Tuesday Poster Session
Category: General Endoscopy
P5117 - High-Flow Nasal Cannula vs Standard Nasal Cannula for Hypoxemia Prevention in Upper Gastrointestinal Endoscopy: A Meta-Analysis of 15 Randomized Controlled Trials
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DP
Deipthan Prabakar, MD (he/him/his)
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Award: ACG Presidential Poster Award
Deipthan Prabakar, MD1, Vaishnavi Sabesan, MD1, Maryam Abbas Malik, MD2, Abirami Rajendiran, MD1, Bansi Sutariya, MD1, Babu P. Mohan, MD3, Sandesh Murali, MD1, Sherif E. Elhanafi, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 3Orlando Gastroenterology PA, Orlando, FL
Introduction: Hypoxemia during sedated upper gastrointestinal (GI) endoscopy remains a common and potentially serious complication, particularly among high-risk patients. High-flow nasal cannula (HFNC) therapy has emerged as a promising alternative to conventional nasal cannula (NC) oxygen delivery. We conducted a comprehensive meta-analysis of randomized controlled trials (RCTs) to evaluate whether HFNC reduces intraprocedural hypoxemia and related adverse outcomes.
Methods: We systematically searched PubMed, EMBASE, Cochrane, Scopus, and Google Scholar through May 2025 for RCTs comparing HFNC versus NC during sedated upper GI endoscopy in adults. The primary outcome was incidence of hypoxemia (SpO₂ < 90%). Secondary outcomes included procedural interruption, minimum SpO₂, and need for rescue intervention. Pooled risk ratios (RR) or mean differences (MD) were calculated using random-effects models. Heterogeneity was assessed with I² statistics; funnel plots were used to assess publication bias.
Results: Fifteen RCTs (n=3,873) met inclusion criteria. Mean age ranged from 43–72 years and BMI from 22–38 kg/m², with several trials enrolling elderly or obese patients. Cardiopulmonary comorbidities including COPD, asthma, and heart failure were either excluded or balanced across groups. HFNC significantly reduced hypoxemia events compared to NC (RR 0.11; 95% CI, 0.07–0.17; I²=0%). HFNC was associated with a higher mean minimum SpO₂ (MD +4.73%; 95% CI, 3.86–5.61; I²=89%) and lower risk of procedural interruption (RR 0.11; 95% CI, 0.04–0.28; I²=0%) and rescue intervention (RR 0.12; 95% CI, 0.07–0.22; I²=0%). Subgroup analyses showed consistent benefit across both high-risk and general populations. HFNC reduced hypoxemia in high-risk (RR 0.12, 95% CI 0.07–0.20) and general (RR 0.07, 95% CI 0.03–0.18) cohorts; procedural interruption was also reduced in high-risk (RR 0.08, 95% CI 0.02–0.44) and general populations (RR 0.14, 95% CI 0.05–0.38). Rescue intervention rates were similarly lower for high-risk (RR 0.13, 95% CI 0.06–0.28) and general (RR 0.09, 95% CI 0.04–0.24) groups. Minimum SpO₂ improved in both subgroups (high-risk: MD +4.60%; general: MD +4.82%). No evidence of publication bias was observed.
Discussion: HFNC markedly reduces intraprocedural hypoxemia, procedural disruption, and need for rescue intervention during sedated upper GI endoscopy, with consistent benefit across risk strata. These findings support broader adoption of HFNC, particularly for high-risk patients, in sedated upper GI endoscopy.
