Tuesday Poster Session
Category: GI Bleeding
P5196 - Can Uncontrolled Hypertension Cause Diverticular Hemorrhage? A Retrospective Analysis From a Community-Based Hospital
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ijeoma Ikedum, MD, MSc (she/her/hers)
Wellstar Kennestone Regional Medical Center
Marietta, GA
Presenting Author(s)
Ijeoma Ikedum, MD, MSc1, Oluwaseun C. Sadare, MD2, Raja Shekhar R. Sappati Biyyani, MD3
1Wellstar Kennestone Regional Medical Center, Marietta, GA; 2Wellstar Kennestone Regional Medical Center, Powder Springs, GA; 3GI Specialists of Georgia, Marietta, GA
Introduction: Diverticular hemorrhage is one of the most common causes of acute lower gastrointestinal bleeding (LGIB) amongst older adults requiring hospitalization. While the precise pathophysiology of diverticular hemorrhage remains unclear, growing evidence suggests a strong role of systemic vascular compromise especially related to hypertension and arteriosclerosis-related in the pathophysiology of diverticular bleeding (1, 2). Early morning fluctuation has been recently identified to be a predisposing factor in patients with recurrent diverticular bleeding (3). Despite these observations, clinical data is lacking regarding the role of blood pressures in patients presenting with LGIB. This study aims to evaluate the association between hypertension severity and diverticular bleeding.
Methods: We conducted a retrospective cohort study of 206 patients who presented with LGIB at a community hospital between January 1 and December 31, 2024. After chart review, 151 patients aged 40–85 were confirmed to have diverticular bleeding. All included patients had recorded initial blood pressure, and data were analyzed using descriptive statistics, Fisher’s exact test, and logistic regression in R (v4.3.1) to evaluate the association between hypertension severity and diverticular bleeding.
Results: Blood pressure at ER presentation was classified per 2020 ACC/AHA guidelines: 9.9% had Stage 1 Hypertension, 39.7% Stage 2, 11.3% Hypertensive Urgency, 7.9% Elevated BP, and 17.9% were hypotensive due to acute blood loss ( Table 1).
Fisher’s Exact Test showed no significant unadjusted association between BP category and diverticular bleeding (p = 0.129). However, multivariable logistic regression adjusting for NSAID use, CKD, diabetes, and anticoagulant/antiplatelet therapy found hypertension significantly increased bleeding odds (OR 17.1, 95% CI: 6.2–56.9, p < 0.001) ( Table 2). NSAID use, CKD, and diabetes were also independent predictors, while anticoagulant/antiplatelet use was not statistically significant
Discussion: Although unadjusted analysis using Fisher’s Exact Test did not show statistical significance, multivariable logistic regression revealed that patients with severe hypertension had markedly higher odds of bleeding. CKD, diabetes, and NSAID use were also independently associated with bleeding risk. These findings suggest that hypertension severity, along with vascular and metabolic comorbidities, may play an important role in the pathophysiology of diverticular hemorrhage.
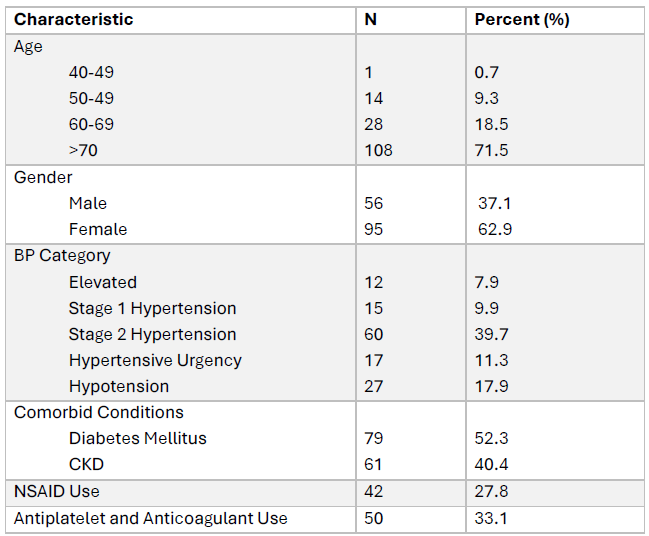
Figure: Table 1. Baseline Characteristics of Patients with Diverticular Bleeding (N = 151)
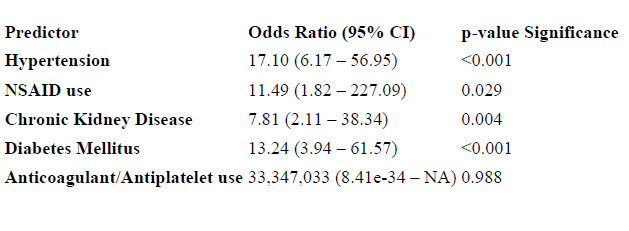
Figure: Table 2: Association Between Hypertension and Diverticular Bleeding Adjusted for Comorbidities and Medication Use
Disclosures:
Ijeoma Ikedum indicated no relevant financial relationships.
Oluwaseun Sadare indicated no relevant financial relationships.
Raja Shekhar Sappati Biyyani indicated no relevant financial relationships.
