Tuesday Poster Session
Category: Esophagus
P5049 - FLIP-Assisted Diagnosis and On-the-Spot Dilation of Achalasia With Inconclusive Manometry
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Wei Tang, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Wei Tang, MD1, Deepali Tewari, MD2, Sarah Rahni, DO, MBA1, Virendra Tewari, MBBS, MD, DM, FACG2
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
Introduction: The functional lumen imaging probe (FLIP) is a novel technology that utilizes high-resolution impedance planimetry during volume-controlled distension to assess esophageal cross-sectional area and distensibility. Endoluminal FLIP (EndoFLIP) aids in diagnosing motility disorders, while therapeutic FLIP (EsoFLIP) enables guided dilation. We present a case of achalasia with inconclusive high-resolution impedance manometry (HRIM), conclusively diagnosed using EndoFLIP and treated with EsoFLIP in the same session.
Case Description/
Methods: A 77-year-old man with a history of GERD and remotely cured tonsil cancer presented with progressive dysphagia to solids and liquids. A barium swallow performed on symptom onset 18 months prior showed mild cricopharyngeal narrowing. Speech and swallow evaluation ruled out oropharyngeal dysphagia. Over the past 8 months, his symptoms worsened with10-pound weight loss. EGD revealed a tight esophagogastric junction (EGJ) and punctate esophageal white plaques; biopsy confirmed Candida esophagitis. Symptoms persisted despite antifungal therapy. High-resolution impedance manometry (HRIM) showed absent esophageal pressurization, and no peristalsis but was inconclusive due to undiscernible esophageal sphincters (Fig. 1).
The patient then underwent EndoFLIP evaluation. A 16-cm EndoFLIP catheter was inserted with the balloon traversing the EGJ (Fig. 2A-B). Standard volumetric distension protocol was used. At successive 10-mL increments, measurements of diameter (mm), distensibility index (DI, mm2/mmHg), and pressure (mmHg) were as follows: 40 mL (4, 1.0, 12.3), 50 mL (6.3, 1.8, 17.8), 60 mL (9.7, 3.0, 24.9), and 70 mL (14.5, 3.8, 43.2). The absence of contractile activity (Fig. 2E) and low EGJ-DI confirmed type I achalasia. Subsequently, an EsoFLIP dilation catheter was used (Fig. 2C), a 30 mm stepwise balloon was introduced, dilating to a diameter of 30 mm (Fig 2D). The patient tolerated the procedure well and experienced marked improvement in symptoms.
Discussion: FLIP aids in diagnosing esophageal motility disorders diagnosis particularly when manometry is inconclusive and offers additional advantages of immediate therapeutic dilation using EsoFLIP. Unlike single size pneumatic dilation, EsoFLIP allows for real-time, gradual dilation with precision without fluoroscopy, improving safety. This case highlights FLIP’s dual utility and its expanding role in frontline management of esophageal dysphagia and motility disorders.
