Tuesday Poster Session
Category: Esophagus
P4953 - Minimally Invasive versus Open Esophagectomy for Locally Advanced Esophageal Cancer: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Angsupat Pornchai, MD (she/her/hers)
University of Pittsburgh Medical Center
Harrisburg, PA
Presenting Author(s)
Angsupat Pornchai, MD1, Maneeth Mylavarapu, MBBS, MPH2, Harshaman Kaur, MD3, Angad Tiwari, 4, Eshan Nanda, MD1
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Walker Baptist Medical Center, Jasper, AL; 3Honor Health Mountain Vista Medical Center, Mesa, AZ; 4Maharani Laxmi Bai Medical College, Jhansi, Uttar Pradesh, India
Introduction: While minimally invasive esophagectomy (MIE) has emerged as a potential alternative to open esophagectomy (OE) for esophageal cancer, its specific perioperative benefits in locally advanced esophageal cancer (LAEC) have not been thoroughly evaluated. This meta-analysis aims to compare intra- and postoperative outcomes of MIE versus OE, focusing on the LAEC population.
Methods: A systematic review adhering to PRISMA guidelines was conducted across PubMed/MEDLINE, Scopus, Science Direct, and Cochrane/CENTRAL. Studies directly comparing MIE and OE for LAEC were included. Intraoperative endpoints were estimated blood loss (EBL) and operative duration. Postoperative endpoints included length of hospital stay (LOS), intensive care unit LOS (ICU-LOS), postoperative complications (Clavien-Dindo ≥ II), blood transfusion, and 30-day mortality. Random-effects models were used to calculate mean differences (MD) and odds ratios (OR) with 95% confidence intervals (CI).
Results: Our meta-analysis included 6 studies (5 retrospective, 1 prospective) encompassing 2,065 patients with LAEC (MIE = 1,136; OE = 929). The MIE group presented with a slightly older mean age (64.6 years vs. 63.8 years) and a marginally higher proportion of females (57.2% vs. 56.0%) than the OE group. Intraoperatively, MIE resulted in significantly lower EBL (MD –176.70 ml; 95% CI –251.34, –102.07; p < 0.00001), while operative duration was comparable (MD –2.13 min; 95% CI –40.73, 36.48; p = 0.91). Postoperatively, MIE was associated with a shorter overall LOS (MD –1.57 days; 95% CI –2.24, –0.89; p < 0.00001) and reduced odds of blood transfusion (OR 0.51; 95% CI 0.30, 0.88; p = 0.01). ICU-LOS (MD 0.00 days; 95% CI –0.04, 0.04; p = 0.99), postoperative complications (OR 0.43; 95% CI 0.17, 1.12; p = 0.08), and 30-day mortality (OR 0.50; 95% CI 0.17, 1.42; p = 0.19) did not significantly differ between the groups.
Discussion: This meta-analysis suggests that, in patients with LAEC, MIE is associated with reduced blood loss, shorter hospital stay, and lower transfusion rates compared to OE. While operative time, ICU-LOS, major complications, and 30-day mortality were similar, further prospective research is needed to validate these findings and assess long-term outcomes in this specific population.