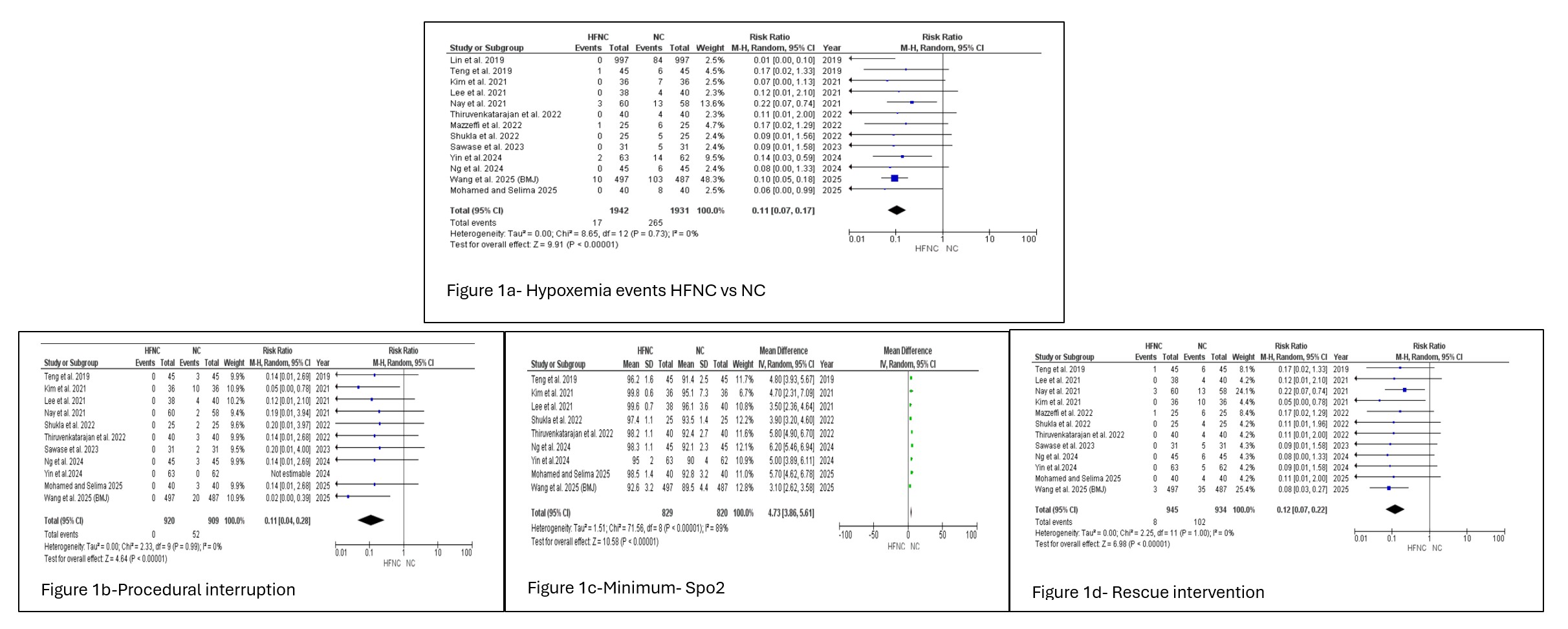
Figure: Figure 1. Pooled Outcomes Comparing HFNC vs. NC During Advanced Upper GI Endoscopy1a. Hypoxemia events (SpO₂ <90%), 1b. Procedural interruptions, 1c. Minimum SpO₂, 1d. Rescue interventions
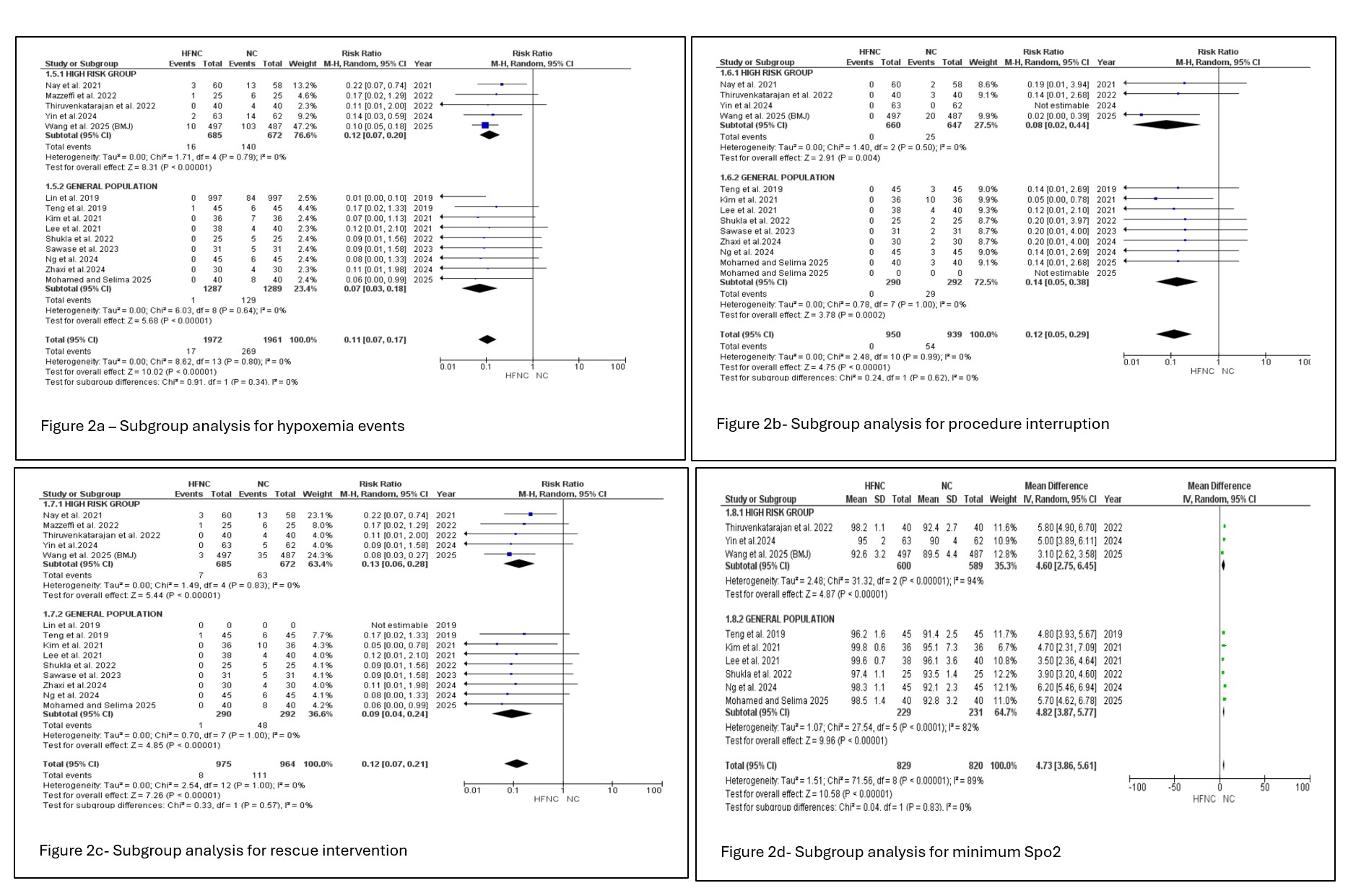
Figure: Figure 2. Subgroup analyses by risk group (high-risk vs. general population) for outcomes: minimum SpO₂ (2a), procedural interruption (2b), rescue intervention (2c), and lowest SpO₂ (2d).
Disclosures:
Deipthan Prabakar indicated no relevant financial relationships.
Vaishnavi Sabesan indicated no relevant financial relationships.
Maryam Abbas Malik indicated no relevant financial relationships.
Abirami Rajendiran indicated no relevant financial relationships.