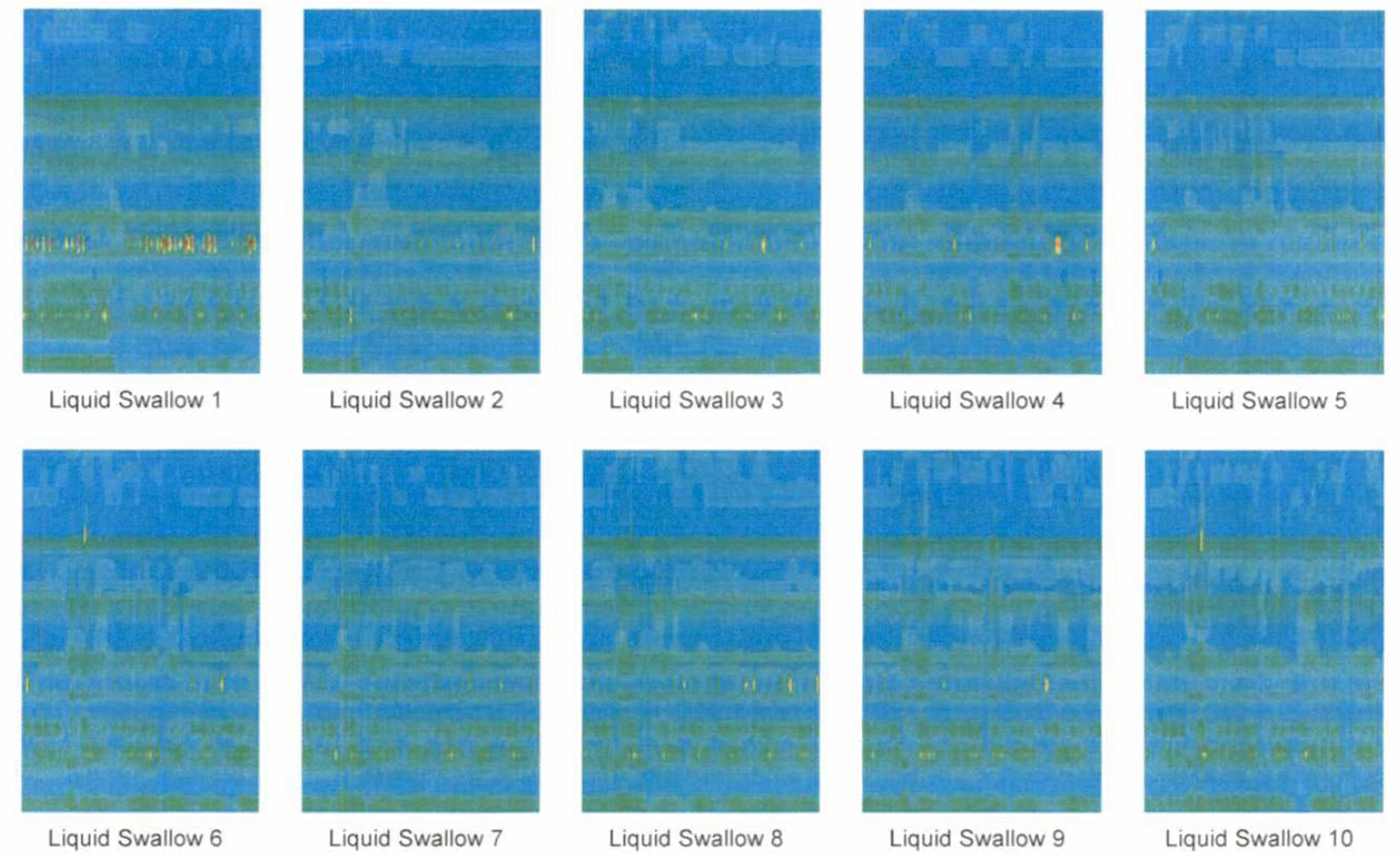
Figure: Figure 1. Absent Esophageal Pressurization and Peristalsis on Manometry.