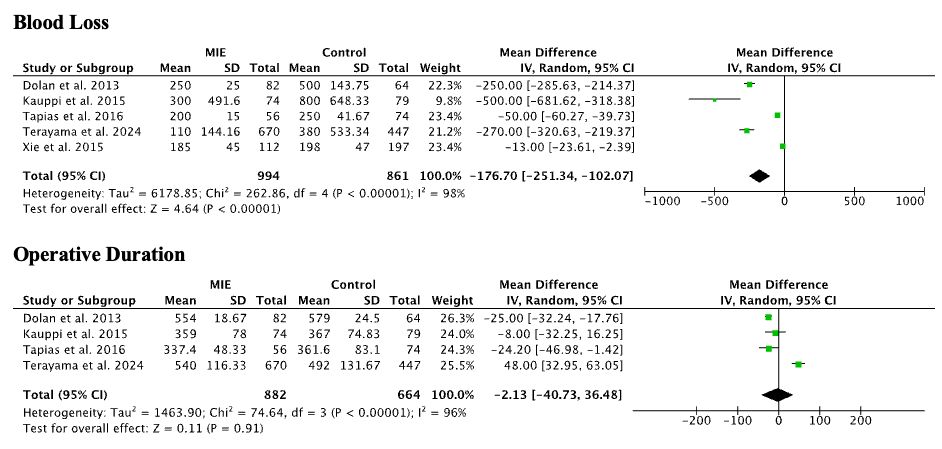
Figure: Intraoperative Outcomes
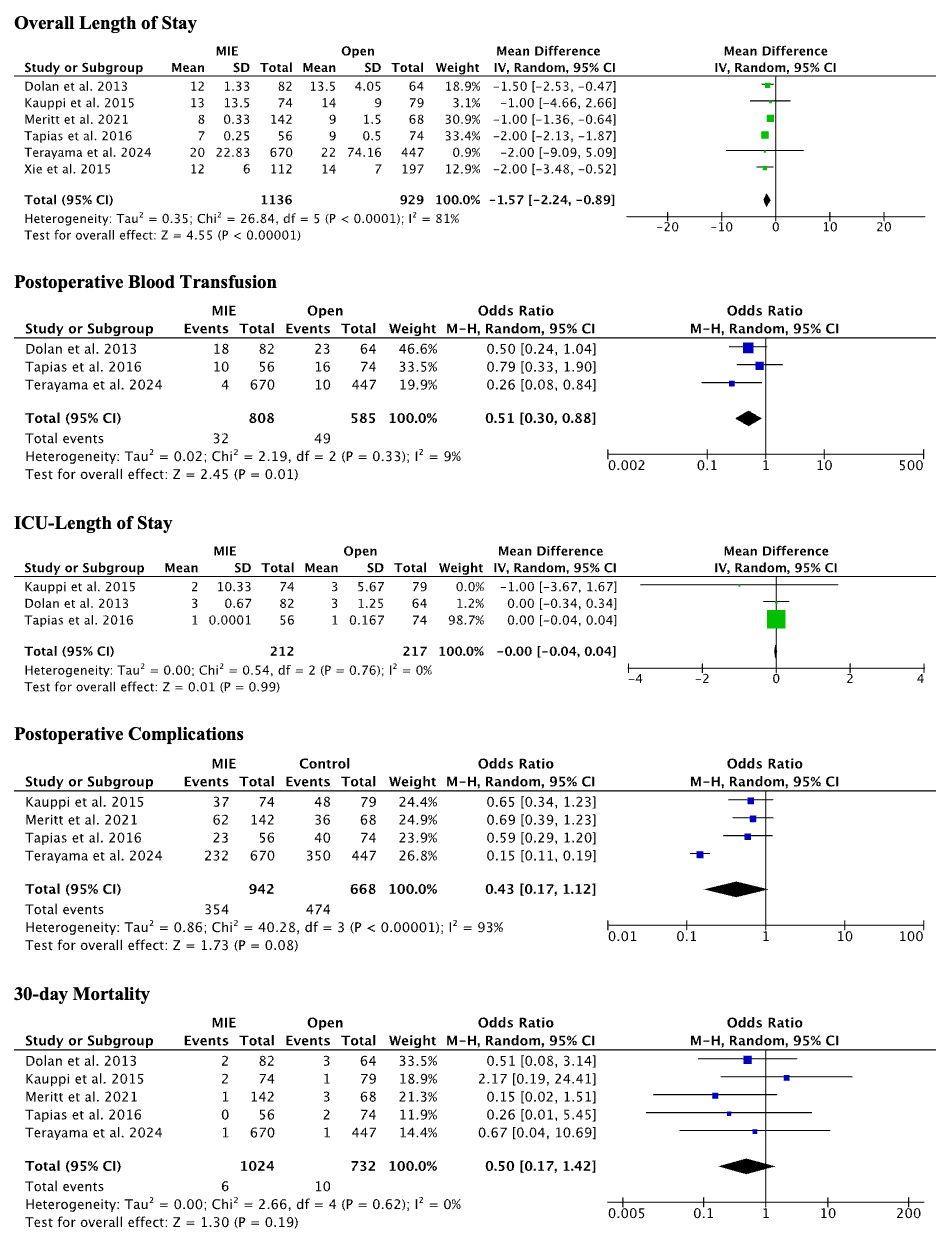
Figure: Postoperative Outcomes
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Maneeth Mylavarapu indicated no relevant financial relationships.
Harshaman Kaur indicated no relevant financial relationships.
Angad Tiwari indicated no relevant financial relationships.
Eshan Nanda indicated no relevant financial relationships.
