Tuesday Poster Session
Category: Esophagus
P4950 - Optimizing Dysphagia Management: The Role of Manometry and Dilator Size in Empiric Esophageal Dilation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DR
Daniyal Raza, MD (he/him/his)
LSU Health Sciences Center - SHREVEPORT, LA
Shreveport, LA
Presenting Author(s)
Daniyal Raza, MD1, Maryam Mubashir, MD2, Rohit Goyal, MD2, Lena Kawji, MD2, David Okuampa, MD3, Khadija Khan, MD3, Farhan Mohiuddin, MD4, Mohammad Alfrad Nobel Bhuiyan, MD2, Qiang Cai, MD, PhD, MACG1, Hassaan A. Zia, MD5
1LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA; 2Louisiana State University, Shreveport, LA; 3LSU Health Shreveport, Shreveport, LA; 4Louisiana State University School of Medicine, New Orleans, LA; 5Medical College of Wisconsin, Shreveport, LA
Introduction: Empiric esophageal dilation (EED) is frequently employed for nonobstructive dysphagia (NOD), yet the influence of procedural factors such as manometry utilization and dilator size on clinical outcomes remains unclear. This study evaluates their impact to inform best practices.
Methods: We retrospectively reviewed 83 patients who underwent EED for NOD. Symptom severity was assessed using the NIH PROMIS-GI dysphagia scale at baseline and post-dilation. Patients were stratified based on whether pre-procedural manometry was performed and by dilator size (small: 16–17 mm; medium: 18–19 mm; large: ≥20 mm). T-tests, ANOVA, and logistic regression were used to assess predictors of symptom improvement and complication rates.
Results: Among the cohort, 21 patients (25.3%) underwent manometry prior to EED, while 62 (74.7%) did not. Dysphagia improvement was noted in 47.6% of patients with manometry versus 62.9% without (p = 0.223). Improvement varied significantly by dilator size: 78.6% with small, 57.8% with medium, and 25.0% with large dilators (p = 0.04). Complications included mucosal tears (31.3%) and bleeding (14.5%), with no significant association to manometry or dilator size.