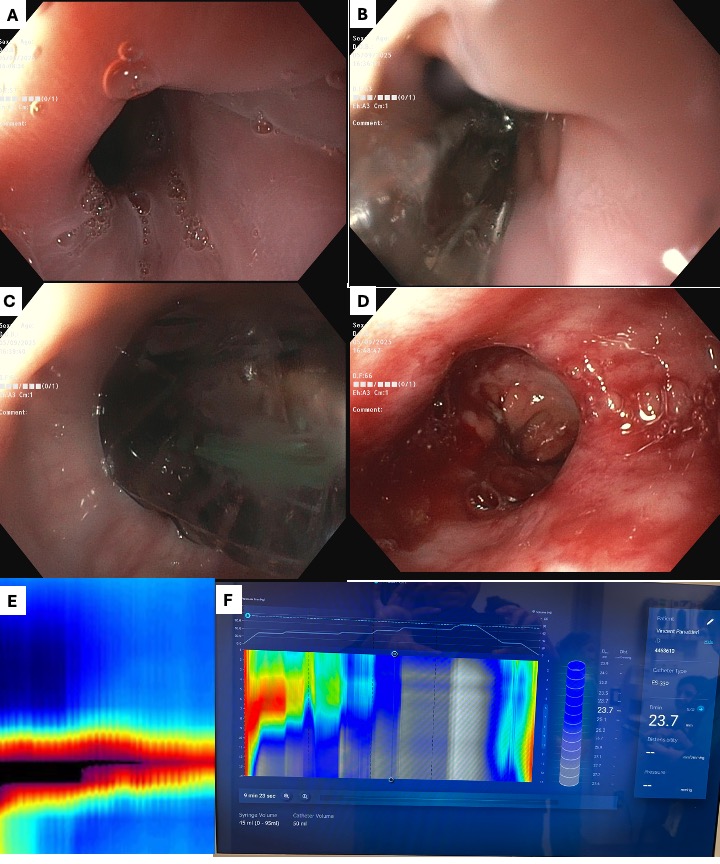
Figure: Figure 2. Diagnosis and Therapeutic Intervention Using the Functional Lumen Imaging Probe (FLIP) Technology.
A tight GEJ was identified on EGD (A). A 16-cm EndoFLIP catheter was inserted with the balloon traversing the GEJ (B). Standard volumetric distension protocol was used, and achalasia was diagnosed based on the absence of contractility response (E) and low EGJ-DI. Immediately following diagnosis, an EsoFLIP balloon dilation catheter was switched in (C), and a 30mm stepwise balloon was introduced for dilation reaching a final diameter of 30 mm (D) under FLIP guidance (F).
Disclosures:
Wei Tang indicated no relevant financial relationships.
Deepali Tewari indicated no relevant financial relationships.
Sarah Rahni indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Wei Tang, MD1, Deepali Tewari, MD2, Sarah Rahni, DO, MBA1, Virendra Tewari, MBBS, MD, DM, FACG2. P5049 - FLIP-Assisted Diagnosis and On-the-Spot Dilation of Achalasia With Inconclusive Manometry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
Introduction: The functional lumen imaging probe (FLIP) is a novel technology that utilizes high-resolution impedance planimetry during volume-controlled distension to assess esophageal cross-sectional area and distensibility. Endoluminal FLIP (EndoFLIP) aids in diagnosing motility disorders, while therapeutic FLIP (EsoFLIP) enables guided dilation. We present a case of achalasia with inconclusive high-resolution impedance manometry (HRIM), conclusively diagnosed using EndoFLIP and treated with EsoFLIP in the same session.
Case Description/
Methods: A 77-year-old man with a history of GERD and remotely cured tonsil cancer presented with progressive dysphagia to solids and liquids. A barium swallow performed on symptom onset 18 months prior showed mild cricopharyngeal narrowing. Speech and swallow evaluation ruled out oropharyngeal dysphagia. Over the past 8 months, his symptoms worsened with10-pound weight loss. EGD revealed a tight esophagogastric junction (EGJ) and punctate esophageal white plaques; biopsy confirmed Candida esophagitis. Symptoms persisted despite antifungal therapy. High-resolution impedance manometry (HRIM) showed absent esophageal pressurization, and no peristalsis but was inconclusive due to undiscernible esophageal sphincters (Fig. 1).
The patient then underwent EndoFLIP evaluation. A 16-cm EndoFLIP catheter was inserted with the balloon traversing the EGJ (Fig. 2A-B). Standard volumetric distension protocol was used. At successive 10-mL increments, measurements of diameter (mm), distensibility index (DI, mm2/mmHg), and pressure (mmHg) were as follows: 40 mL (4, 1.0, 12.3), 50 mL (6.3, 1.8, 17.8), 60 mL (9.7, 3.0, 24.9), and 70 mL (14.5, 3.8, 43.2). The absence of contractile activity (Fig. 2E) and low EGJ-DI confirmed type I achalasia. Subsequently, an EsoFLIP dilation catheter was used (Fig. 2C), a 30 mm stepwise balloon was introduced, dilating to a diameter of 30 mm (Fig 2D). The patient tolerated the procedure well and experienced marked improvement in symptoms.
