the United States, we conducted a population-based cohort study to examine the incidence of dysphagia after RYGB and LSG versus patients with morbid obesity who did not undergo bariatric surgery from 2014 to 2024. The database uses ICD codes for diagnoses and CPT codes for procedures. A 1:1 propensity score matching was performed to adjust for OSA, PPI use, GERD, age, tobacco and alcohol use. The odds of developing dysphagia within 1 month, 1-3 months, 3-6 months, 6-12 months, 1-3 years, 3-5 years and 5-10 years after bariatric surgery was also examined. Odds ratios (OR) with 95% confidence intervals (CI) were calculated.
Results: A total of 2,761,563 patients with morbid obesity were included in the analysis. Of these, 2,616,988 did not undergo surgery (No Surgery group), and 223,415 (8.53%) from that group developed dysphagia. 29,242 underwent RYGB (RYGB group), of whom 4,277 (14.6%) developed dysphagia (RYGB vs. No Surgery OR= 2.48, 95% CI [2.24- 2.61], p< 0.01). 57,013 patients underwent LSG (LSG group), of whom 4,820 (8.67%) developed dysphagia (LSG vs. No surgery OR=1.5; 95% CI [1.42-1.62], p< 0.01). Demographics and characteristics of all groups are shown in Table 1. In both surgical groups, the incidence of dysphagia was highest within 30 days after the surgery with 30% of patients in the RYGB developing dysphagia and 24.3% in the LSG developing dysphagia (Figure 1). In a propensity scored analysis compared to patients with morbid obesity that did not undergo surgery, RYGB (OR=1.57; 95% CI [1.48-1.67], p< 0.01) and LSG (OR=1.16, 95% CI [1.10-1.12], p< 0.01) were both independent risk factors for dysphagia.
