Tuesday Poster Session
Category: Esophagus
P5038 - Breaking Through the Mucosal Wall: Topical Tacrolimus for Refractory Esophageal Lichen Planus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jared Fehlman, MD (he/him/his)
Huntington Hospital
Pasadena, CA
Presenting Author(s)
Jared Fehlman, MD1, Nicha Wongjarupong, MD2, Ali Rezaie, MD, MSc2, Brent Larson, DO2, Michael Kozak, DO2, Amrit K. Kamboj, MD2
1Huntington Hospital, Pasadena, CA; 2Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Lichen planus is a chronic inflammatory disorder that commonly affects the skin and mucosal surfaces such as the mouth, larynx, genitals, and esophagus. Isolated esophageal lichen planus (ELP) is an under-recognized and frequently misdiagnosed condition, given the absence of cutaneous manifestations and nonspecific esophageal symptoms. While topical corticosteroids are often utilized as first-line treatment, there is a paucity of literature on management of refractory ELP that does not respond to initial therapy.
Case Description/
Methods: A 63-year-old woman presented with a 6-year history of worsening odynophagia and dysphagia. Initial esophagogastroduodenoscopy (EGD) showed diffusely narrow esophagus with an inner diameter of 10 mm with severely congested and crepe paper-like mucosa [Figure 1a, 1b, 1c]. Biopsies showed lymphocyte-predominant esophagitis with ulceration and dyskeratosis with negative stains for fungal and viral organisms [Figure 1d, 1e, 1f]. Given the high suspicion for ELP, our patient was referred to dermatology, ENT, and gynecology, and these evaluations were negative for extra-esophageal lichen planus. Over the subsequent months, the patient was trialed on approximately 12-week courses of the following: twice daily high-dose proton pump inhibitor (PPI), two different formulations of topical corticosteroids equivalent to budesonide 2 mg twice daily, oral tacrolimus 2 mg twice daily, and hydroxychloroquine 200 mg daily. These therapies resulted in no significant symptomatic or endoscopic improvement. She was then initiated on topical tacrolimus 1 mg twice daily. This was a compounded esophageal suspension with a ratio of 0.25 mg of tacrolimus powder and 1 mL of isomalt polymer water-soluble-base (MucoloxTM). After 3 months, her odynophagia and dysphagia significantly improved, as did the endoscopic findings, and endoscopic dilation could be performed to 14 mm with moderate mucosal disruption [Figure 2a, 2b]. The patient was maintained on topical tacrolimus at the same dose with close outpatient follow-up.
Discussion: This case serves to highlight severe ELP that did not respond to PPI, various formulations of topical corticosteroids, oral tacrolimus, and hydroxychloroquine. Fortunately, our patient had significant improvement both clinically and endoscopically after use of swallowed topical tacrolimus suspension. Given the difficulty of treating refractory ELP, this case may provide clinicians with another medication that may be utilized when other therapies have failed.