Discussion: FLIP aids in diagnosing esophageal motility disorders diagnosis particularly when manometry is inconclusive and offers additional advantages of immediate therapeutic dilation using EsoFLIP. Unlike single size pneumatic dilation, EsoFLIP allows for real-time, gradual dilation with precision without fluoroscopy, improving safety. This case highlights FLIP’s dual utility and its expanding role in frontline management of esophageal dysphagia and motility disorders.
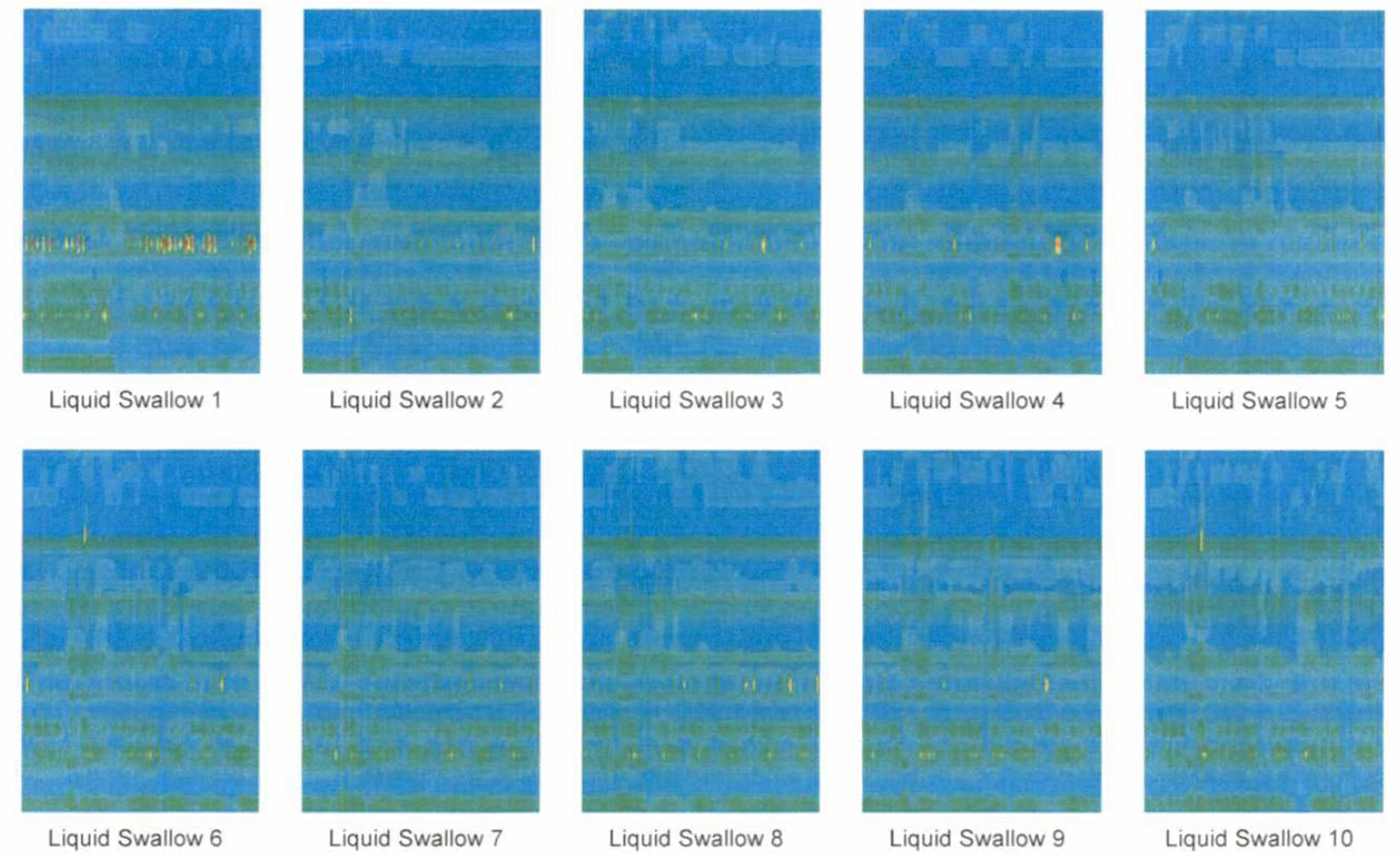
Figure: Figure 1. Absent Esophageal Pressurization and Peristalsis on Manometry.