Discussion: Based on a large national database the incidence of dysphagia is increased after both LSG and RYGB compared to patients with morbid obesity who did not undergo surgery, though the increased incidence is more pronounced after RYGB. Dysphagia mostly occurred within the first 30 days postoperatively in both RYGB and LSG groups. Further studies are needed to determine the etiologies of dysphagia.
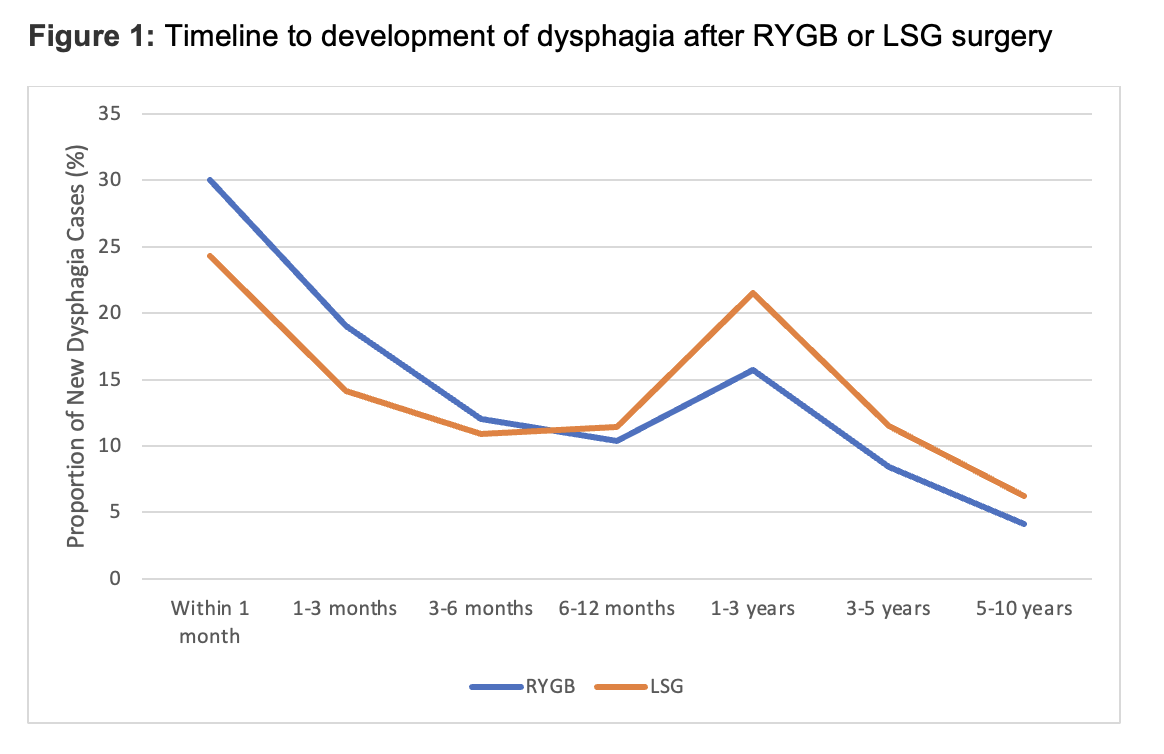
Figure: Figure 1: Timeline to development of dysphagia after RYGB or LSG surgery
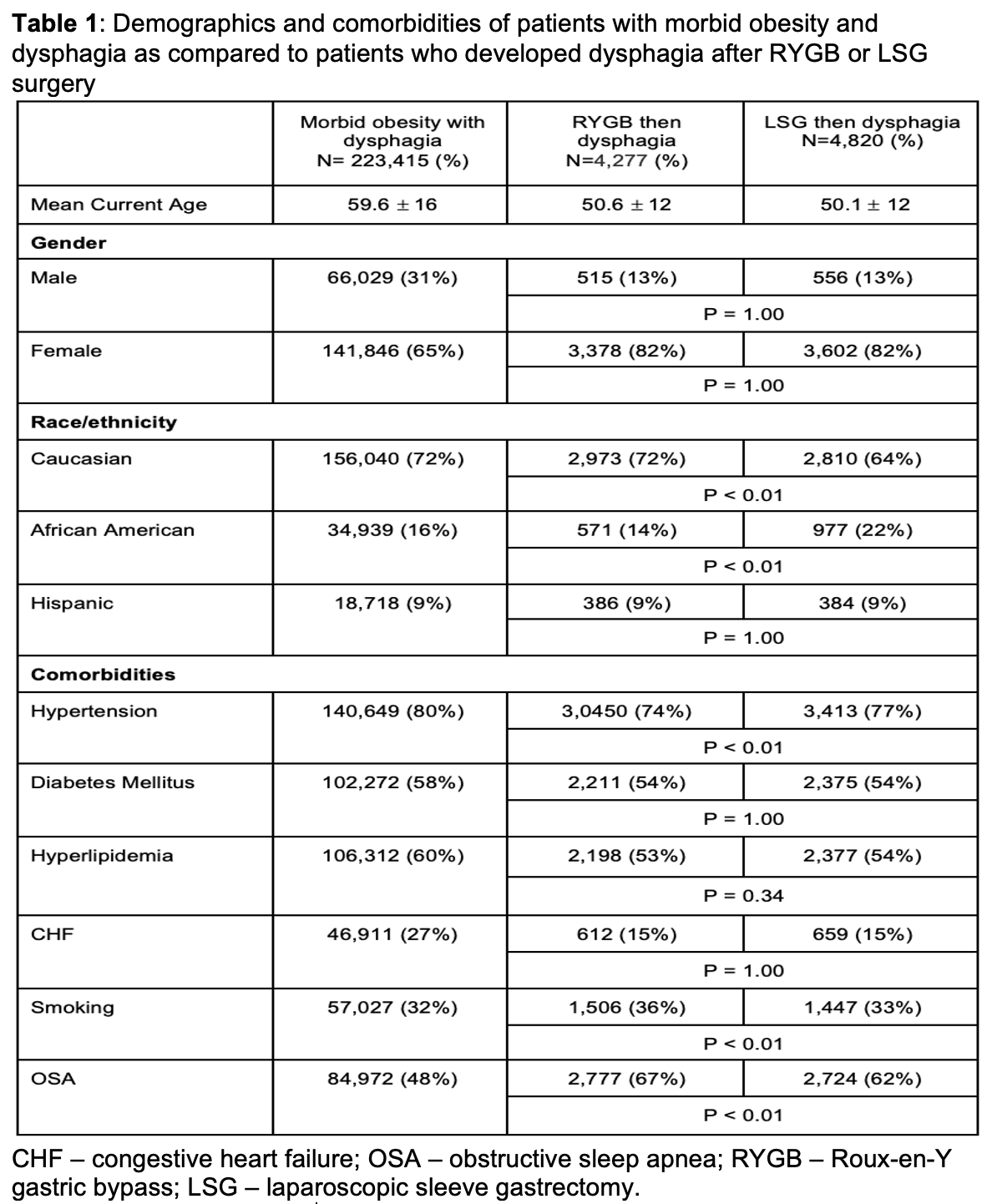
Figure: Table 1: Demographics and comorbidities of patients with morbid obesity and dysphagia as compared to patients who developed dysphagia after RYGB or LSG surgery
Disclosures:
Sherif Saleh indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Steve D'Souza indicated no relevant financial relationships.
Katarina Greer indicated no relevant financial relationships.
Sherif Saleh, MD1, Michael Kurin, MD1, Mayada Ismail, MD2, Raj Shah, MD3, Steve D'Souza, MD1, Katarina Greer, MD4. P4882 - Prevalence of Dysphagia After Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy: A National Propensity Score Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3The Ohio State University Wexner Medical Center, Columbus, OH; 4Louis Stokes Cleveland VA Medical Center, Cleveland, OH
Introduction: Bariatric surgery is increasingly performed, with Laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (RYGB) being the most common procedures. The comparative incidence of dysphagia after LSG and RYGB is not well-studied. We aimed to determine the incidence of dysphagia following LSG and RYGB using a large database.
