Tuesday Poster Session
Category: Esophagus
P5051 - Black Esophagus: A Severely Morbid or Benign Finding?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rebecca Beard
Uniformed Services University of the Health Sciences
Bethesda, MD
Presenting Author(s)
Rebecca Beard, 1, Kathryn Driggers, MD2, Henri De La Baume, MD3
1Uniformed Services University of the Health Sciences, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD; 3Fort Belvoir Community Hospital, Fort Belvoir, VA
Introduction: Acute esophageal necrosis (AEN), also known as “black esophagus”, is a rare condition defined by circumferential, black-appearing, esophageal mucosa. The etiology is likely multifactorial secondary to ischemia, impaired mucosal barrier systems, and erosive damage. Upper GI bleeding is the most common presentation. Most patients with AEN have significant underlying comorbidities which are then compounded by a triggering event such as shock or severe infection. This case demonstrates a patient with common risk factors and presentation but who had no notable triggering event.
Case Description/
Methods: An 87-year-old male with atrial fibrillation (on apixaban), BPH, COPD, alcohol use of up to ½ bottle of wine per night, and hyperlipidemia presented to the emergency department with 1 day of dark colored emesis and urinary retention and 2 weeks of mild intermittent dyspepsia. The patient was not taking NSAIDs, aspirin, clopidogrel, or other anticoagulants. He had no notable GI history and no prior endoscopies. An EGD performed shortly after admission demonstrated severe grade D erosive esophagitis with necrosis noted from 40cm (beginning exactly at the Z-line which was regular) to 30cm with subsequent transition to more normal mucosa at 20cm and a 5cm hiatal hernia. The overall findings were consistent with severe grade D, necrotic esophagitis. The patient was treated with IV and then oral proton pump inhibitor, alcohol cessation, and supportive care. He remained hospitalized for congestive heart failure that developed later in his admission. A repeat EGD two months after his initial endoscopic evaluation demonstrated an entirely normal esophagus.
Discussion: This case presents an unusual instance of AEN in an elderly patient with no identifiable triggering event. While he had common risk factors (atrial fibrillation, alcohol use), the absence of significant hypotension or sepsis at diagnosis challenges the conventional two-hit hypothesis of AEN pathophysiology and suggests that there might be other, less severe pathways leading to esophageal ischemia and necrosis. This case highlights the need for further research to explore potential benign mechanisms of AEN, especially in patients who do not fit the usual clinical profile.
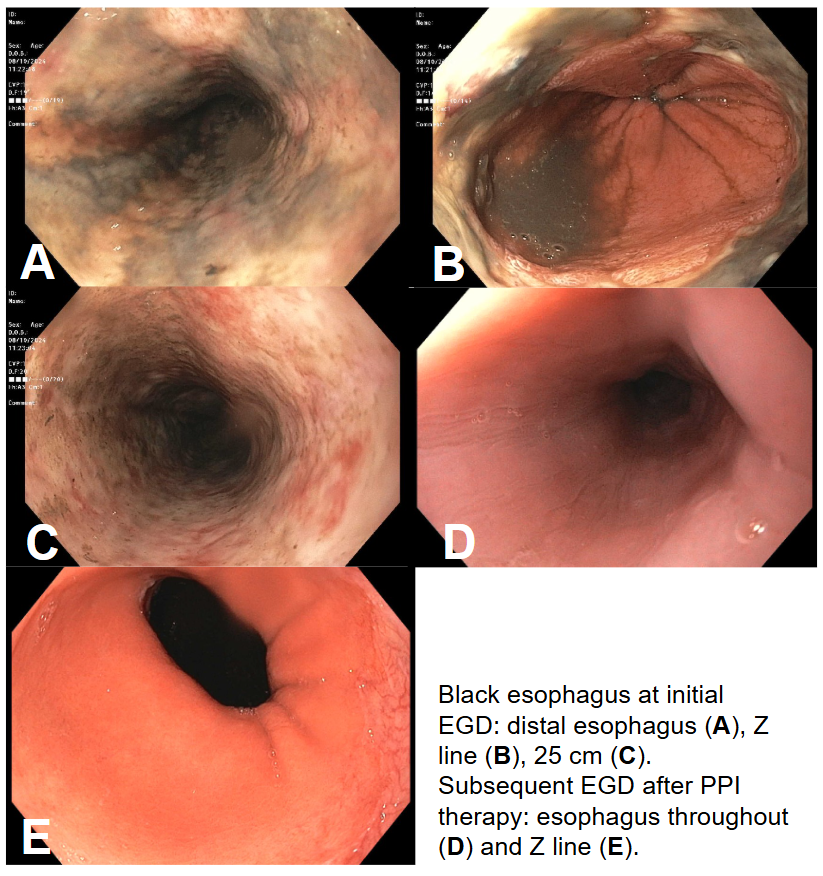
Figure: Black esophagus at initial EGD: distal esophagus (A), Z line (B), 25 cm (C). Subsequent EGD after PPI therapy: esophagus throughout (D) and Z line (E).
Disclosures:
Rebecca Beard indicated no relevant financial relationships.
Kathryn Driggers indicated no relevant financial relationships.
Henri De La Baume indicated no relevant financial relationships.