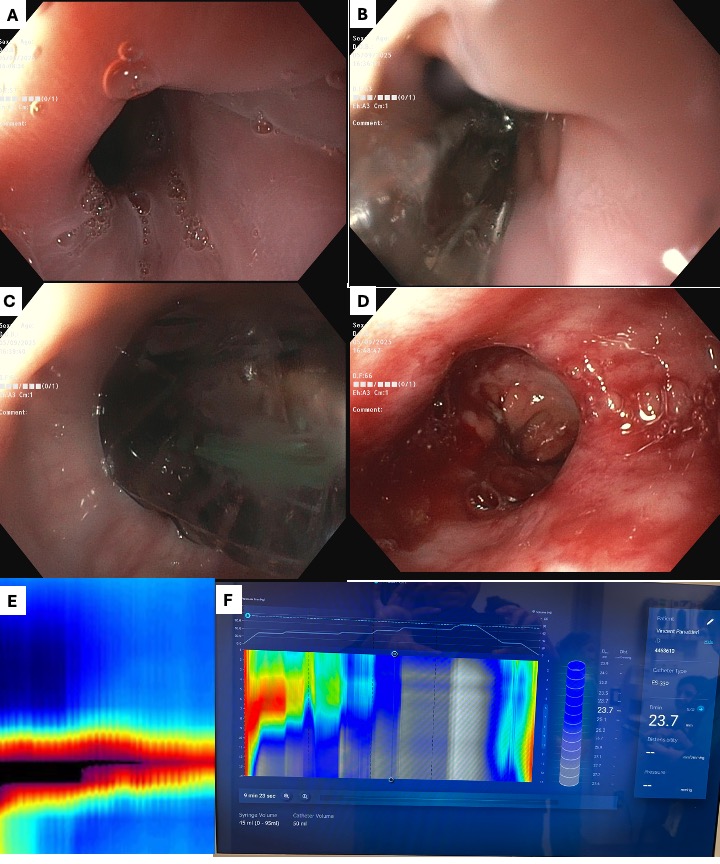
Figure: Figure 2. Diagnosis and Therapeutic Intervention Using the Functional Lumen Imaging Probe (FLIP) Technology.
A tight GEJ was identified on EGD (A). A 16-cm EndoFLIP catheter was inserted with the balloon traversing the GEJ (B). Standard volumetric distension protocol was used, and achalasia was diagnosed based on the absence of contractility response (E) and low EGJ-DI. Immediately following diagnosis, an EsoFLIP balloon dilation catheter was switched in (C), and a 30mm stepwise balloon was introduced for dilation reaching a final diameter of 30 mm (D) under FLIP guidance (F).
Disclosures:
Wei Tang indicated no relevant financial relationships.
Deepali Tewari indicated no relevant financial relationships.
Sarah Rahni indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Wei Tang, MD1, Deepali Tewari, MD2, Sarah Rahni, DO, MBA1, Virendra Tewari, MBBS, MD, DM, FACG2. P5049 - FLIP-Assisted Diagnosis and On-the-Spot Dilation of Achalasia With Inconclusive Manometry, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