Bansi Sutariya indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Sandesh Murali indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Deipthan Prabakar, MD1, Vaishnavi Sabesan, MD1, Maryam Abbas Malik, MD2, Abirami Rajendiran, MD1, Bansi Sutariya, MD1, Babu P. Mohan, MD3, Sandesh Murali, MD1, Sherif E. Elhanafi, MD1. P5117 - High-Flow Nasal Cannula vs Standard Nasal Cannula for Hypoxemia Prevention in Upper Gastrointestinal Endoscopy: A Meta-Analysis of 15 Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Deipthan Prabakar, MD1, Vaishnavi Sabesan, MD1, Maryam Abbas Malik, MD2, Abirami Rajendiran, MD1, Bansi Sutariya, MD1, Babu P. Mohan, MD3, Sandesh Murali, MD1, Sherif E. Elhanafi, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Services Institute of Medical Sciences, Lahore, Punjab, Pakistan; 3Orlando Gastroenterology PA, Orlando, FL
Introduction: Hypoxemia during sedated upper gastrointestinal (GI) endoscopy remains a common and potentially serious complication, particularly among high-risk patients. High-flow nasal cannula (HFNC) therapy has emerged as a promising alternative to conventional nasal cannula (NC) oxygen delivery. We conducted a comprehensive meta-analysis of randomized controlled trials (RCTs) to evaluate whether HFNC reduces intraprocedural hypoxemia and related adverse outcomes.
Methods: We systematically searched PubMed, EMBASE, Cochrane, Scopus, and Google Scholar through May 2025 for RCTs comparing HFNC versus NC during sedated upper GI endoscopy in adults. The primary outcome was incidence of hypoxemia (SpO₂ < 90%). Secondary outcomes included procedural interruption, minimum SpO₂, and need for rescue intervention. Pooled risk ratios (RR) or mean differences (MD) were calculated using random-effects models. Heterogeneity was assessed with I² statistics; funnel plots were used to assess publication bias.
Results: Fifteen RCTs (n=3,873) met inclusion criteria. Mean age ranged from 43–72 years and BMI from 22–38 kg/m², with several trials enrolling elderly or obese patients. Cardiopulmonary comorbidities including COPD, asthma, and heart failure were either excluded or balanced across groups. HFNC significantly reduced hypoxemia events compared to NC (RR 0.11; 95% CI, 0.07–0.17; I²=0%). HFNC was associated with a higher mean minimum SpO₂ (MD +4.73%; 95% CI, 3.86–5.61; I²=89%) and lower risk of procedural interruption (RR 0.11; 95% CI, 0.04–0.28; I²=0%) and rescue intervention (RR 0.12; 95% CI, 0.07–0.22; I²=0%). Subgroup analyses showed consistent benefit across both high-risk and general populations. HFNC reduced hypoxemia in high-risk (RR 0.12, 95% CI 0.07–0.20) and general (RR 0.07, 95% CI 0.03–0.18) cohorts; procedural interruption was also reduced in high-risk (RR 0.08, 95% CI 0.02–0.44) and general populations (RR 0.14, 95% CI 0.05–0.38). Rescue intervention rates were similarly lower for high-risk (RR 0.13, 95% CI 0.06–0.28) and general (RR 0.09, 95% CI 0.04–0.24) groups. Minimum SpO₂ improved in both subgroups (high-risk: MD +4.60%; general: MD +4.82%). No evidence of publication bias was observed.
Discussion: HFNC markedly reduces intraprocedural hypoxemia, procedural disruption, and need for rescue intervention during sedated upper GI endoscopy, with consistent benefit across risk strata. These findings support broader adoption of HFNC, particularly for high-risk patients, in sedated upper GI endoscopy.