Discussion: In this single-center study, smaller dilators were associated with significantly higher symptom improvement in patients undergoing EED for NOD. Pre-procedural manometry did not significantly influence outcomes. These findings support a tailored procedural approach, particularly the use of smaller dilators, in optimizing dysphagia management. Prospective studies are needed to confirm these results and inform guidelines.
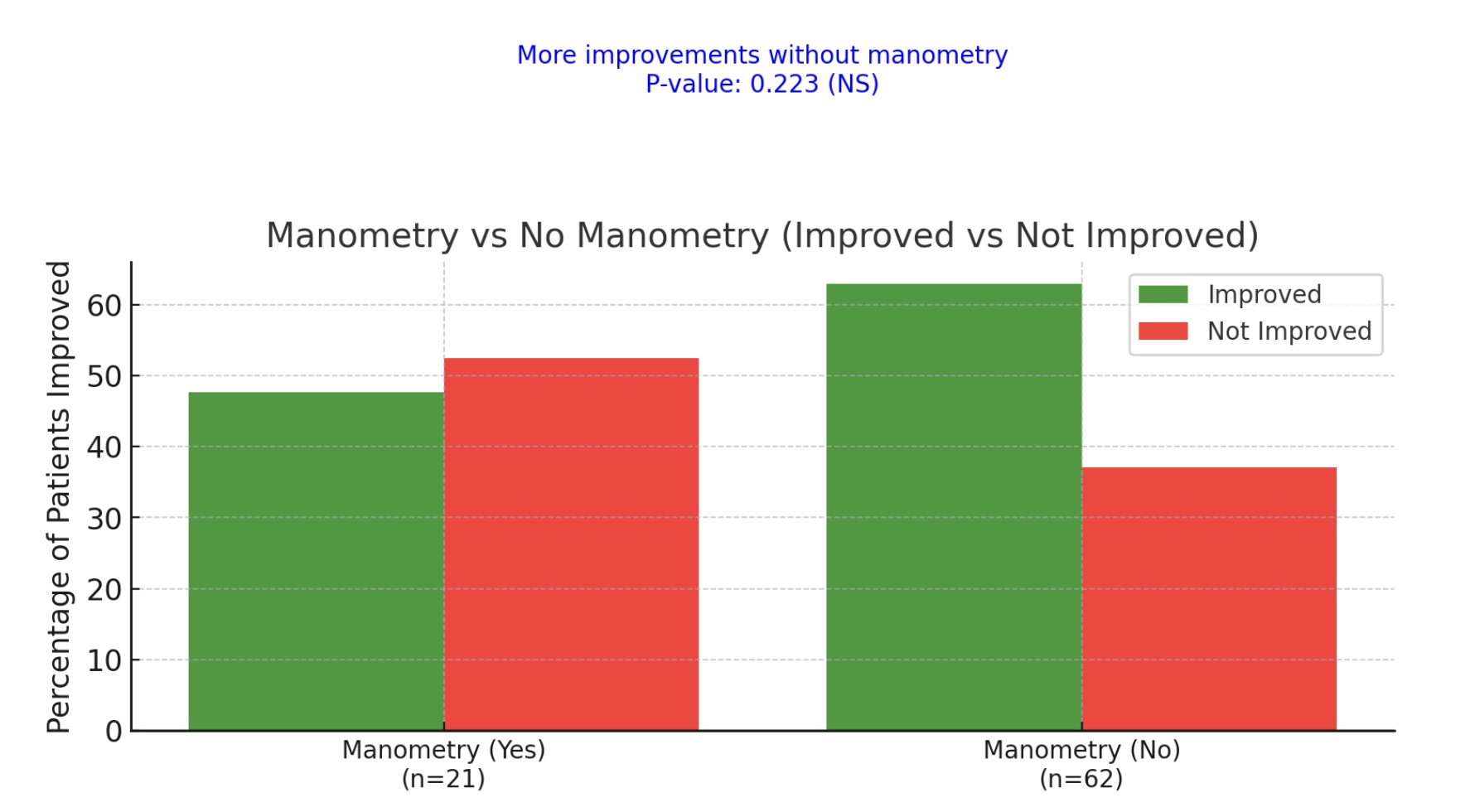
Figure: Figure. 1: Manometry vs. No Manometry: Improvement in Dysphagia Symptoms with and
without Pre-Procedural Manometry.
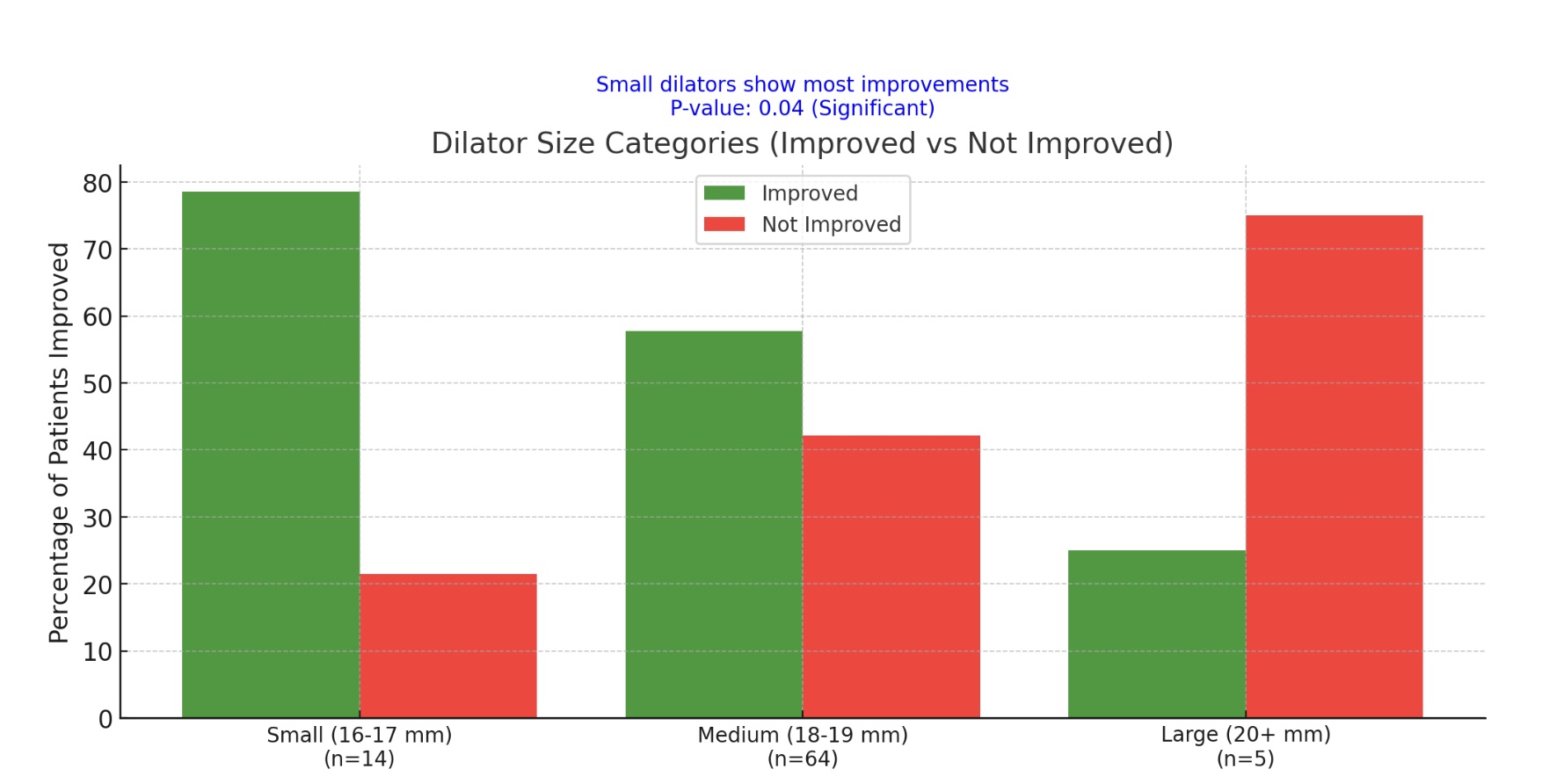
Figure: Figure. 2: For Dilator Size Categories: Improvement in Dysphagia Symptoms by Dilator Size
Categories.
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Maryam Mubashir indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Lena Kawji indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Khadija Khan indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Mohammad Alfrad Nobel Bhuiyan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Hassaan A. Zia indicated no relevant financial relationships.
Daniyal Raza, MD1, Maryam Mubashir, MD2, Rohit Goyal, MD2, Lena Kawji, MD2, David Okuampa, MD3, Khadija Khan, MD3, Farhan Mohiuddin, MD4, Mohammad Alfrad Nobel Bhuiyan, MD2, Qiang Cai, MD, PhD, MACG1, Hassaan A. Zia, MD5. P4950 - Optimizing Dysphagia Management: The Role of Manometry and Dilator Size in Empiric Esophageal Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA; 2Louisiana State University, Shreveport, LA; 3LSU Health Shreveport, Shreveport, LA; 4Louisiana State University School of Medicine, New Orleans, LA; 5Medical College of Wisconsin, Shreveport, LA
