Tuesday Poster Session
Category: Esophagus
P4955 - Oral Contraceptives Significantly Reduce the Risk of GERD, Esophagitis and Barrett’s Esophagus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Kelly M. Vo, DO (she/her/hers)
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Kelly M. Vo, DO1, Himsikhar Khataniar, MD2, Nikki Duong, MD3, Michael Adams, DO1
1Walter Reed National Military Medical Center, Bethesda, MD; 2Allegheny General Hospital, Pittsburgh, PA; 3Stanford University, Stanford, CA
Introduction: Gastroesophageal reflux disease (GERD) affects over 784 million people worldwide. Hormonal contraceptives have been suggested to influence GERD risk due to their effects on gastric acid secretion and esophageal sphincter function. While combined oral contraceptives (COCs) have been more commonly associated with GERD, limited evidence exists on progestin-only contraceptives (POCs). Of women aged 15–49, 65% use contraception, with 1:4 utilizing oral contraceptive pills. Given their widespread use, this study aimed to compare the incidence of GERD and related esophageal conditions between COC and POC users.
Methods: This retrospective cohort study utilized de-identified data from the TriNetX US Collaborative Network, encompassing records from 67 U.S. healthcare organizations. Women aged 18–50 with documented use of POCs, COCs, or no hormonal contraception between January to December 2014 were included. Patients with pre-existing esophageal conditions or confounding health issues were excluded. Propensity score matching was used to control for variables such as age, BMI, alcohol use, smoking, and comorbidities. GERD, esophagitis, Barrett’s esophagus, and esophageal cancer were identified using ICD-10 codes, and outcomes were tracked over a 10-year period.
Results: After matching, both POC and COC users had significantly lower odds of GERD, esophagitis, and Barrett’s esophagus compared to the control group. GERD incidence was lowest in POC users (9.76%) versus COC users (11.30%) and controls (12.60%). POC users also had a lower risk of esophagitis than both COC users and controls. Both contraceptive groups had reduced odds of Barrett’s esophagus, with no significant difference between them. Esophageal cancer was rare and showed no significant differences across groups.
Discussion: This study demonstrates that both POCs and COCs are associated with a reduced risk of GERD compared to controls, with POCs showing a stronger protective effect. This contrasts with previous findings suggesting estrogen increases GERD risk. The long-term design and rigorous matching in this study may explain the differing results. The protective effect may be attributed to synthetic progestins enhancing lower esophageal sphincter tone and reducing inflammation. Further clinical trials are needed to confirm these results and explore underlying mechanisms.
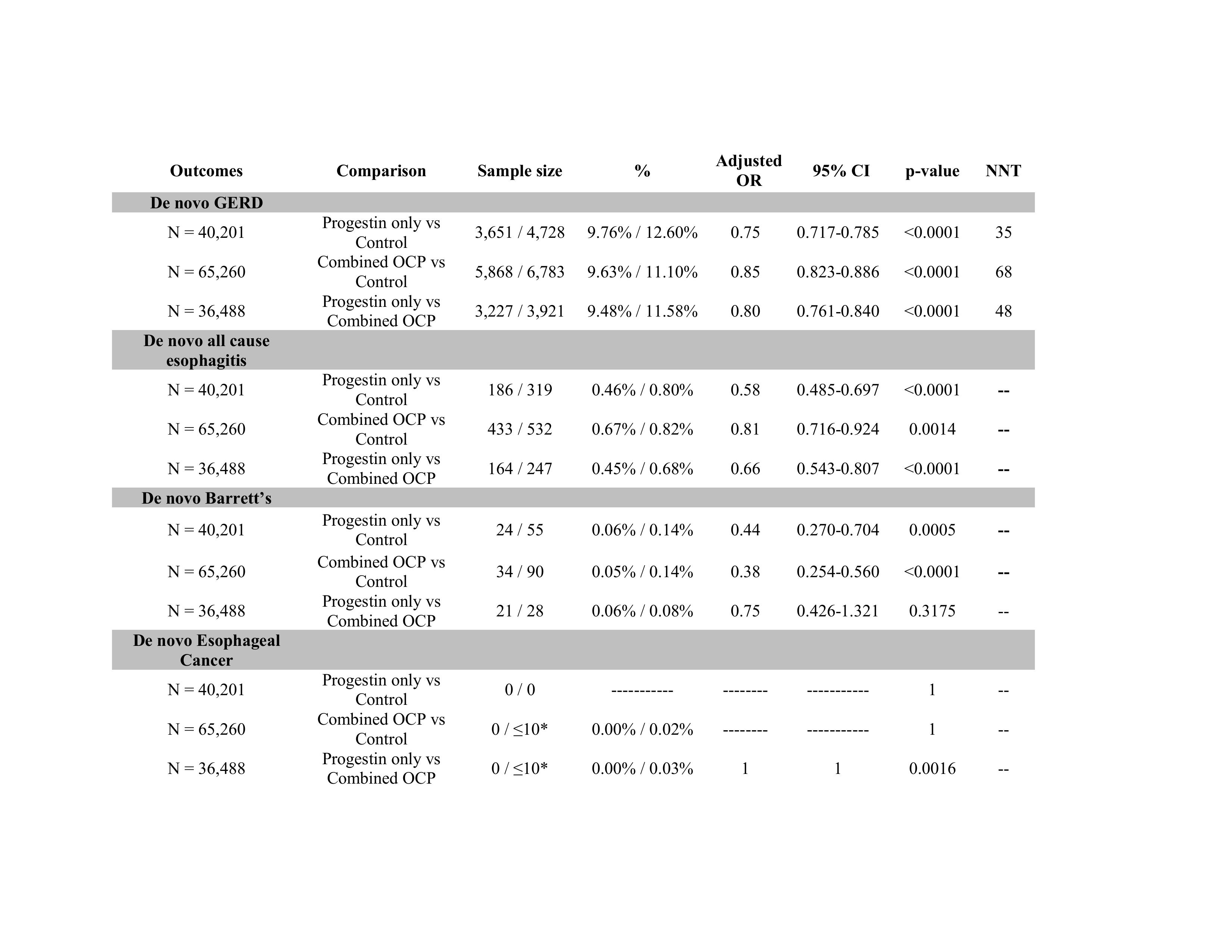
Figure: Table 1: Comparative outcomes of oral contraception within 10 years of contraceptive use (after propensity matching)