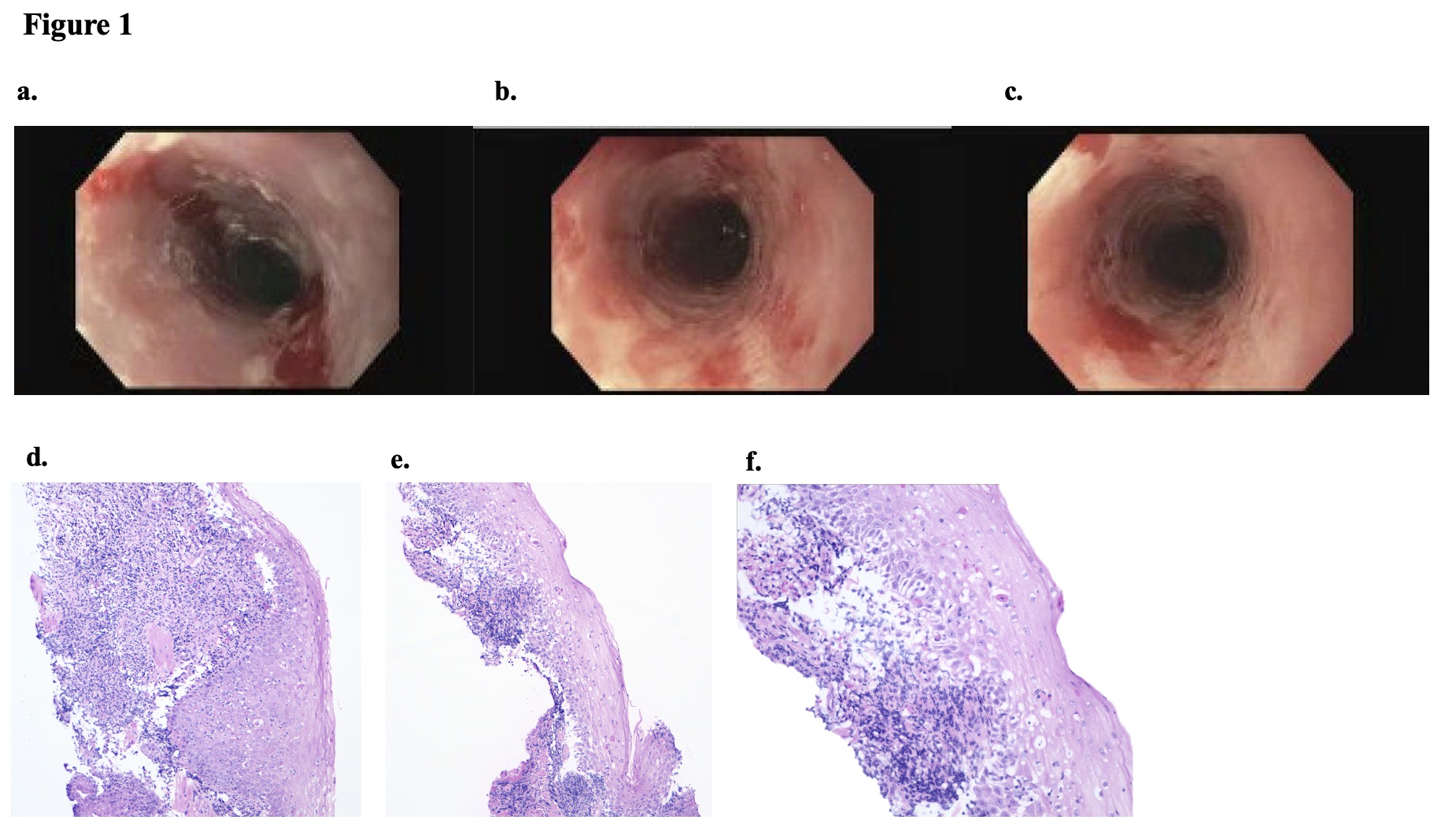
Figure: Figure 1: Initial endoscopic findings in the proximal (1a.), mid (1b.), and distal (1c.) esophagus and histopathology demonstrating lymphocyte predominant esophagitis with dyskeratotic cells (1d,1e,1f)
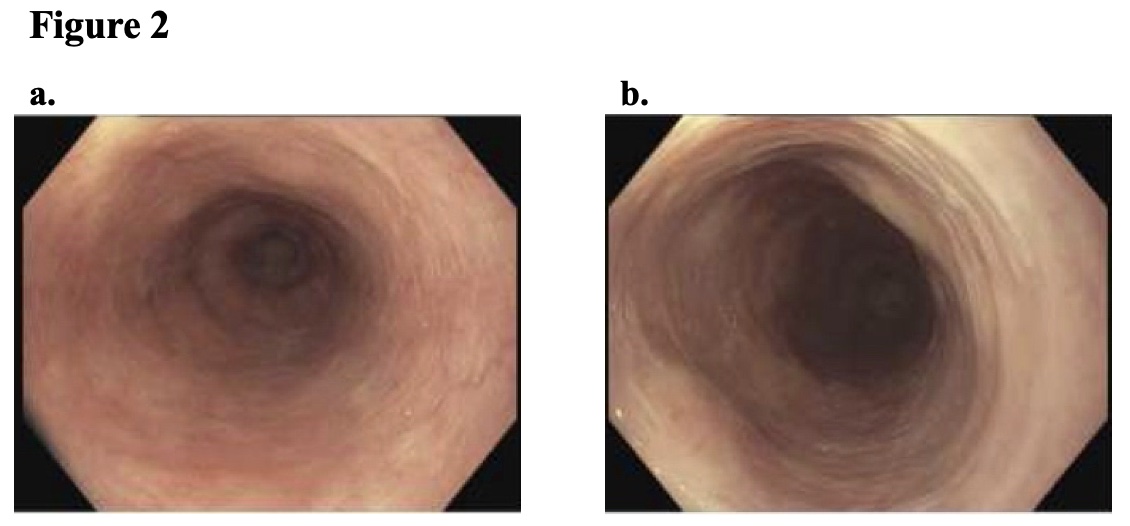
Figure: Figure 2. Follow up endoscopic findings after 3 months of esophageal suspension tacrolimus (2a, 2b)
Disclosures:
Jared Fehlman indicated no relevant financial relationships.
Nicha Wongjarupong indicated no relevant financial relationships.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Brent Larson indicated no relevant financial relationships.
Michael Kozak: Tempus AI – Stock-publicly held company(excluding mutual/index funds).
Amrit Kamboj: Sanofi – Speakers Bureau.
Jared Fehlman, MD1, Nicha Wongjarupong, MD2, Ali Rezaie, MD, MSc2, Brent Larson, DO2, Michael Kozak, DO2, Amrit K. Kamboj, MD2. P5038 - Breaking Through the Mucosal Wall: Topical Tacrolimus for Refractory Esophageal Lichen Planus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Huntington Hospital, Pasadena, CA; 2Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Lichen planus is a chronic inflammatory disorder that commonly affects the skin and mucosal surfaces such as the mouth, larynx, genitals, and esophagus. Isolated esophageal lichen planus (ELP) is an under-recognized and frequently misdiagnosed condition, given the absence of cutaneous manifestations and nonspecific esophageal symptoms. While topical corticosteroids are often utilized as first-line treatment, there is a paucity of literature on management of refractory ELP that does not respond to initial therapy.
