Tuesday Poster Session
Category: Esophagus
P5050 - Acute Esophageal Necrosis in the Setting of Acute Gastric Volvulus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Naveen Mallangada, MD (he/him/his)
Robert Wood Johnson Medical School, Rutgers University
New Brunswick, NJ
Presenting Author(s)
Naveen Mallangada, MD1, Anish V. Patel, MD2
1Robert Wood Johnson Medical School, Rutgers University, Jericho, NY; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Acute Esophageal Necrosis (AEN), also called “black esophagus” or Gurvits syndrome, is a rare endoscopic finding featuring partial or circumferential black discoloration. It carries significant mortality (13-35%) due to complications such as esophageal perforation leading to sepsis, and hemorrhagic shock from active bleeding. It is associated with ischemic insult, chemic injury and infectious esophagitis.
Case Description/
Methods: An 89-year-old female with a known large hiatal hernia presented to the emergency department with hematemesis. Hemoglobin was 10.5 g/dL. CT angiogram of chest & abdomen revealed a large hiatal hernia with an intrathoracic stomach and organoaxial volvulus (Figure 1A). Patient was emergently brought to the operating room for endoscopic and possible surgical intervention. On endoscopy, there was blackening of the mid and distal esophagus with abrupt transition at the gastroesophageal junction, with friable mucosa and hemorrhagic esophagitis (Figure 1B) consistent with AEN. There was a spurting vessel in the distal esophagus that was treated with bipolar cautery. A 10 cm hiatal hernia was present and there was visualized detorsion of the acute gastric volvulus with gentle advancement of the endoscope. The gastro-duodenal mucosa was otherwise normal. The patient was transferred to the surgical intensive care unit on intravenous pantoprazole. Goals of care were discussed with the family, who deciding to pursue comfort measures over surgical intervention. The patient eventually passed away.
Discussion: We present a case of AEN with co-existent acute gastric volvulus (AGV). This is a very rare occurrence, with less than 10 cases reported in the literature. Urgent imaging should be performed in patients with known large hiatal hernia who present with acute symptoms such as hematemesis and epigastric pain. Early endoscopy is essential to establish a diagnosis of AEN and exclude gastric compromise. In our patient, the etiology of AEN was compromised blood flow due to AGV and gastric outlet obstruction. Surgical consultation is recommended, and early laparoscopic intervention on AGV can re-establish esophageal perfusion. Though our case ended with the patient passing after conservative management, it is important to identify AEN and AGV early, be aware of its rare co-existing presentation, determine utility of surgical intervention, and remain proactive with resuscitation efforts and medical therapies (proton pump inhibitor) to aid in esophageal reperfusion and recovery.
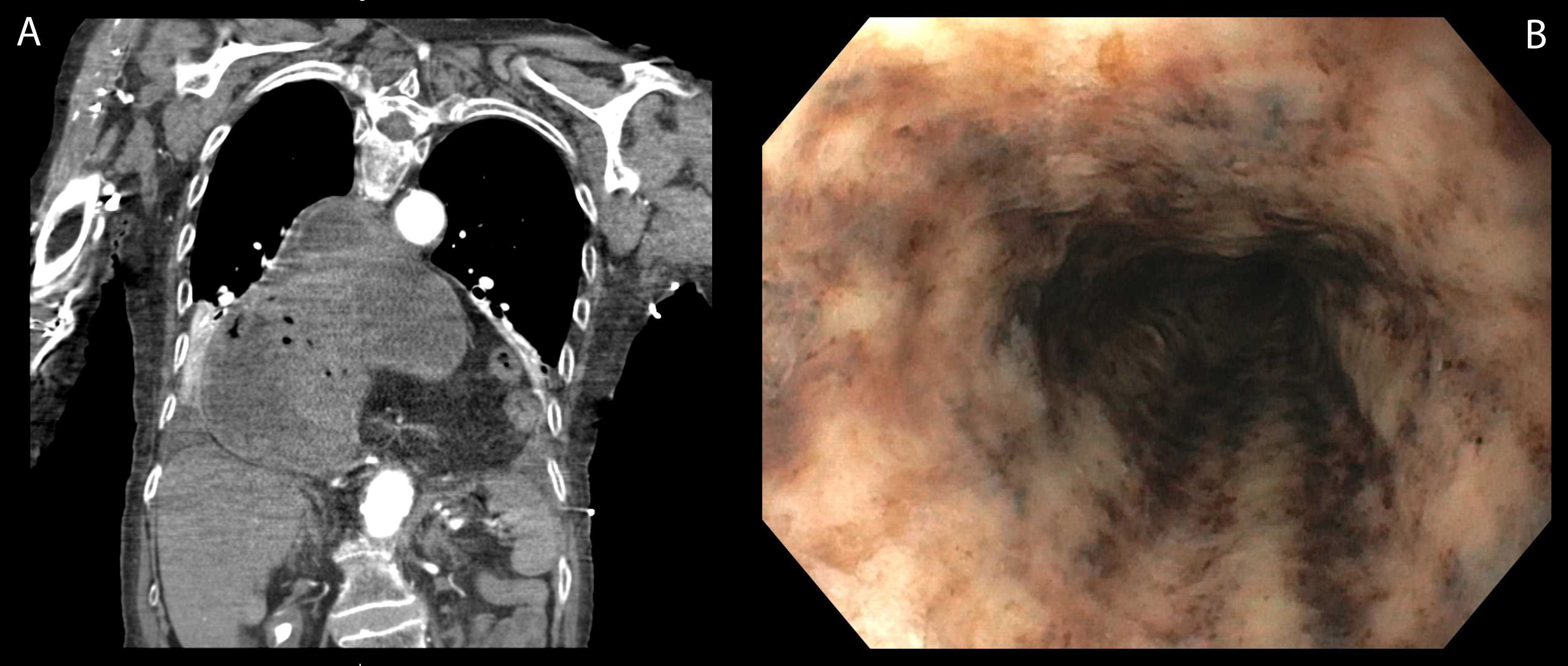
Figure: Image A: CT angiogram of chest & abdomen revealing a large hiatal hernia with an intrathoracic stomach and organoaxial volvulus; Image B: Endoscopic view detailing blackening of the mid and distal esophagus consistent with AEN.
Disclosures:
Naveen Mallangada indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Naveen Mallangada, MD1, Anish V. Patel, MD2. P5050 - Acute Esophageal Necrosis in the Setting of Acute Gastric Volvulus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Robert Wood Johnson Medical School, Rutgers University, Jericho, NY; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Acute Esophageal Necrosis (AEN), also called “black esophagus” or Gurvits syndrome, is a rare endoscopic finding featuring partial or circumferential black discoloration. It carries significant mortality (13-35%) due to complications such as esophageal perforation leading to sepsis, and hemorrhagic shock from active bleeding. It is associated with ischemic insult, chemic injury and infectious esophagitis.
Case Description/
Methods: An 89-year-old female with a known large hiatal hernia presented to the emergency department with hematemesis. Hemoglobin was 10.5 g/dL. CT angiogram of chest & abdomen revealed a large hiatal hernia with an intrathoracic stomach and organoaxial volvulus (Figure 1A). Patient was emergently brought to the operating room for endoscopic and possible surgical intervention. On endoscopy, there was blackening of the mid and distal esophagus with abrupt transition at the gastroesophageal junction, with friable mucosa and hemorrhagic esophagitis (Figure 1B) consistent with AEN. There was a spurting vessel in the distal esophagus that was treated with bipolar cautery. A 10 cm hiatal hernia was present and there was visualized detorsion of the acute gastric volvulus with gentle advancement of the endoscope. The gastro-duodenal mucosa was otherwise normal. The patient was transferred to the surgical intensive care unit on intravenous pantoprazole. Goals of care were discussed with the family, who deciding to pursue comfort measures over surgical intervention. The patient eventually passed away.
Discussion: We present a case of AEN with co-existent acute gastric volvulus (AGV). This is a very rare occurrence, with less than 10 cases reported in the literature. Urgent imaging should be performed in patients with known large hiatal hernia who present with acute symptoms such as hematemesis and epigastric pain. Early endoscopy is essential to establish a diagnosis of AEN and exclude gastric compromise. In our patient, the etiology of AEN was compromised blood flow due to AGV and gastric outlet obstruction. Surgical consultation is recommended, and early laparoscopic intervention on AGV can re-establish esophageal perfusion. Though our case ended with the patient passing after conservative management, it is important to identify AEN and AGV early, be aware of its rare co-existing presentation, determine utility of surgical intervention, and remain proactive with resuscitation efforts and medical therapies (proton pump inhibitor) to aid in esophageal reperfusion and recovery.
Figure: Image A: CT angiogram of chest & abdomen revealing a large hiatal hernia with an intrathoracic stomach and organoaxial volvulus; Image B: Endoscopic view detailing blackening of the mid and distal esophagus consistent with AEN.
Disclosures:
Naveen Mallangada indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Naveen Mallangada, MD1, Anish V. Patel, MD2. P5050 - Acute Esophageal Necrosis in the Setting of Acute Gastric Volvulus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
