Tuesday Poster Session
Category: General Endoscopy
P5119 - Increased Mortality for Patients With Cirrhosis and Coagulopathy Undergoing Emergent EGD Receiving Pre-Procedure Fresh Frozen Plasma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Priyanka Jagannathan, MD
University of Texas at Austin
Austin, Texas
Presenting Author(s)
Priyanka Jagannathan, MD1, Mahnoor Liaqat, MD2, Maria Goretti Ochi, MD2, Suhritha Bolisetty, MS3, Deepak Agrawal, MD, MPH1, David Tang, MD2, Cristal Brown, MD, MHS2
1University of Texas at Austin, Austin, TX; 2University of Texas at Austin Dell Medical School, Austin, TX; 3dell, Austin, TX
Introduction: Coagulopathy is common in patients with cirrhosis and AASLD guidelines discourage the use of fresh frozen plasma (FFP) before invasive procedures given its risks outweigh the benefits. Tests such as INR poorly predict bleeding risk in patients with advanced liver disease and transfusion of FFP carries risks including volume overload, transfusion reactions, and increased portal hypertension. However, its role specifically in patients with gastrointestinal bleeding undergoing emergent EGD remains more controversial. This study evaluated the effect of pre-procedure treatment with FFP on mortality in patients with cirrhosis and coagulopathy undergoing emergent endoscopy.
Methods: Retrospective cohort study of patients with cirrhosis and coagulopathy (INR≥1.5) seen in a multi-hospital system who underwent an emergent EGD between 2017-2019. Patients who received and did not receive pre-procedural FFP were compared. Primary outcome was 30-day mortality. Secondary outcomes were the rate of procedure-related bleeding, length of stay, ICU admission, and 30-day re-admission.
Statistical analyses were performed including multivariate regression analyses to adjust for baseline differences between the cohorts.
Results: In this cohort, 109 patients (40.5%) received pre-procedure FFP and 160 (59.4%) patients did not. Patients had similar demographics, CCI score, cirrhosis etiology but those who received FFP had slightly higher MELD and pre-procedure INR (Table 1). 30-day mortality was significantly higher in the FFP group (33.0% vs. 10.0%, p< 0.00001) which remained significant after multivariate analysis adjusting for confounding variables. Additionally, FFP administration was associated with longer hospital stays (8.8 vs. 5.8 days, p=0.0002) and increased ICU admissions (92.7% vs. 67.5%, p< 0.00001). There was no significant reduction in procedure-related bleeding (4.6% vs. 1.3%, p=0.12) or 30-day readmission rates (22.0% vs. 24.4%, p=0.77). Patients receiving FFP had higher rates of liver-related deaths (77.8% vs 43.6%, p=0.025).
Discussion: Pre-procedural FFP administration in patients with cirrhosis undergoing emergent EGD was associated with higher mortality, increased length of stay, and higher ICU admission rates, without reducing any bleeding complications. These findings highlight the lack of benefit and potential risks of FFP even in the setting of gastrointestinal bleeding.
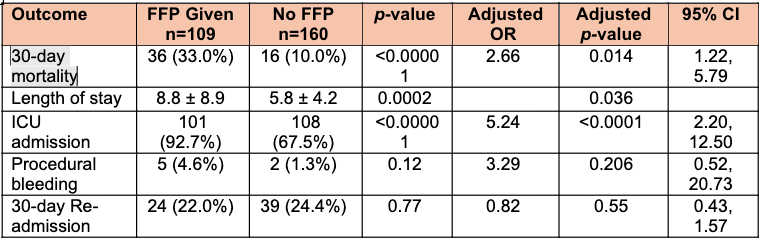
Figure: Patient demographics and features of cirrhosis including baseline admission data.