Angsupat Pornchai, MD1, Maneeth Mylavarapu, MBBS, MPH2, Harshaman Kaur, MD3, Angad Tiwari, 4, Eshan Nanda, MD1. P4953 - Minimally Invasive versus Open Esophagectomy for Locally Advanced Esophageal Cancer: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Walker Baptist Medical Center, Jasper, AL; 3Honor Health Mountain Vista Medical Center, Mesa, AZ; 4Maharani Laxmi Bai Medical College, Jhansi, Uttar Pradesh, India
Introduction: While minimally invasive esophagectomy (MIE) has emerged as a potential alternative to open esophagectomy (OE) for esophageal cancer, its specific perioperative benefits in locally advanced esophageal cancer (LAEC) have not been thoroughly evaluated. This meta-analysis aims to compare intra- and postoperative outcomes of MIE versus OE, focusing on the LAEC population.
Methods: A systematic review adhering to PRISMA guidelines was conducted across PubMed/MEDLINE, Scopus, Science Direct, and Cochrane/CENTRAL. Studies directly comparing MIE and OE for LAEC were included. Intraoperative endpoints were estimated blood loss (EBL) and operative duration. Postoperative endpoints included length of hospital stay (LOS), intensive care unit LOS (ICU-LOS), postoperative complications (Clavien-Dindo ≥ II), blood transfusion, and 30-day mortality. Random-effects models were used to calculate mean differences (MD) and odds ratios (OR) with 95% confidence intervals (CI).
Results: Our meta-analysis included 6 studies (5 retrospective, 1 prospective) encompassing 2,065 patients with LAEC (MIE = 1,136; OE = 929). The MIE group presented with a slightly older mean age (64.6 years vs. 63.8 years) and a marginally higher proportion of females (57.2% vs. 56.0%) than the OE group. Intraoperatively, MIE