Methods: Utilizing the US Collaborative Network within TriNetX, which brings together data from 66 health care organizations from the United States, we conducted a population-based cohort study to examine the incidence of dysphagia after RYGB and LSG versus patients with morbid obesity who did not undergo bariatric surgery from 2014 to 2024. The database uses ICD codes for diagnoses and CPT codes for procedures. A 1:1 propensity score matching was performed to adjust for OSA, PPI use, GERD, age, tobacco and alcohol use. The odds of developing dysphagia within 1 month, 1-3 months, 3-6 months, 6-12 months, 1-3 years, 3-5 years and 5-10 years after bariatric surgery was also examined. Odds ratios (OR) with 95% confidence intervals (CI) were calculated.
Results: A total of 2,761,563 patients with morbid obesity were included in the analysis. Of these, 2,616,988 did not undergo surgery (No Surgery group), and 223,415 (8.53%) from that group developed dysphagia. 29,242 underwent RYGB (RYGB group), of whom 4,277 (14.6%) developed dysphagia (RYGB vs. No Surgery OR= 2.48, 95% CI [2.24- 2.61], p< 0.01). 57,013 patients underwent LSG (LSG group), of whom 4,820 (8.67%) developed dysphagia (LSG vs. No surgery OR=1.5; 95% CI [1.42-1.62], p< 0.01). Demographics and characteristics of all groups are shown in Table 1. In both surgical groups, the incidence of dysphagia was highest within 30 days after the surgery with 30% of patients in the RYGB developing dysphagia and 24.3% in the LSG developing dysphagia (Figure 1). In a propensity scored analysis compared to patients with morbid obesity that did not undergo surgery, RYGB (OR=1.57; 95% CI [1.48-1.67], p< 0.01) and LSG (OR=1.16, 95% CI [1.10-1.12], p< 0.01) were both independent risk factors for dysphagia.