Introduction: Empiric esophageal dilation (EED) is frequently employed for nonobstructive dysphagia (NOD), yet the influence of procedural factors such as manometry utilization and dilator size on clinical outcomes remains unclear. This study evaluates their impact to inform best practices.
Methods: We retrospectively reviewed 83 patients who underwent EED for NOD. Symptom severity was assessed using the NIH PROMIS-GI dysphagia scale at baseline and post-dilation. Patients were stratified based on whether pre-procedural manometry was performed and by dilator size (small: 16–17 mm; medium: 18–19 mm; large: ≥20 mm). T-tests, ANOVA, and logistic regression were used to assess predictors of symptom improvement and complication rates.
Results: Among the cohort, 21 patients (25.3%) underwent manometry prior to EED, while 62 (74.7%) did not. Dysphagia improvement was noted in 47.6% of patients with manometry versus 62.9% without (p = 0.223). Improvement varied significantly by dilator size: 78.6% with small, 57.8% with medium, and 25.0% with large dilators (p = 0.04). Complications included mucosal tears (31.3%) and bleeding (14.5%), with no significant association to manometry or dilator size.
Discussion: In this single-center study, smaller dilators were associated with significantly higher symptom improvement in patients undergoing EED for NOD. Pre-procedural manometry did not significantly influence outcomes. These findings support a tailored procedural approach, particularly the use of smaller dilators, in optimizing dysphagia management. Prospective studies are needed to confirm these results and inform guidelines.