resulted in significantly lower EBL (MD –176.70 ml; 95% CI –251.34, –102.07; p < 0.00001), while operative duration was comparable (MD –2.13 min; 95% CI –40.73, 36.48; p = 0.91). Postoperatively, MIE was associated with a shorter overall LOS (MD –1.57 days; 95% CI –2.24, –0.89; p < 0.00001) and reduced odds of blood transfusion (OR 0.51; 95% CI 0.30, 0.88; p = 0.01). ICU-LOS (MD 0.00 days; 95% CI –0.04, 0.04; p = 0.99), postoperative complications (OR 0.43; 95% CI 0.17, 1.12; p = 0.08), and 30-day mortality (OR 0.50; 95% CI 0.17, 1.42; p = 0.19) did not significantly differ between the groups.
Discussion: This meta-analysis suggests that, in patients with LAEC, MIE is associated with reduced blood loss, shorter hospital stay, and lower transfusion rates compared to OE. While operative time, ICU-LOS, major complications, and 30-day mortality were similar, further prospective research is needed to validate these findings and assess long-term outcomes in this specific population.
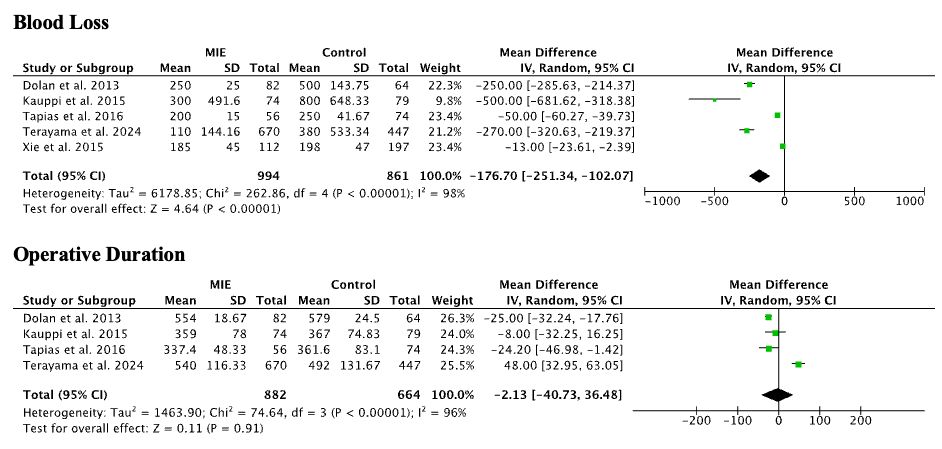
Figure: Intraoperative Outcomes
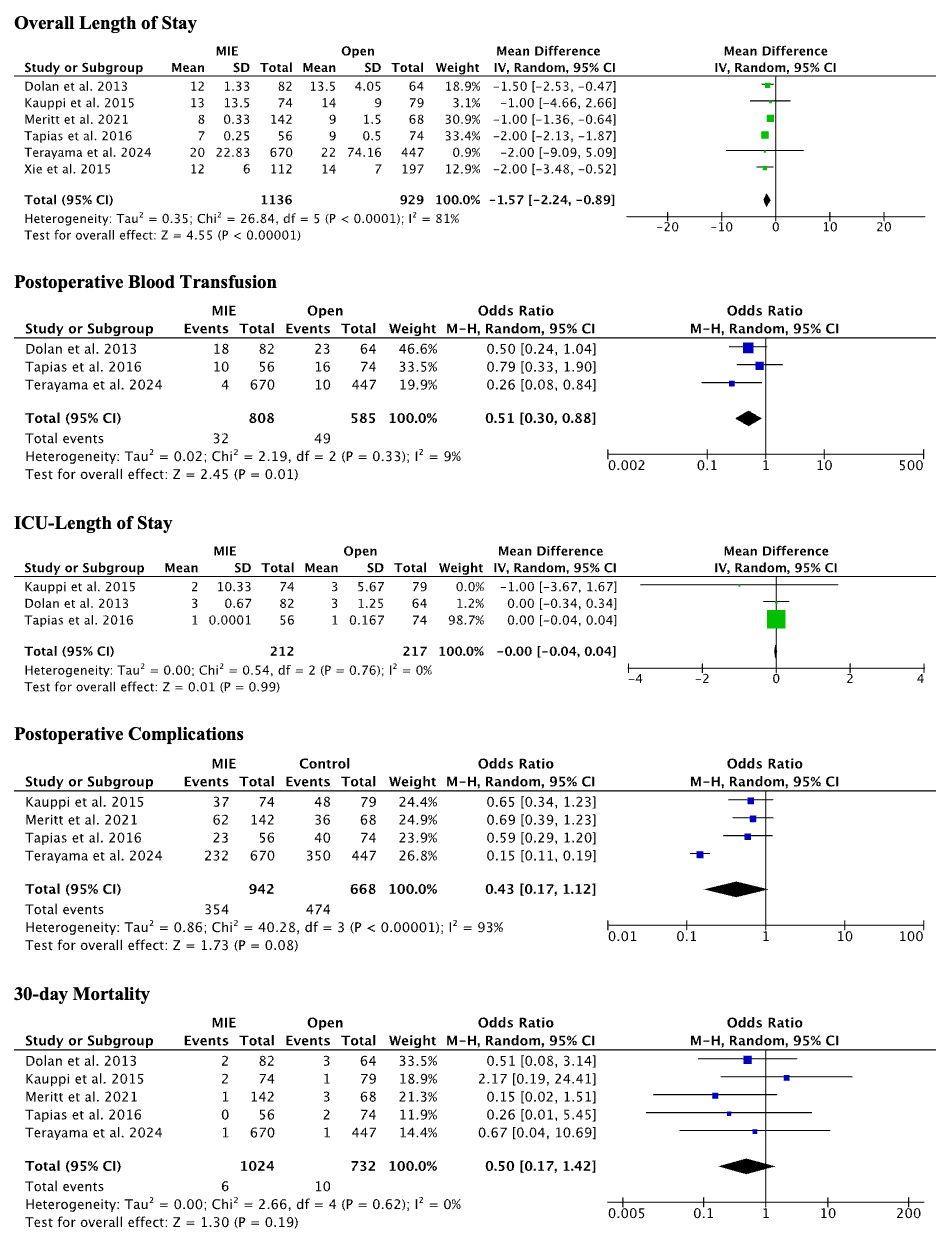
Figure: Postoperative Outcomes
Disclosures:
Angsupat Pornchai indicated no relevant financial relationships.
Maneeth Mylavarapu indicated no relevant financial relationships.
Harshaman Kaur indicated no relevant financial relationships.
Angad Tiwari indicated no relevant financial relationships.
Eshan Nanda indicated no relevant financial relationships.
Angsupat Pornchai, MD1, Maneeth Mylavarapu, MBBS, MPH2, Harshaman Kaur, MD3, Angad Tiwari, 4, Eshan Nanda, MD1. P4953 - Minimally Invasive versus Open Esophagectomy for Locally Advanced Esophageal Cancer: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