Note: *1-10 incidences are all reported as ≤10 to maintain anonymity.
Abbreviations: N = cohort sample size after propensity matching, GERD (gastroesophageal reflux disease), OCP (oral contraceptive pills), OR (odd ratio), CI (confidence interval)
Disclosures:
Kelly Vo indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Michael Adams indicated no relevant financial relationships.
Kelly M. Vo, DO1, Himsikhar Khataniar, MD2, Nikki Duong, MD3, Michael Adams, DO1. P4955 - Oral Contraceptives Significantly Reduce the Risk of GERD, Esophagitis and Barrett’s Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2Allegheny General Hospital, Pittsburgh, PA; 3Stanford University, Stanford, CA
Introduction: Gastroesophageal reflux disease (GERD) affects over 784 million people worldwide. Hormonal contraceptives have been suggested to influence GERD risk due to their effects on gastric acid secretion and esophageal sphincter function. While combined oral contraceptives (COCs) have been more commonly associated with GERD, limited evidence exists on progestin-only contraceptives (POCs). Of women aged 15–49, 65% use contraception, with 1:4 utilizing oral contraceptive pills. Given their widespread use, this study aimed to compare the incidence of GERD and related esophageal conditions between COC and POC users.
Methods: This retrospective cohort study utilized de-identified data from the TriNetX US Collaborative Network, encompassing records from 67 U.S. healthcare organizations. Women aged 18–50 with documented use of POCs, COCs, or no hormonal contraception between January to December 2014 were included. Patients with pre-existing esophageal conditions or confounding health issues were excluded. Propensity score matching was used to control for variables such as age, BMI, alcohol use, smoking, and comorbidities. GERD, esophagitis, Barrett’s esophagus, and esophageal cancer were identified using ICD-10 codes, and outcomes were tracked over a 10-year period.
Results: After matching, both POC and COC users had significantly lower odds of GERD, esophagitis, and Barrett’s esophagus compared to the control group. GERD incidence was lowest in POC users (9.76%) versus COC users (11.30%) and controls (12.60%). POC users also had a lower risk of esophagitis than both COC users and controls. Both contraceptive groups had reduced odds of Barrett’s esophagus, with no significant difference between them. Esophageal cancer was rare and showed no significant differences across groups.
Discussion: This study demonstrates that both POCs and COCs are associated with a reduced risk of GERD compared to controls, with POCs showing a stronger protective effect. This contrasts with previous findings suggesting estrogen increases GERD risk. The long-term design and rigorous matching in this study may explain the differing results. The protective effect may be attributed to synthetic progestins enhancing lower esophageal sphincter tone and reducing inflammation. Further clinical trials are needed to confirm these results and explore underlying mechanisms.