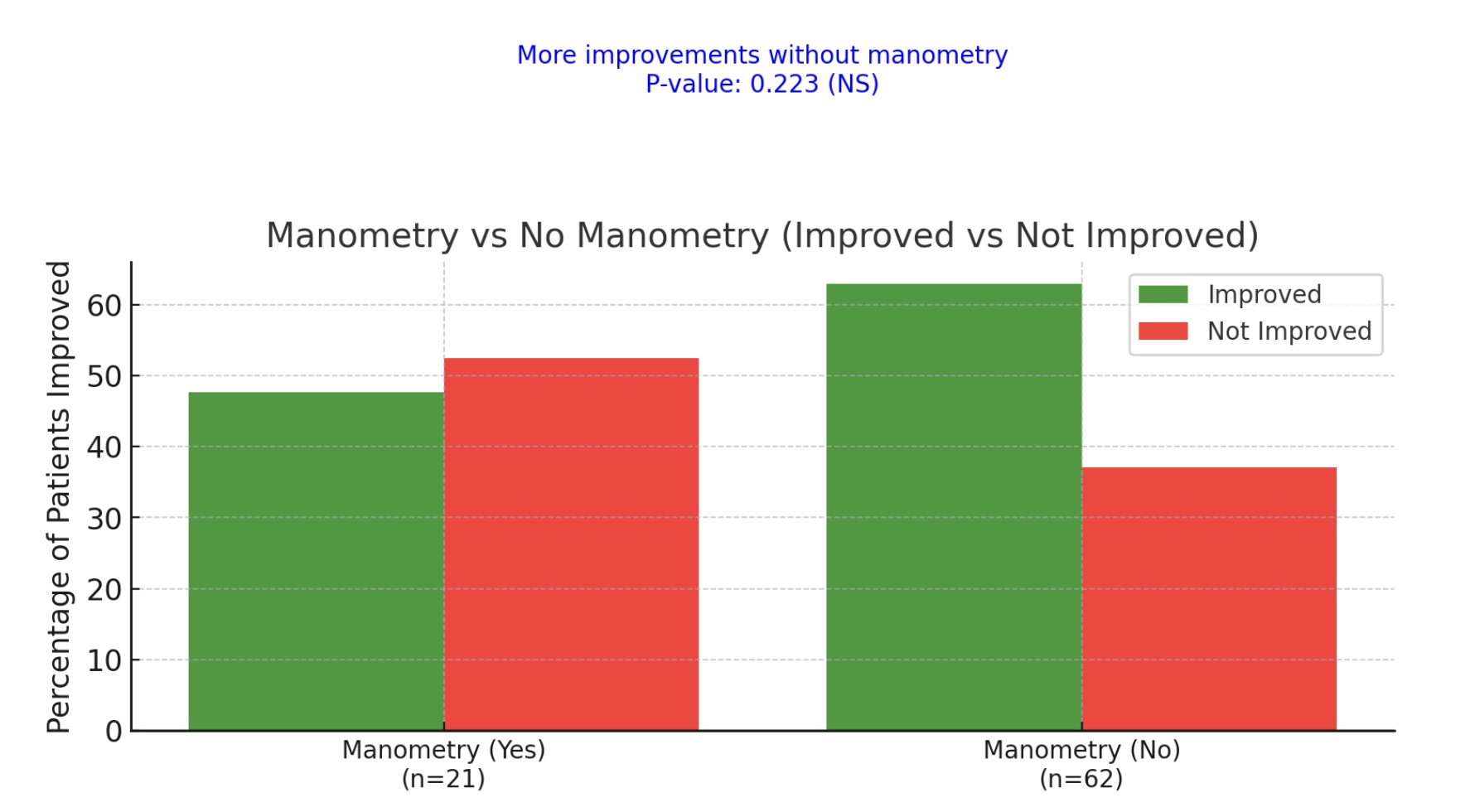
Figure: Figure. 1: Manometry vs. No Manometry: Improvement in Dysphagia Symptoms with and
without Pre-Procedural Manometry.