Rebecca Beard, 1, Kathryn Driggers, MD2, Henri De La Baume, MD3. P5051 - Black Esophagus: A Severely Morbid or Benign Finding?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Uniformed Services University of the Health Sciences, Bethesda, MD; 2Walter Reed National Military Medical Center, Bethesda, MD; 3Fort Belvoir Community Hospital, Fort Belvoir, VA
Introduction: Acute esophageal necrosis (AEN), also known as “black esophagus”, is a rare condition defined by circumferential, black-appearing, esophageal mucosa. The etiology is likely multifactorial secondary to ischemia, impaired mucosal barrier systems, and erosive damage. Upper GI bleeding is the most common presentation. Most patients with AEN have significant underlying comorbidities which are then compounded by a triggering event such as shock or severe infection. This case demonstrates a patient with common risk factors and presentation but who had no notable triggering event.
Case Description/
Methods: An 87-year-old male with atrial fibrillation (on apixaban), BPH, COPD, alcohol use of up to ½ bottle of wine per night, and hyperlipidemia presented to the emergency department with 1 day of dark colored emesis and urinary retention and 2 weeks of mild intermittent dyspepsia. The patient was not taking NSAIDs, aspirin, clopidogrel, or other anticoagulants. He had no notable GI history and no prior endoscopies. An EGD performed shortly after admission demonstrated severe grade D erosive esophagitis with necrosis noted from 40cm (beginning exactly at the Z-line which was regular) to 30cm with subsequent transition to more normal mucosa at 20cm and a 5cm hiatal hernia. The overall findings were consistent with severe grade D, necrotic esophagitis. The patient was treated with IV and then oral proton pump inhibitor, alcohol cessation, and supportive care. He remained hospitalized for congestive heart failure that developed later in his admission. A repeat EGD two months after his initial endoscopic evaluation demonstrated an entirely normal esophagus.
Discussion: This case presents an unusual instance of AEN in an elderly patient with no identifiable triggering event. While he had common risk factors (atrial fibrillation, alcohol use), the absence of significant hypotension or sepsis at diagnosis challenges the conventional two-hit hypothesis of AEN pathophysiology and suggests that there might be other, less severe pathways leading to esophageal ischemia and necrosis. This case highlights the need for further research to explore potential benign mechanisms of AEN, especially in patients who do not fit the usual clinical profile.
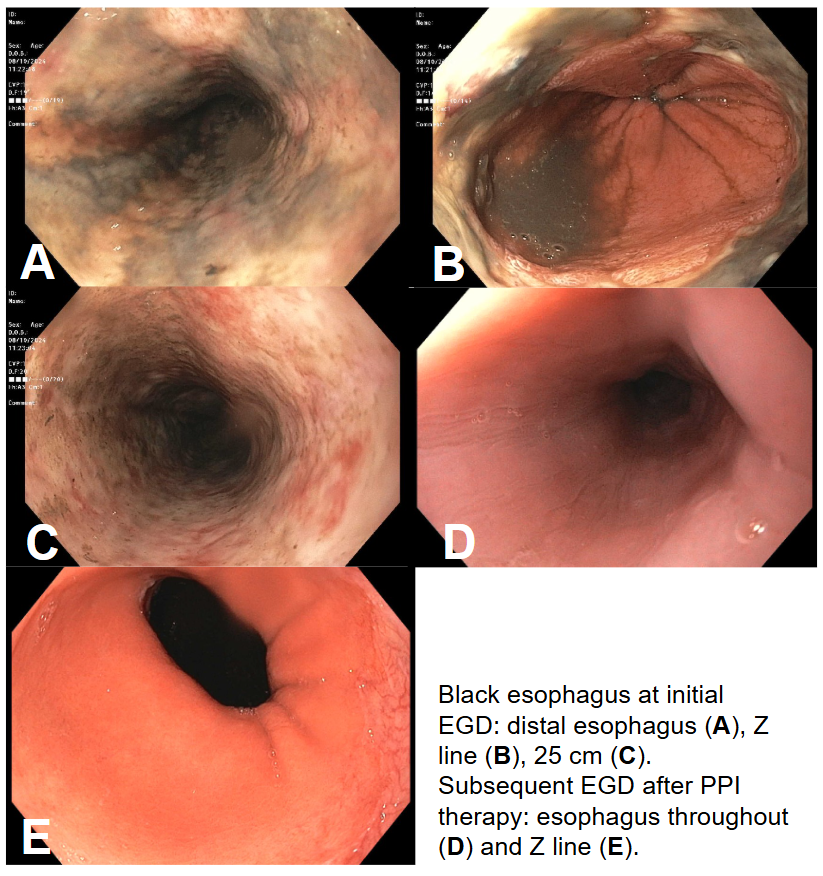
Figure: Black esophagus at initial EGD: distal esophagus (A), Z line (B), 25 cm (C). Subsequent EGD after PPI therapy: esophagus throughout (D) and Z line (E).
Disclosures:
Rebecca Beard indicated no relevant financial relationships.
Kathryn Driggers indicated no relevant financial relationships.
Henri De La Baume indicated no relevant financial relationships.
Rebecca Beard, 1, Kathryn Driggers, MD2, Henri De La Baume, MD3. P5051 - Black Esophagus: A Severely Morbid or Benign Finding?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
