Tuesday Poster Session
Category: Esophagus
P4964 - Beyond the Mucosa: When Candida Breaches the Esophageal Barrier -- A Rare Case of Transmural Fungal Invasion Leading to Perforation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Raahi Patel, DO
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Raahi Patel, DO, Varshita Goduguchinta, DO, Ahmed Al Mubaid, DO, Erick Tiemens, DO, Muhammad Nazir, MD, Keval Patel, MD, Jay Cowen, MD
Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Esophageal perforations are most commonly iatrogenic due to medical procedures, followed by spontaneous and traumatic perforations. Transmural fungal infections, on the other hand, are extremely rare causes of esophageal perforations. We present a case of a transmural Candida infection of the esophagus causing perforation despite adequate treatment.
Case Description/
Methods: A 61-year-old male with a recent history of Candida esophagitis s/p fluconazole therapy presented with worsening weakness in bilateral lower extremities and an episode of coffee-ground emesis. He was admitted to the ICU due to severe lactic acidosis and acute hypoxic respiratory failure requiring emergent intubation. Chest X-ray showed left-sided hydropneumothorax, for which a surgical chest tube was placed. Initial computed tomography (CT) scan of the chest showed severe thoracic esophageal wall thickening and possible esophagitis versus esophageal mass. Pleural effusion studies subsequently revealed benign squamous findings from the esophagus with aggregates of food particles along with pleural fluid cultures growing Streptococcus salivarius. The gastroenterology service was consulted due to suspicion of an underlying esophageal-pleural fistula. Repeat CT scan of the chest with oral contrast was obtained instead and showed findings concerning a broncho-esophageal fistula from the lateral left distal wall of the esophagus into the postero-lateral left segmental bronchus. The patient was transferred to a tertiary center for a higher level of care, where he underwent an esophagogastroduodenoscopy with Lu's approach for video-assisted thoracoscopic surgical (LVATS) decortication, confirming an esophageal perforation. Patient progressed well throughout his stay and was discharged in a stable condition.
Discussion: Esophageal perforation is a rare but life-threatening condition, with a mortality rate ranging from 10–40%, depending on the cause and timing of intervention. While Candida esophagitis occurs in up to 5% of hospitalized or immunocompromised patients, progression to transmural infection and perforation is exceedingly rare. Most patients respond to antifungal therapy, and only a few cases of Candida-related esophageal perforation have been reported in the literature. In this case, despite fluconazole treatment, the patient developed a perforation, confirmed by imaging, pleural cultures, and EGD. This highlights the need for high clinical suspicion and early intervention in deteriorating patients with fungal esophagitis.
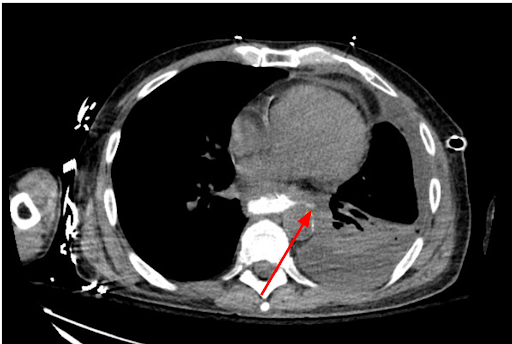
Figure: A broncho-esophageal fistula seen on initial CT imaging that later advanced to esophageal perforation
Disclosures:
Raahi Patel indicated no relevant financial relationships.
Varshita Goduguchinta indicated no relevant financial relationships.
Ahmed Al Mubaid indicated no relevant financial relationships.
Erick Tiemens indicated no relevant financial relationships.
Muhammad Nazir indicated no relevant financial relationships.
Keval Patel indicated no relevant financial relationships.
Jay Cowen indicated no relevant financial relationships.