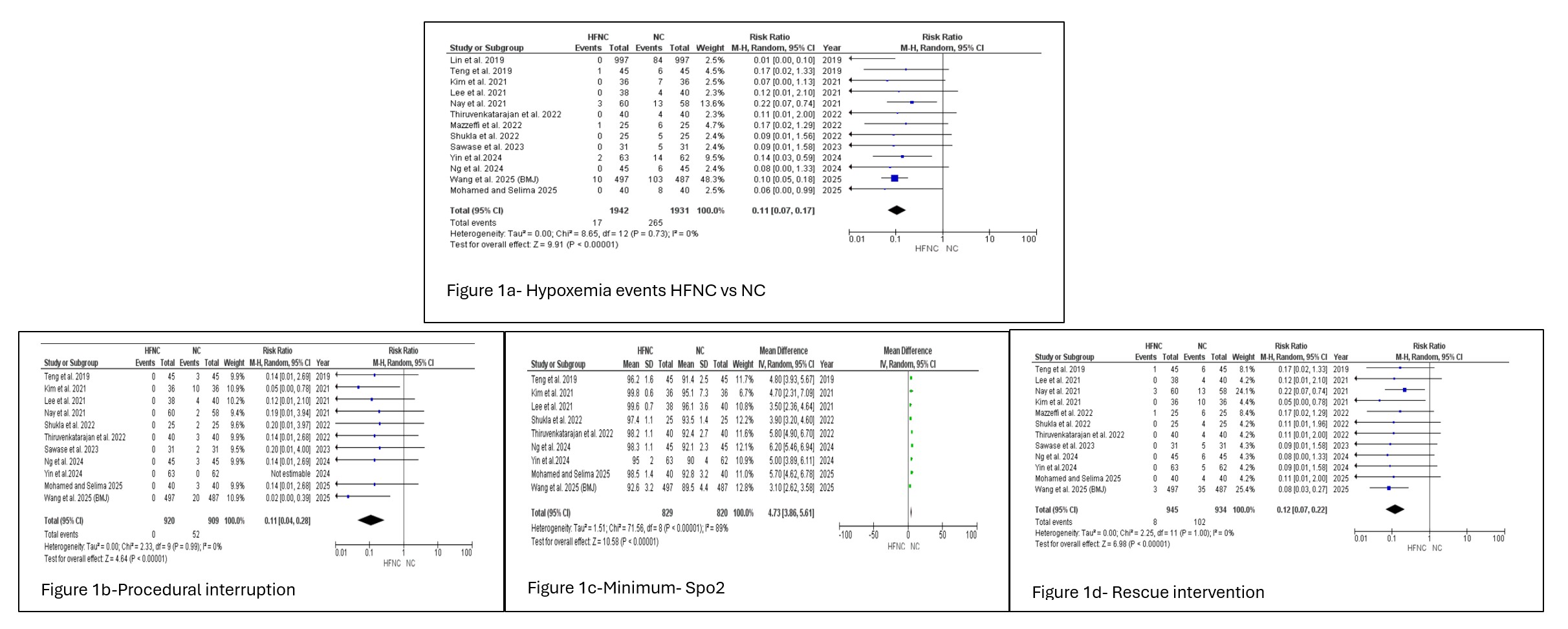
Figure: Figure 1. Pooled Outcomes Comparing HFNC vs. NC During Advanced Upper GI Endoscopy1a. Hypoxemia events (SpO₂ <90%), 1b. Procedural interruptions, 1c. Minimum SpO₂, 1d. Rescue interventions
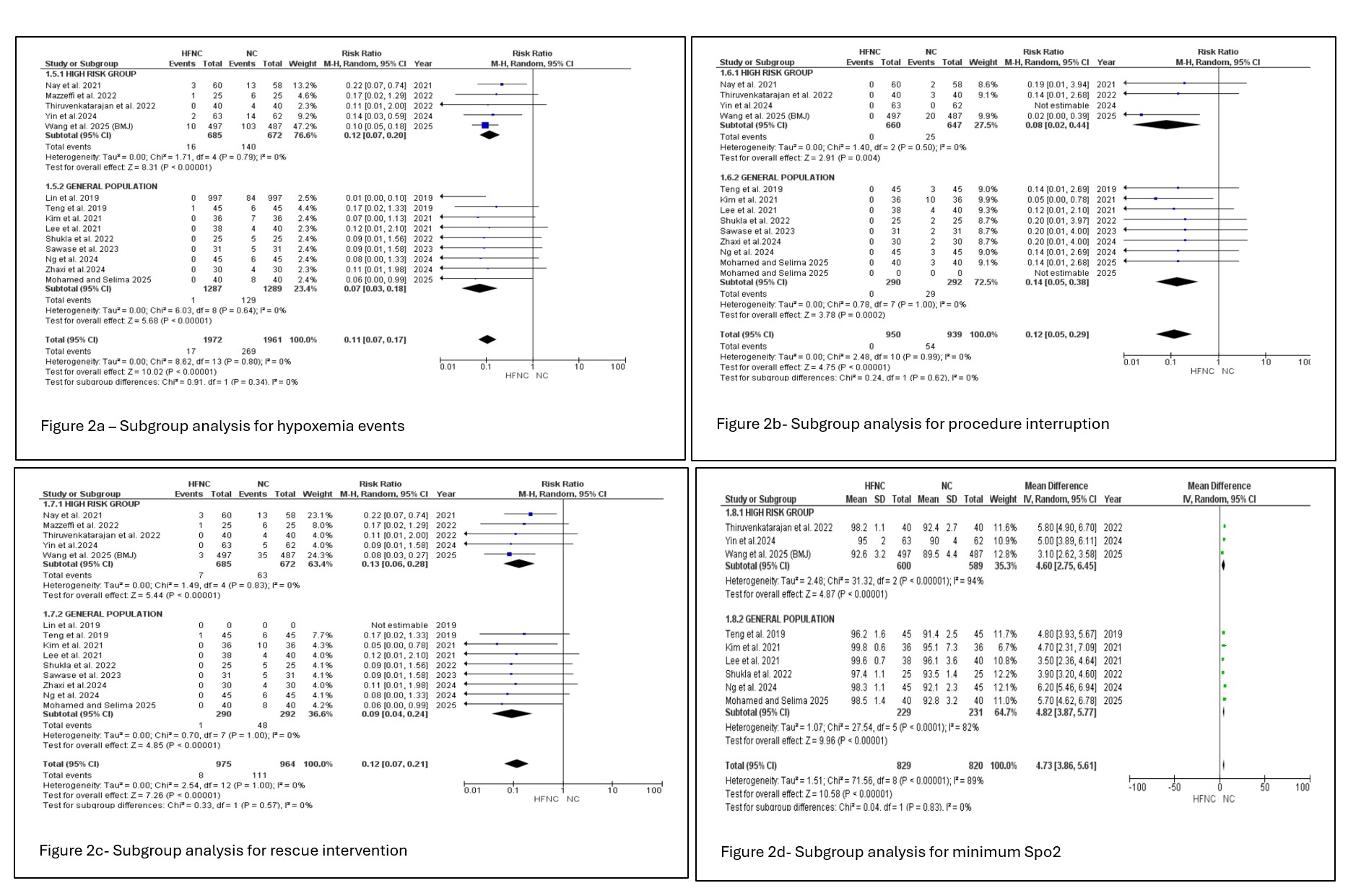
Figure: Figure 2. Subgroup analyses by risk group (high-risk vs. general population) for outcomes: minimum SpO₂ (2a), procedural interruption (2b), rescue intervention (2c), and lowest SpO₂ (2d).
Disclosures:
Deipthan Prabakar indicated no relevant financial relationships.
Vaishnavi Sabesan indicated no relevant financial relationships.
Maryam Abbas Malik indicated no relevant financial relationships.
Abirami Rajendiran indicated no relevant financial relationships.
Bansi Sutariya indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Sandesh Murali indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Deipthan Prabakar, MD1, Vaishnavi Sabesan, MD1, Maryam Abbas Malik, MD2, Abirami Rajendiran, MD1, Bansi Sutariya, MD1, Babu P. Mohan, MD3, Sandesh Murali, MD1, Sherif E. Elhanafi, MD1. P5117 - High-Flow Nasal Cannula vs Standard Nasal Cannula for Hypoxemia Prevention in Upper Gastrointestinal Endoscopy: A Meta-Analysis of 15 Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