Case Description/
Methods: A 63-year-old woman presented with a 6-year history of worsening odynophagia and dysphagia. Initial esophagogastroduodenoscopy (EGD) showed diffusely narrow esophagus with an inner diameter of 10 mm with severely congested and crepe paper-like mucosa [Figure 1a, 1b, 1c]. Biopsies showed lymphocyte-predominant esophagitis with ulceration and dyskeratosis with negative stains for fungal and viral organisms [Figure 1d, 1e, 1f]. Given the high suspicion for ELP, our patient was referred to dermatology, ENT, and gynecology, and these evaluations were negative for extra-esophageal lichen planus. Over the subsequent months, the patient was trialed on approximately 12-week courses of the following: twice daily high-dose proton pump inhibitor (PPI), two different formulations of topical corticosteroids equivalent to budesonide 2 mg twice daily, oral tacrolimus 2 mg twice daily, and hydroxychloroquine 200 mg daily. These therapies resulted in no significant symptomatic or endoscopic improvement. She was then initiated on topical tacrolimus 1 mg twice daily. This was a compounded esophageal suspension with a ratio of 0.25 mg of tacrolimus powder and 1 mL of isomalt polymer water-soluble-base (MucoloxTM). After 3 months, her odynophagia and dysphagia significantly improved, as did the endoscopic findings, and endoscopic dilation could be performed to 14 mm with moderate mucosal disruption [Figure 2a, 2b]. The patient was maintained on topical tacrolimus at the same dose with close outpatient follow-up.
