Tuesday Poster Session
Category: Esophagus
P4961 - An Unusual Presentation for Lichen Esophagitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jerry H. Rose, MD (he/him/his)
University of Maryland Medical System
Baltimore, CA
Presenting Author(s)
Jerry H. Rose, MD1, Andrew Leopold, MD2, William Twaddell, MD2, Abdulhameed M. Al-Sabban, MBBS3
1University of Maryland Medical System, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD; 3UNIVERSITY OF MARYLAND School of Medicine, Baltimore, MD
Introduction: Lichen Planus is an autoimmune skin disorder where lymphocytes on the surface of the dermis of the skin cause a pruritic or burning sensation. It has been reported to manifest in other organs, including the esophagus. Esophageal lichen planus (ELP) is an rare condition with about 100 cases reported in the literature.1 We present a case of lichen esophagitis in a middle-aged male patient from Nigeria, as opposed to the usual demographic of older white females.
Case Description/
Methods: This is a case of a 48-year-old Nigerian male who presented with chronic dysphagia. Endoscopic evaluation revealed hyperkeratotic mucosa, fragile mucosa, denudation, with proximal stenosis in the upper esophagus precluding advancement of the endoscope, consistent with ELP. After Savary dilation and subsequent advancement of the endoscope. An additional, severe, 2 mm stricture was seen in the distal esophagus at the GE junction, which was not traversed. Biopsies showed no evidence of malignancy from the strictures. Esophageal biopsies revealed changes consistent with a lichenoid esophagitis pattern. Biopsies were negative for viral cytopathic effects and dysplasia, and histological features of eosinophilic esophagitis were not identified. He was prescribed oral budesonide and returned for repeat Savary and balloon dilation of the strictures for a total of 3 endoscopic sessions. Interestingly, repeat biopsies revealed only chronic inflammation. On examination, he did not have any features of cutaneous lichen, and he denied any dermatologic symptoms. His symptoms improved with the dilation and oral budesonide.
Discussion: Most ELP patients are elderly, white females.1,2 Stenoses occur in the proximal esophagus in 41% of cases.3 This can be treated with topical steroids and serial dilation of strictures. Low prevalence, lack of endoscopist experience, and lack of pathological experience with ELP lead to delayed diagnoses or confusion with the reflux, requiring multiple studies for a definitive diagnosis. This case presents an unusual demographic for a severe presentation of ELP, which includes the age and ethnicity. Interestingly, biopsies showed chronic inflammation at times in this patient, highlighting the importance of a high index of clinical suspicion, regardless of demographic.
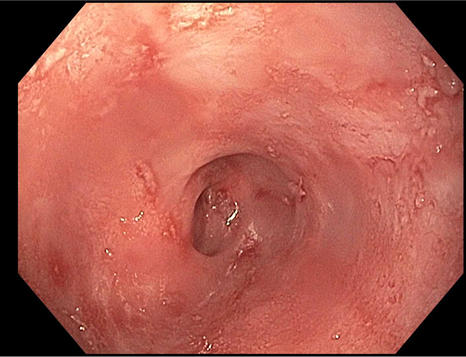
Figure: Image 1: Proximal esophageal stricture with skin like changes in the mucosa consistent with Lichen esophagus

Figure: Image 2: Positivity on Immunofluorescence for fibrinogen from the esophageal biopsies consistent with Lichen esophagus
Disclosures:
Jerry Rose indicated no relevant financial relationships.
Andrew Leopold indicated no relevant financial relationships.
William Twaddell indicated no relevant financial relationships.
Abdulhameed Al-Sabban indicated no relevant financial relationships.
Jerry H. Rose, MD1, Andrew Leopold, MD2, William Twaddell, MD2, Abdulhameed M. Al-Sabban, MBBS3. P4961 - An Unusual Presentation for Lichen Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Maryland Medical System, Baltimore, MD; 2University of Maryland Medical Center, Baltimore, MD; 3UNIVERSITY OF MARYLAND School of Medicine, Baltimore, MD
Introduction: Lichen Planus is an autoimmune skin disorder where lymphocytes on the surface of the dermis of the skin cause a pruritic or burning sensation. It has been reported to manifest in other organs, including the esophagus. Esophageal lichen planus (ELP) is an rare condition with about 100 cases reported in the literature.1 We present a case of lichen esophagitis in a middle-aged male patient from Nigeria, as opposed to the usual demographic of older white females.
Case Description/
Methods: This is a case of a 48-year-old Nigerian male who presented with chronic dysphagia. Endoscopic evaluation revealed hyperkeratotic mucosa, fragile mucosa, denudation, with proximal stenosis in the upper esophagus precluding advancement of the endoscope, consistent with ELP. After Savary dilation and subsequent advancement of the endoscope. An additional, severe, 2 mm stricture was seen in the distal esophagus at the GE junction, which was not traversed. Biopsies showed no evidence of malignancy from the strictures. Esophageal biopsies revealed changes consistent with a lichenoid esophagitis pattern. Biopsies were negative for viral cytopathic effects and dysplasia, and histological features of eosinophilic esophagitis were not identified. He was prescribed oral budesonide and returned for repeat Savary and balloon dilation of the strictures for a total of 3 endoscopic sessions. Interestingly, repeat biopsies revealed only chronic inflammation. On examination, he did not have any features of cutaneous lichen, and he denied any dermatologic symptoms. His symptoms improved with the dilation and oral budesonide.
Discussion: Most ELP patients are elderly, white females.1,2 Stenoses occur in the proximal esophagus in 41% of cases.3 This can be treated with topical steroids and serial dilation of strictures. Low prevalence, lack of endoscopist experience, and lack of pathological experience with ELP lead to delayed diagnoses or confusion with the reflux, requiring multiple studies for a definitive diagnosis. This case presents an unusual demographic for a severe presentation of ELP, which includes the age and ethnicity. Interestingly, biopsies showed chronic inflammation at times in this patient, highlighting the importance of a high index of clinical suspicion, regardless of demographic.
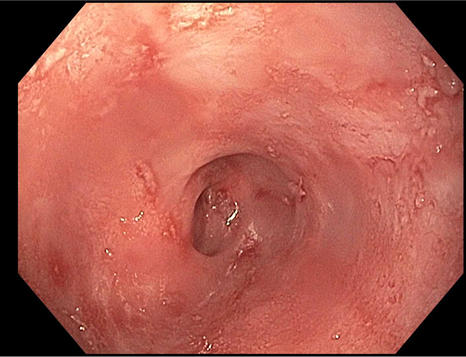
Figure: Image 1: Proximal esophageal stricture with skin like changes in the mucosa consistent with Lichen esophagus

Figure: Image 2: Positivity on Immunofluorescence for fibrinogen from the esophageal biopsies consistent with Lichen esophagus
Disclosures:
Jerry Rose indicated no relevant financial relationships.
Andrew Leopold indicated no relevant financial relationships.
William Twaddell indicated no relevant financial relationships.
Abdulhameed Al-Sabban indicated no relevant financial relationships.
Jerry H. Rose, MD1, Andrew Leopold, MD2, William Twaddell, MD2, Abdulhameed M. Al-Sabban, MBBS3. P4961 - An Unusual Presentation for Lichen Esophagitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