Discussion: Based on a large national database the incidence of dysphagia is increased after both LSG and RYGB compared to patients with morbid obesity who did not undergo surgery, though the increased incidence is more pronounced after RYGB. Dysphagia mostly occurred within the first 30 days postoperatively in both RYGB and LSG groups. Further studies are needed to determine the etiologies of dysphagia.
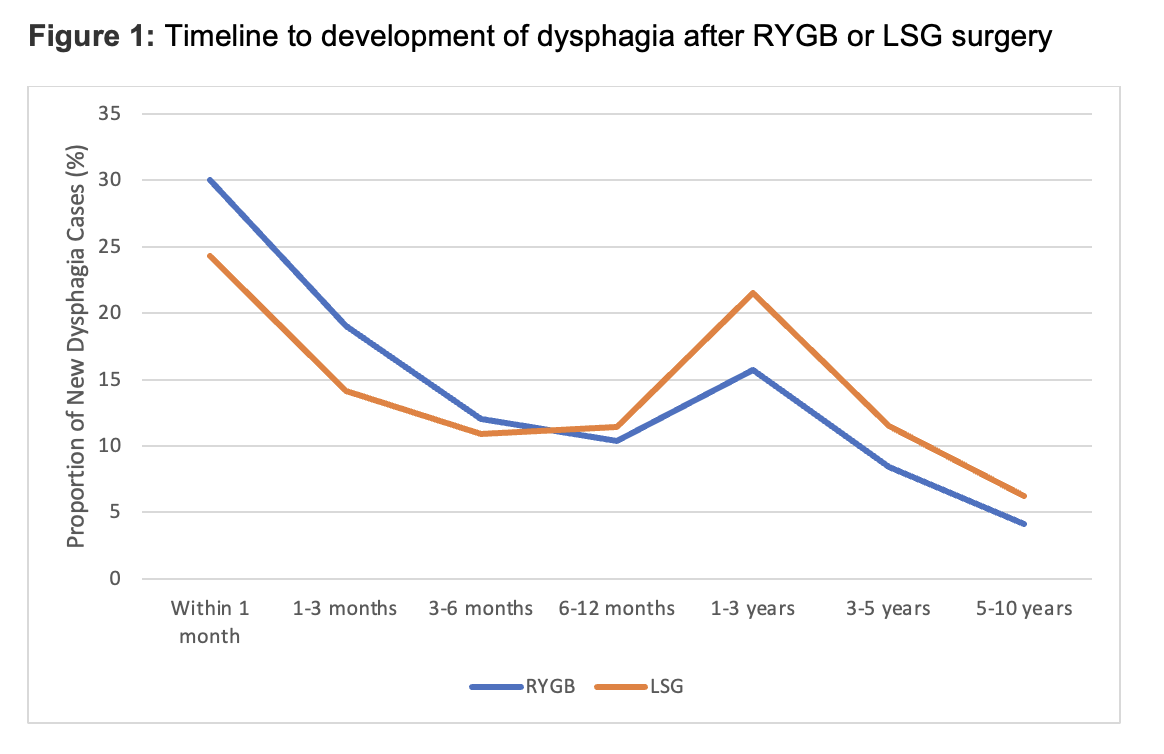
Figure: Figure 1: Timeline to development of dysphagia after RYGB or LSG surgery
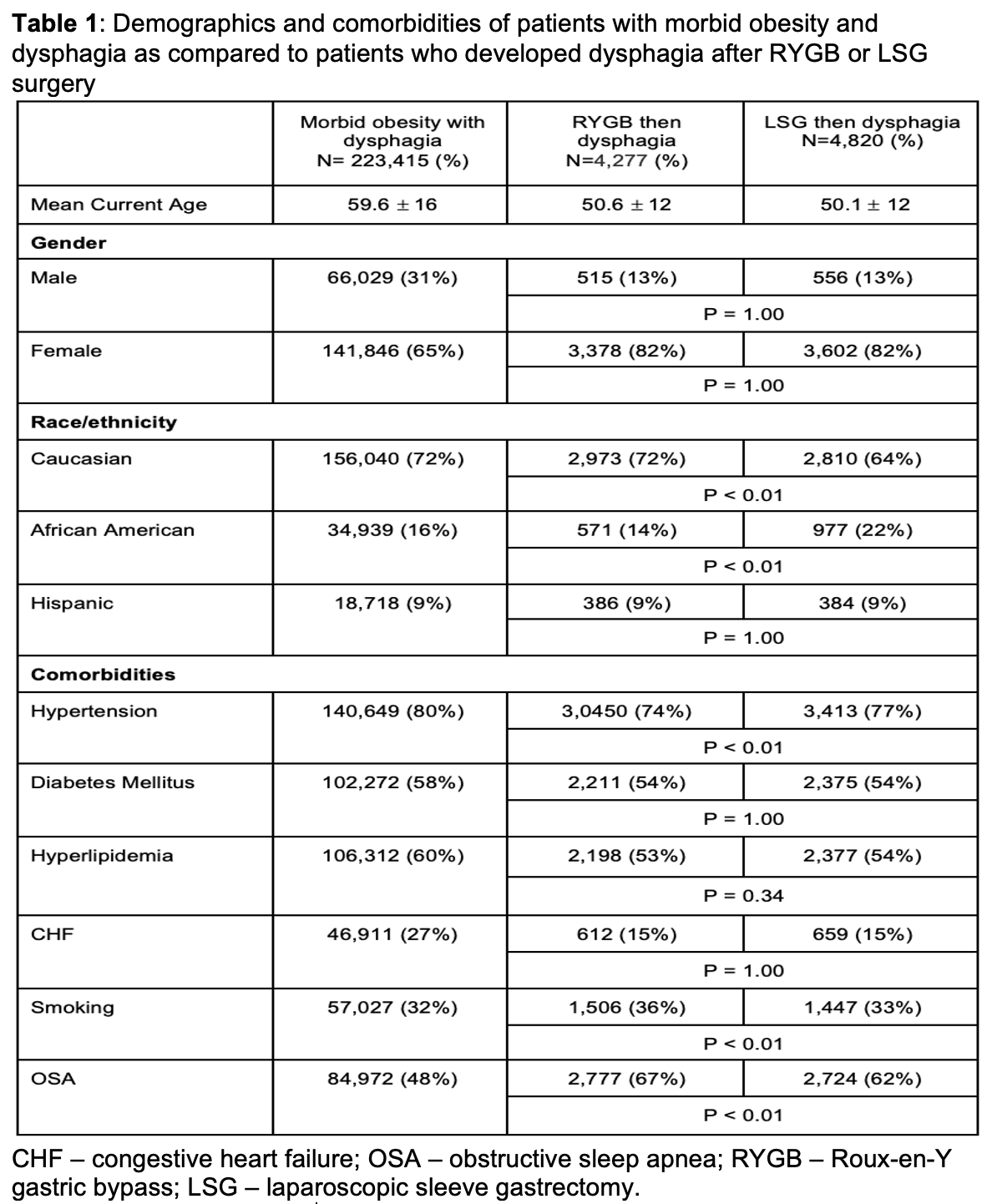
Figure: Table 1: Demographics and comorbidities of patients with morbid obesity and dysphagia as compared to patients who developed dysphagia after RYGB or LSG surgery
Disclosures:
Sherif Saleh indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Steve D'Souza indicated no relevant financial relationships.
Katarina Greer indicated no relevant financial relationships.
Sherif Saleh, MD1, Michael Kurin, MD1, Mayada Ismail, MD2, Raj Shah, MD3, Steve D'Souza, MD1, Katarina Greer, MD4. P4882 - Prevalence of Dysphagia After Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy: A National Propensity Score Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