Discussion: This case serves to highlight severe ELP that did not respond to PPI, various formulations of topical corticosteroids, oral tacrolimus, and hydroxychloroquine. Fortunately, our patient had significant improvement both clinically and endoscopically after use of swallowed topical tacrolimus suspension. Given the difficulty of treating refractory ELP, this case may provide clinicians with another medication that may be utilized when other therapies have failed.
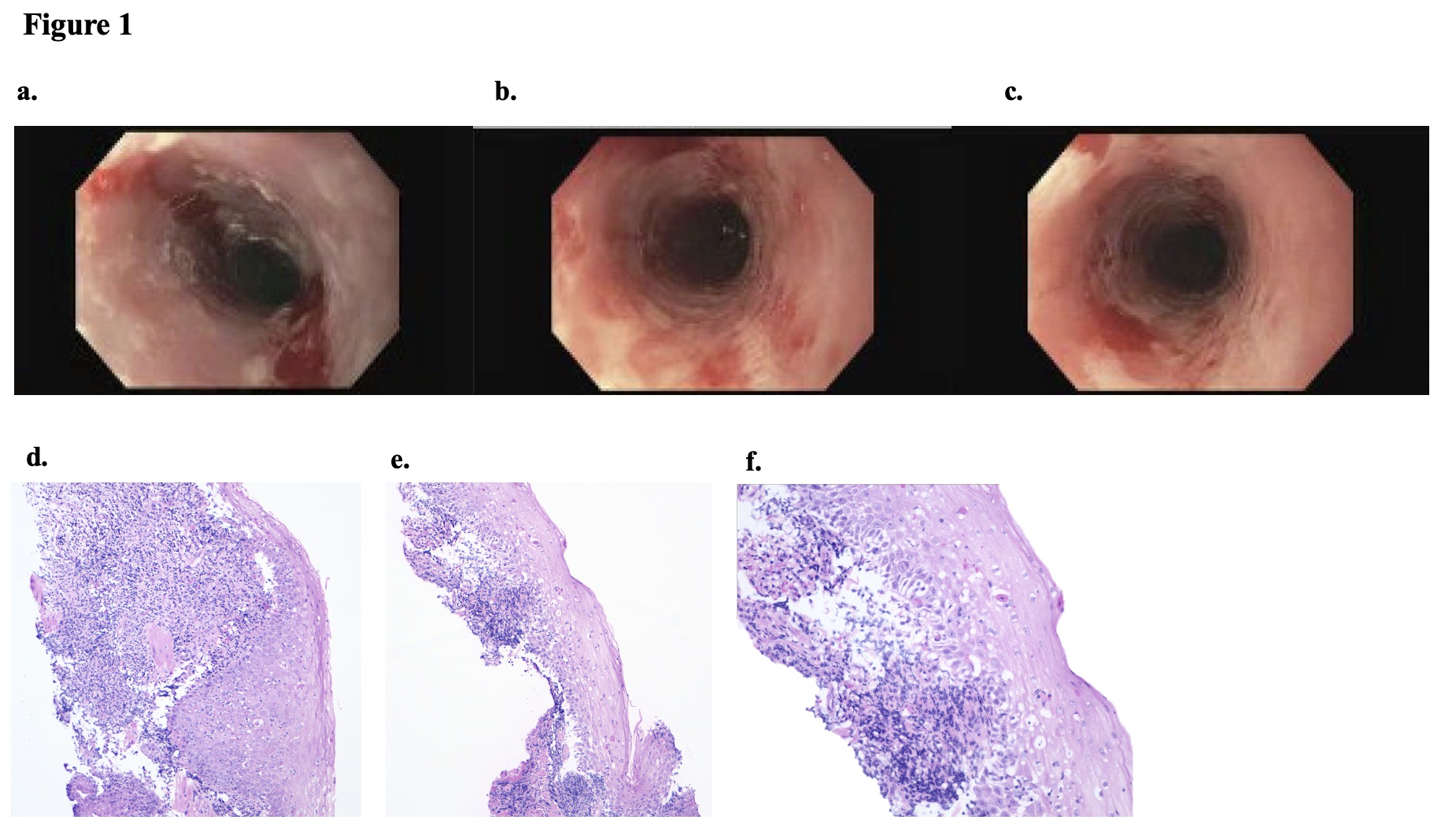
Figure: Figure 1: Initial endoscopic findings in the proximal (1a.), mid (1b.), and distal (1c.) esophagus and histopathology demonstrating lymphocyte predominant esophagitis with dyskeratotic cells (1d,1e,1f)
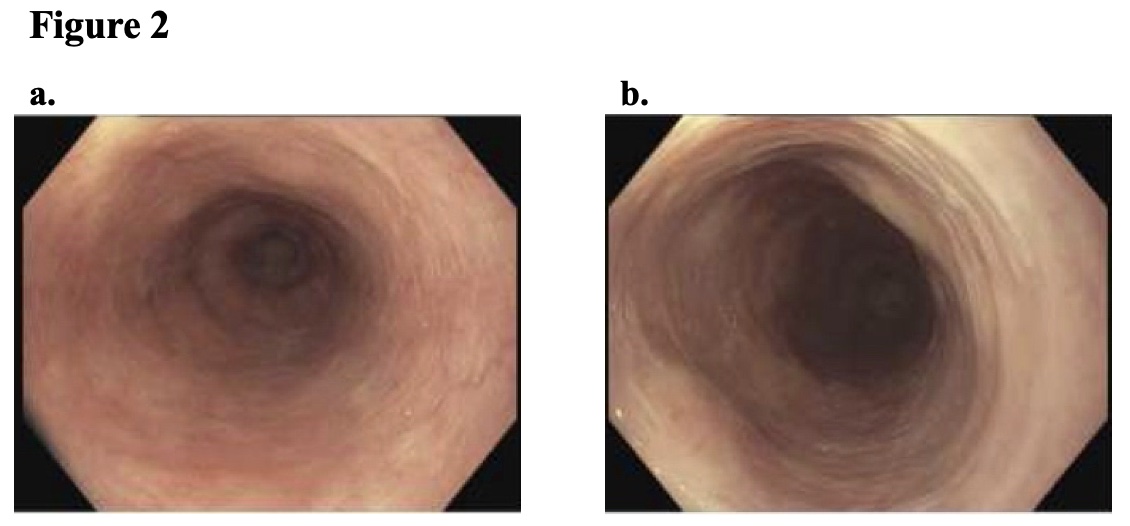
Figure: Figure 2. Follow up endoscopic findings after 3 months of esophageal suspension tacrolimus (2a, 2b)
Disclosures:
Jared Fehlman indicated no relevant financial relationships.
Nicha Wongjarupong indicated no relevant financial relationships.
Ali Rezaie: Ardelyx, Blueprint Medicine and Salix Pharmaceuticals – Consultant. Gemelli Biotech, and Good LFE – Equity stake.
Brent Larson indicated no relevant financial relationships.
Michael Kozak: Tempus AI – Stock-publicly held company(excluding mutual/index funds).
Amrit Kamboj: Sanofi – Speakers Bureau.
Jared Fehlman, MD1, Nicha Wongjarupong, MD2, Ali Rezaie, MD, MSc2, Brent Larson, DO2, Michael Kozak, DO2, Amrit K. Kamboj, MD2. P5038 - Breaking Through the Mucosal Wall: Topical Tacrolimus for Refractory Esophageal Lichen Planus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