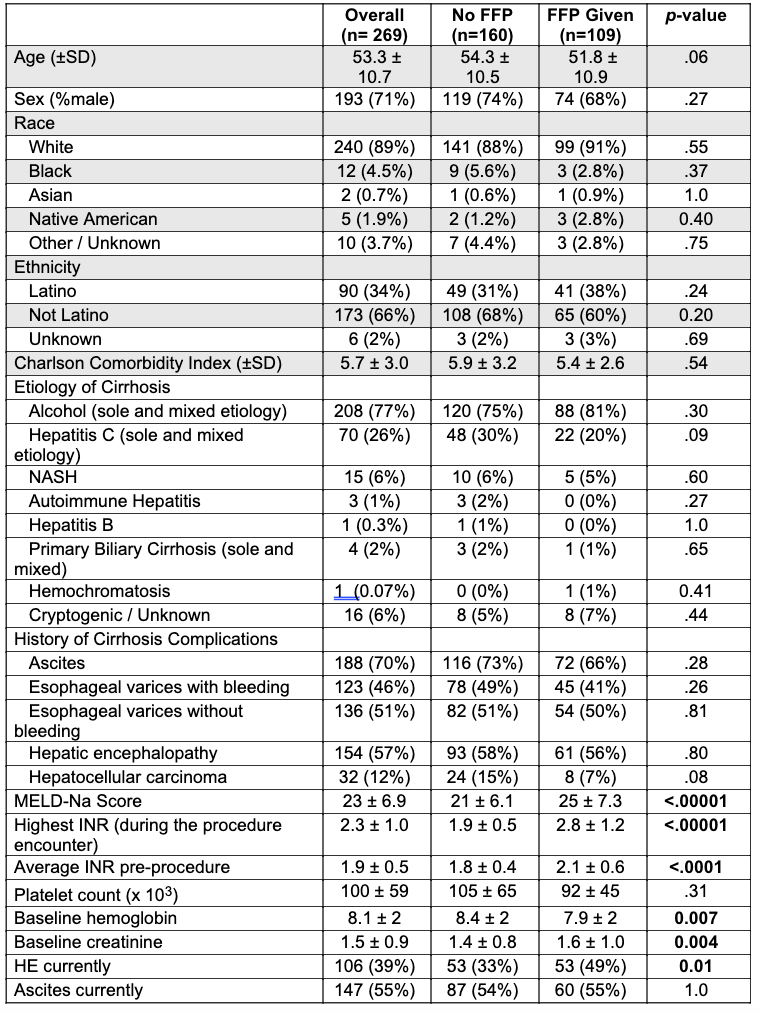
Figure: Univariate and multivariate regression analysis of the primary outcome, in hospital mortality, and the secondary outcomes.
Disclosures:
Priyanka Jagannathan indicated no relevant financial relationships.
Mahnoor Liaqat indicated no relevant financial relationships.
Maria Goretti Ochi indicated no relevant financial relationships.
Suhritha Bolisetty indicated no relevant financial relationships.
Deepak Agrawal indicated no relevant financial relationships.
David Tang indicated no relevant financial relationships.
Cristal Brown indicated no relevant financial relationships.
Priyanka Jagannathan, MD1, Mahnoor Liaqat, MD2, Maria Goretti Ochi, MD2, Suhritha Bolisetty, MS3, Deepak Agrawal, MD, MPH1, David Tang, MD2, Cristal Brown, MD, MHS2. P5119 - Increased Mortality for Patients With Cirrhosis and Coagulopathy Undergoing Emergent EGD Receiving Pre-Procedure Fresh Frozen Plasma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Austin, Austin, TX; 2University of Texas at Austin Dell Medical School, Austin, TX; 3dell, Austin, TX
Introduction: Coagulopathy is common in patients with cirrhosis and AASLD guidelines discourage the use of fresh frozen plasma (FFP) before invasive procedures given its risks outweigh the benefits. Tests such as INR poorly predict bleeding risk in patients with advanced liver disease and transfusion of FFP carries risks including volume overload, transfusion reactions, and increased portal hypertension. However, its role specifically in patients with gastrointestinal bleeding undergoing emergent EGD remains more controversial. This study evaluated the effect of pre-procedure treatment with FFP on mortality in patients with cirrhosis and coagulopathy undergoing emergent endoscopy.
Methods: Retrospective cohort study of patients with cirrhosis and coagulopathy (INR≥1.5) seen in a multi-hospital system who underwent an emergent EGD between 2017-2019. Patients who received and did not receive pre-procedural FFP were compared. Primary outcome was 30-day mortality. Secondary outcomes were the rate of procedure-related bleeding, length of stay, ICU admission, and 30-day re-admission.
Statistical analyses were performed including multivariate regression analyses to adjust for baseline differences between the cohorts.
Results: In this cohort, 109 patients (40.5%) received pre-procedure FFP and 160 (59.4%) patients did not. Patients had similar demographics, CCI score, cirrhosis etiology but those who received FFP had slightly higher MELD and pre-procedure INR (Table 1). 30-day mortality was significantly higher in the FFP group (33.0% vs. 10.0%, p< 0.00001) which remained significant after multivariate analysis adjusting for confounding variables. Additionally, FFP administration was associated with longer hospital stays (8.8 vs. 5.8 days, p=0.0002) and increased ICU admissions (92.7% vs. 67.5%, p< 0.00001). There was no significant reduction in procedure-related bleeding (4.6% vs. 1.3%, p=0.12) or 30-day readmission rates (22.0% vs. 24.4%, p=0.77). Patients receiving FFP had higher rates of liver-related deaths (77.8% vs 43.6%, p=0.025).