Raahi Patel, DO, Varshita Goduguchinta, DO, Ahmed Al Mubaid, DO, Erick Tiemens, DO, Muhammad Nazir, MD, Keval Patel, MD, Jay Cowen, MD. P4964 - Beyond the Mucosa: When Candida Breaches the Esophageal Barrier -- A Rare Case of Transmural Fungal Invasion Leading to Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Esophageal perforations are most commonly iatrogenic due to medical procedures, followed by spontaneous and traumatic perforations. Transmural fungal infections, on the other hand, are extremely rare causes of esophageal perforations. We present a case of a transmural Candida infection of the esophagus causing perforation despite adequate treatment.
Case Description/
Methods: A 61-year-old male with a recent history of Candida esophagitis s/p fluconazole therapy presented with worsening weakness in bilateral lower extremities and an episode of coffee-ground emesis. He was admitted to the ICU due to severe lactic acidosis and acute hypoxic respiratory failure requiring emergent intubation. Chest X-ray showed left-sided hydropneumothorax, for which a surgical chest tube was placed. Initial computed tomography (CT) scan of the chest showed severe thoracic esophageal wall thickening and possible esophagitis versus esophageal mass. Pleural effusion studies subsequently revealed benign squamous findings from the esophagus with aggregates of food particles along with pleural fluid cultures growing Streptococcus salivarius. The gastroenterology service was consulted due to suspicion of an underlying esophageal-pleural fistula. Repeat CT scan of the chest with oral contrast was obtained instead and showed findings concerning a broncho-esophageal fistula from the lateral left distal wall of the esophagus into the postero-lateral left segmental bronchus. The patient was transferred to a tertiary center for a higher level of care, where he underwent an esophagogastroduodenoscopy with Lu's approach for video-assisted thoracoscopic surgical (LVATS) decortication, confirming an esophageal perforation. Patient progressed well throughout his stay and was discharged in a stable condition.
Discussion: Esophageal perforation is a rare but life-threatening condition, with a mortality rate ranging from 10–40%, depending on the cause and timing of intervention. While Candida esophagitis occurs in up to 5% of hospitalized or immunocompromised patients, progression to transmural infection and perforation is exceedingly rare. Most patients respond to antifungal therapy, and only a few cases of Candida-related esophageal perforation have been reported in the literature. In this case, despite fluconazole treatment, the patient developed a perforation, confirmed by imaging, pleural cultures, and EGD. This highlights the need for high clinical suspicion and early intervention in deteriorating patients with fungal esophagitis.
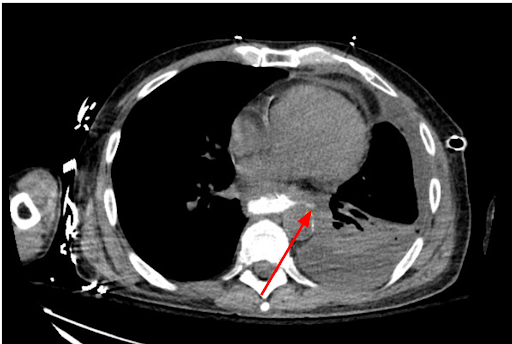
Figure: A broncho-esophageal fistula seen on initial CT imaging that later advanced to esophageal perforation
Disclosures:
Raahi Patel indicated no relevant financial relationships.
Varshita Goduguchinta indicated no relevant financial relationships.
Ahmed Al Mubaid indicated no relevant financial relationships.
Erick Tiemens indicated no relevant financial relationships.
Muhammad Nazir indicated no relevant financial relationships.
Keval Patel indicated no relevant financial relationships.
Jay Cowen indicated no relevant financial relationships.
Raahi Patel, DO, Varshita Goduguchinta, DO, Ahmed Al Mubaid, DO, Erick Tiemens, DO, Muhammad Nazir, MD, Keval Patel, MD, Jay Cowen, MD. P4964 - Beyond the Mucosa: When Candida Breaches the Esophageal Barrier -- A Rare Case of Transmural Fungal Invasion Leading to Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