Ijeoma Ikedum, MD, MSc1, Oluwaseun C. Sadare, MD2, Raja Shekhar R. Sappati Biyyani, MD3. P5196 - Can Uncontrolled Hypertension Cause Diverticular Hemorrhage? A Retrospective Analysis From a Community-Based Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wellstar Kennestone Regional Medical Center, Marietta, GA; 2Wellstar Kennestone Regional Medical Center, Powder Springs, GA; 3GI Specialists of Georgia, Marietta, GA
Introduction: Diverticular hemorrhage is one of the most common causes of acute lower gastrointestinal bleeding (LGIB) amongst older adults requiring hospitalization. While the precise pathophysiology of diverticular hemorrhage remains unclear, growing evidence suggests a strong role of systemic vascular compromise especially related to hypertension and arteriosclerosis-related in the pathophysiology of diverticular bleeding (1, 2). Early morning fluctuation has been recently identified to be a predisposing factor in patients with recurrent diverticular bleeding (3). Despite these observations, clinical data is lacking regarding the role of blood pressures in patients presenting with LGIB. This study aims to evaluate the association between hypertension severity and diverticular bleeding.
Methods: We conducted a retrospective cohort study of 206 patients who presented with LGIB at a community hospital between January 1 and December 31, 2024. After chart review, 151 patients aged 40–85 were confirmed to have diverticular bleeding. All included patients had recorded initial blood pressure, and data were analyzed using descriptive statistics, Fisher’s exact test, and logistic regression in R (v4.3.1) to evaluate the association between hypertension severity and diverticular bleeding.
Results: Blood pressure at ER presentation was classified per 2020 ACC/AHA guidelines: 9.9% had Stage 1 Hypertension, 39.7% Stage 2, 11.3% Hypertensive Urgency, 7.9% Elevated BP, and 17.9% were hypotensive due to acute blood loss ( Table 1).
Fisher’s Exact Test showed no significant unadjusted association between BP category and diverticular bleeding (p = 0.129). However, multivariable logistic regression adjusting for NSAID use, CKD, diabetes, and anticoagulant/antiplatelet therapy found hypertension significantly increased bleeding odds (OR 17.1, 95% CI: 6.2–56.9, p < 0.001) ( Table 2). NSAID use, CKD, and diabetes were also independent predictors, while anticoagulant/antiplatelet use was not statistically significant
Discussion: Although unadjusted analysis using Fisher’s Exact Test did not show statistical significance, multivariable logistic regression revealed that patients with severe hypertension had markedly higher odds of bleeding. CKD, diabetes, and NSAID use were also independently associated with bleeding risk. These findings suggest that hypertension severity, along with vascular and metabolic comorbidities, may play an important role in the pathophysiology of diverticular hemorrhage.
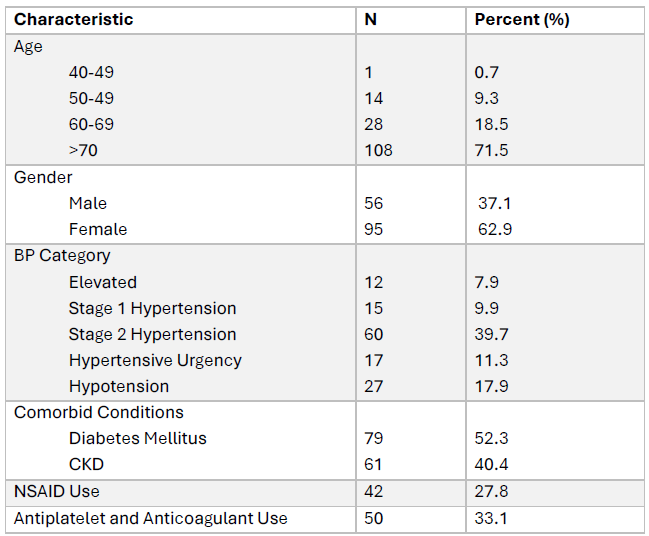
Figure: Table 1. Baseline Characteristics of Patients with Diverticular Bleeding (N = 151)
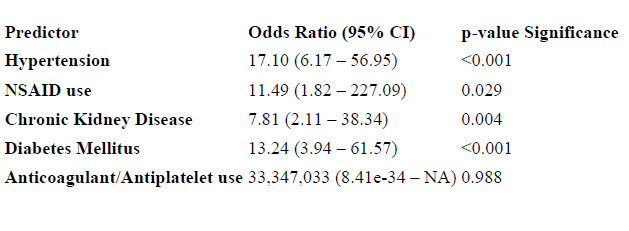
Figure: Table 2: Association Between Hypertension and Diverticular Bleeding Adjusted for Comorbidities and Medication Use
Disclosures:
Ijeoma Ikedum indicated no relevant financial relationships.
Oluwaseun Sadare indicated no relevant financial relationships.
Raja Shekhar Sappati Biyyani indicated no relevant financial relationships.
Ijeoma Ikedum, MD, MSc1, Oluwaseun C. Sadare, MD2, Raja Shekhar R. Sappati Biyyani, MD3. P5196 - Can Uncontrolled Hypertension Cause Diverticular Hemorrhage? A Retrospective Analysis From a Community-Based Hospital, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