Discussion: Pre-procedural FFP administration in patients with cirrhosis undergoing emergent EGD was associated with higher mortality, increased length of stay, and higher ICU admission rates, without reducing any bleeding complications. These findings highlight the lack of benefit and potential risks of FFP even in the setting of gastrointestinal bleeding.
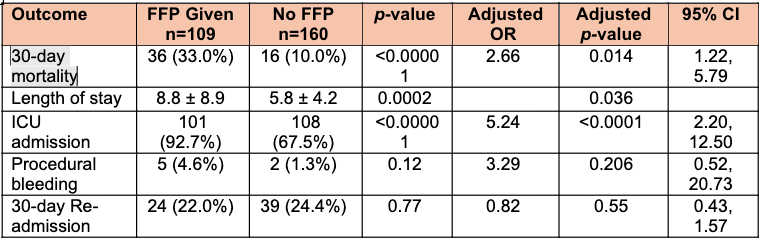
Figure: Patient demographics and features of cirrhosis including baseline admission data.
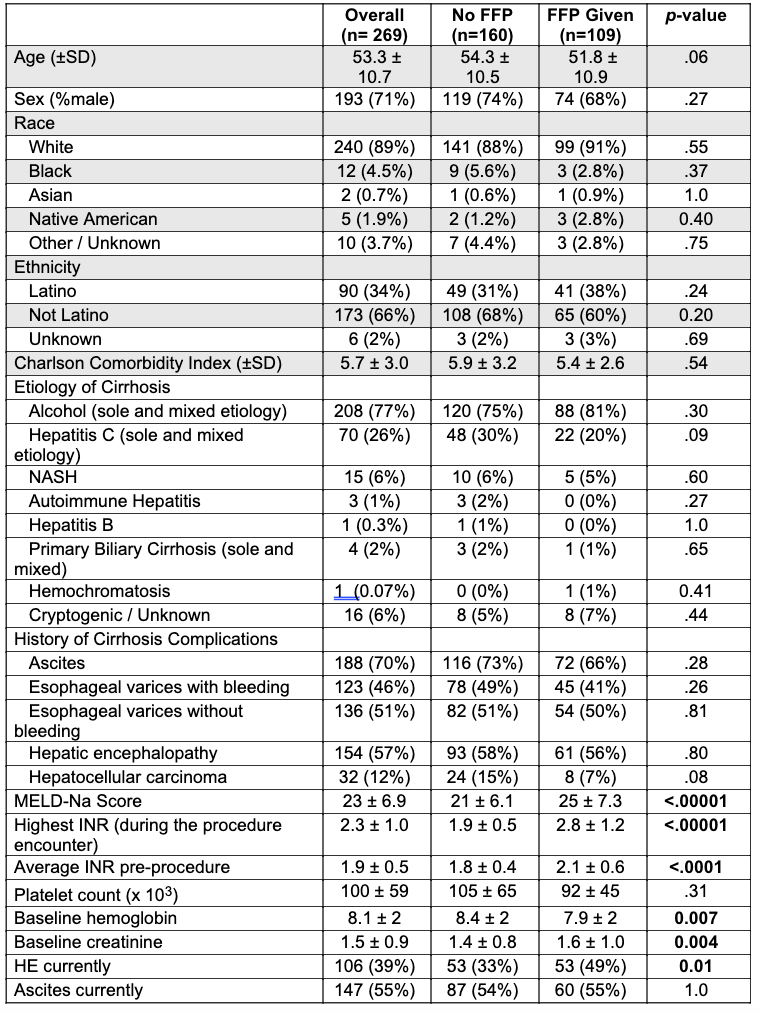
Figure: Univariate and multivariate regression analysis of the primary outcome, in hospital mortality, and the secondary outcomes.
Disclosures:
Priyanka Jagannathan indicated no relevant financial relationships.
Mahnoor Liaqat indicated no relevant financial relationships.
Maria Goretti Ochi indicated no relevant financial relationships.
Suhritha Bolisetty indicated no relevant financial relationships.
Deepak Agrawal indicated no relevant financial relationships.
David Tang indicated no relevant financial relationships.
Cristal Brown indicated no relevant financial relationships.
Priyanka Jagannathan, MD1, Mahnoor Liaqat, MD2, Maria Goretti Ochi, MD2, Suhritha Bolisetty, MS3, Deepak Agrawal, MD, MPH1, David Tang, MD2, Cristal Brown, MD, MHS2. P5119 - Increased Mortality for Patients With Cirrhosis and Coagulopathy Undergoing Emergent EGD Receiving Pre-Procedure Fresh Frozen Plasma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