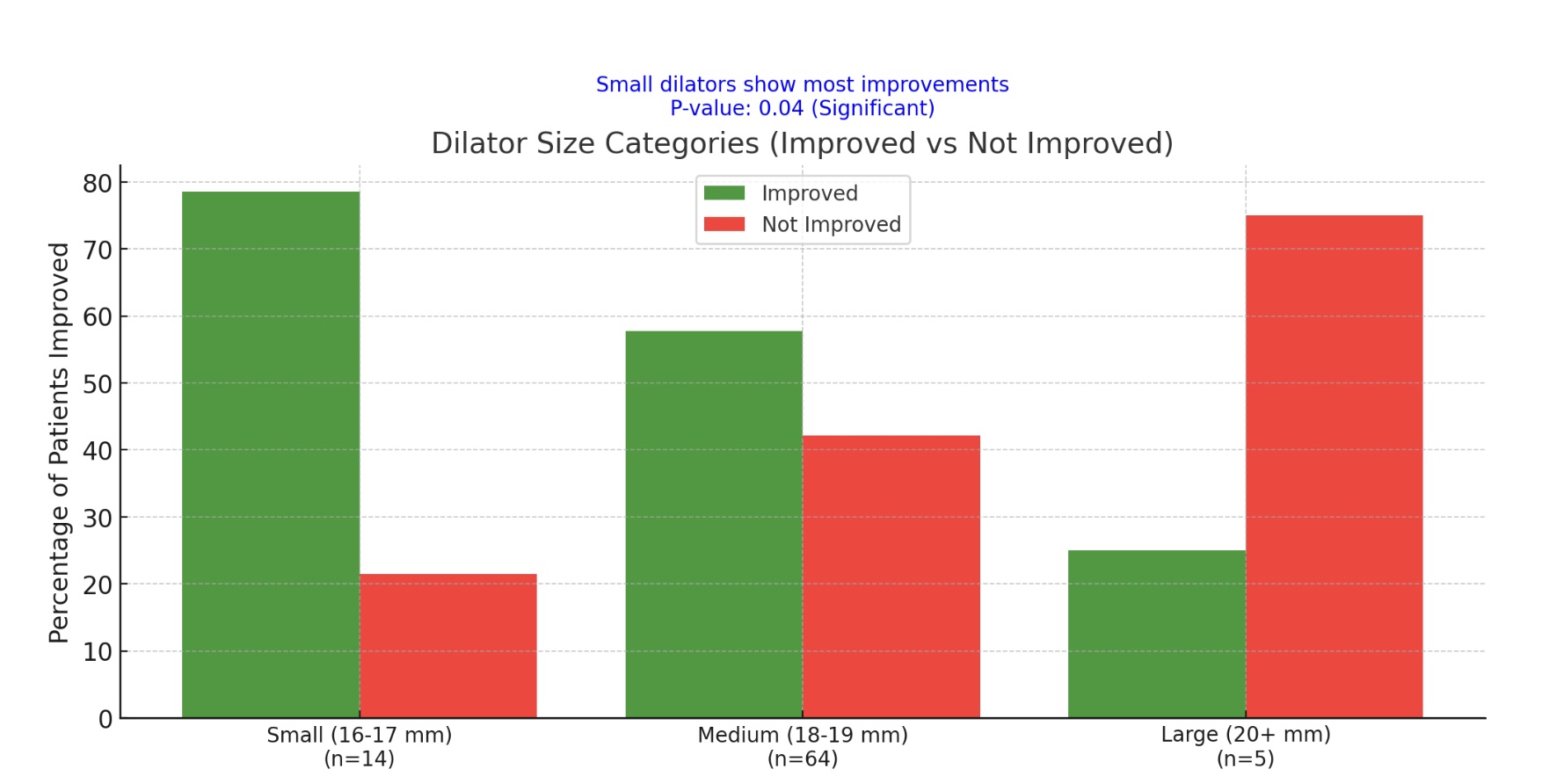
Figure: Figure. 2: For Dilator Size Categories: Improvement in Dysphagia Symptoms by Dilator Size
Categories.
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Maryam Mubashir indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Lena Kawji indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Khadija Khan indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Mohammad Alfrad Nobel Bhuiyan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Hassaan A. Zia indicated no relevant financial relationships.
Daniyal Raza, MD1, Maryam Mubashir, MD2, Rohit Goyal, MD2, Lena Kawji, MD2, David Okuampa, MD3, Khadija Khan, MD3, Farhan Mohiuddin, MD4, Mohammad Alfrad Nobel Bhuiyan, MD2, Qiang Cai, MD, PhD, MACG1, Hassaan A. Zia, MD5. P4950 - Optimizing Dysphagia Management: The Role of Manometry and Dilator Size in Empiric Esophageal Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