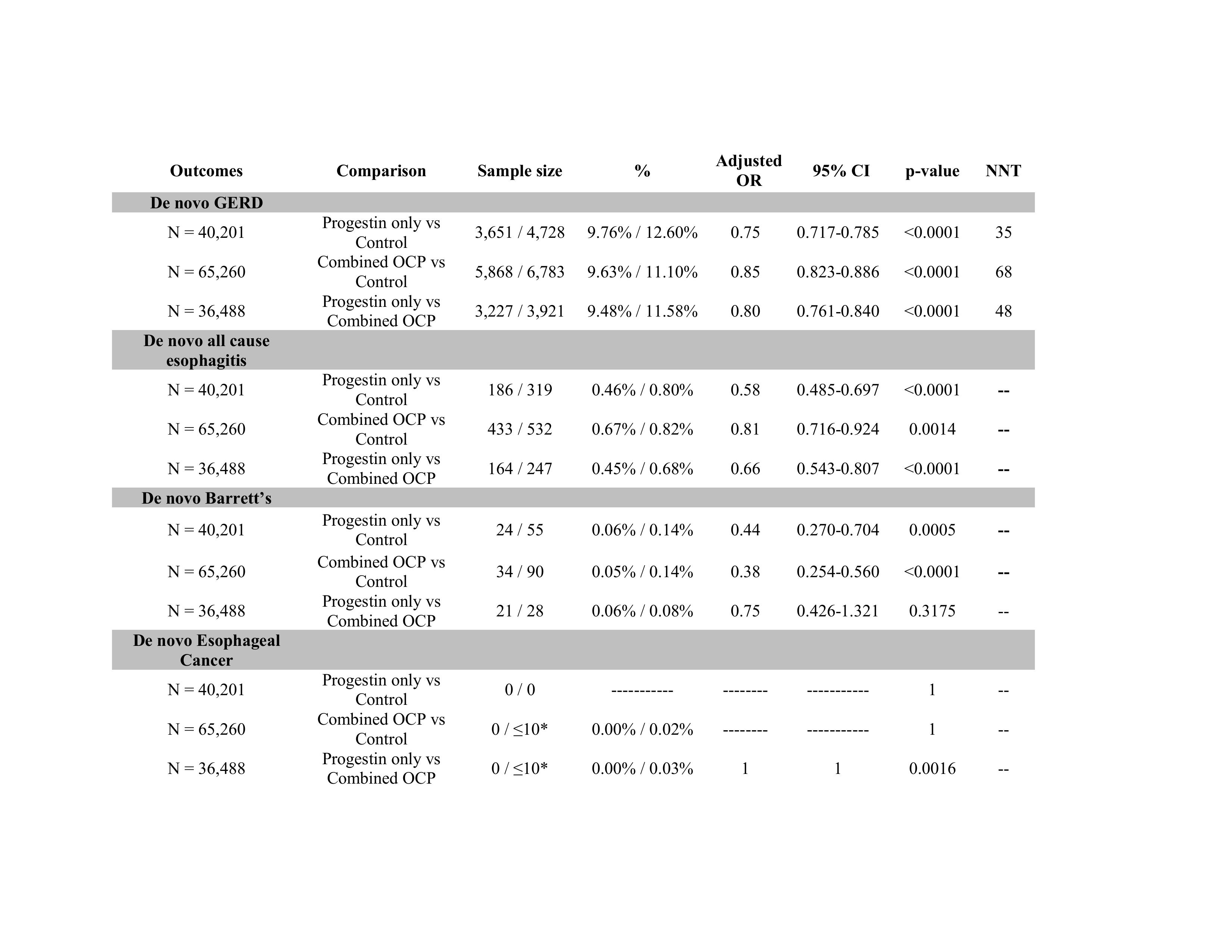
Figure: Table 1: Comparative outcomes of oral contraception within 10 years of contraceptive use (after propensity matching)
Note: *1-10 incidences are all reported as ≤10 to maintain anonymity.
Abbreviations: N = cohort sample size after propensity matching, GERD (gastroesophageal reflux disease), OCP (oral contraceptive pills), OR (odd ratio), CI (confidence interval)
Disclosures:
Kelly Vo indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Michael Adams indicated no relevant financial relationships.
Kelly M. Vo, DO1, Himsikhar Khataniar, MD2, Nikki Duong, MD3, Michael Adams, DO1. P4955 - Oral Contraceptives Significantly Reduce the Risk of GERD, Esophagitis and Barrett’s Esophagus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
