Tuesday Poster Session
Category: GI Bleeding
P5195 - One-Year Risk of Non-Variceal Gastrointestinal Bleeding Following PCI: A Real-World Comparative Analysis of Antiplatelet Regimens Using a National Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KA
Khaled Alsabbagh Alchirazi, MD
Aurora Health Care
Brookfield, WI
Presenting Author(s)
Khaled Alsabbagh Alchirazi, MD1, Rahul Karna, MD2, Muaz Alsabbagh, MD3, Kinan Obeidat, MD4, Fouad Jaber, MD5, Mohammad Bilal, MD, FACG6
1Aurora Health Care, Brookfield, WI; 2University of Minnesota Medical Center, Minneapolis, MN; 3Detroit Medical Center/Wayne State University, Cleveland, OH; 4University of Texas Medical Branch, Santa Fe, TX; 5Baylor College of Medicine, Houston, TX; 6University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a challenging problem to manage following percutaneous coronary intervention (PCI), particularly in patients receiving dual antiplatelet therapy (DAPT). Newer P2Y12 inhibitors, while offering improved cardiovascular outcomes, may elevate bleeding risk. This study aimed to determine the 1-year incidence of NVUGIB post-PCI and to compare bleeding risk across commonly used antiplatelet regimens using a large real-world cohort.
Methods: We queried the TriNetX database to identify adults (≥18 years) who had ST-elevation myocardial infarction (STEMI) or non-STEMI and underwent PCI between 2014 and 2023. Patients were stratified into three groups based on antiplatelet therapy post-PCI: (1) general DAPT users, (2) aspirin (ASA) + clopidogrel, and (3) ASA + ticagrelor or prasugrel. Exclusion criteria included prior GI bleeding, liver cirrhosis, or anticoagulation use. We performed 1:1 propensity-score matching (PSM) for demographics, comorbidities, alcohol use, tobacco use, thrombocytopenia, proton pump inhibitor use and NSAID use. The primary outcome was 1-year incidence of NVGIB. Secondary outcomes were 1-year overall mortality rate, prolonged mechanical ventilation, shock, upper endoscopy, Intensive care unit need, acute kidney injury, need for hemodialysis and need for blood transfusion. Hazard ratios (HR) with 95% confidence intervals (CI) were calculated to express the risk of each variable. P-value of < 0.05 was considered statistically significant.
Results: After PSM, 49,355 patients were included in the PCI cohort, with 3091 (6.3%) developing NVUGIB within 1 year. Among 37,953 patients on ASA + clopidogrel, 2543 (6.7%) experienced NVUGIB. In the ASA + ticagrelor/prasugrel group (n = 23,834), 1563 patients (6.6%) developed NVUGIB. In a matched comparison between patients who underwent PCI and developed NVUGIB versus those who did not, NVUGIB was associated with significantly higher rates of intensive care unit admission (HR 1.82), intubation (HR 1.76), acute kidney injury (HR 1.36), hypovolemic shock (HR 7.87), need for blood transfusion (HR 5.02), hemodialysis (HR 1.62), and mortality (HR 1.24).
Discussion: The 1-year risk of NVUGIB following PCI was significant and varied across antiplatelet regimens. Patients on ASA + clopidogrel had the highest bleeding risk. NVUGIB has a substantial impact on mortality, morbidity, and in-hospital health care resource utilization.
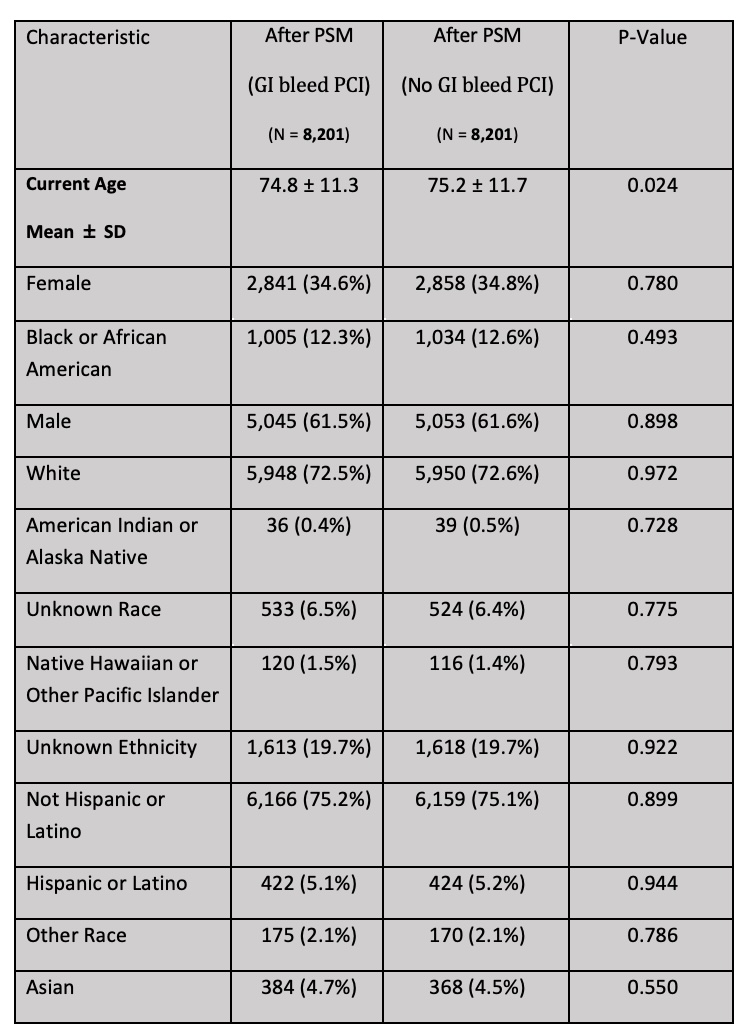
Figure: Table 1: Baseline demographic characteristics of patients undergoing PCI with and without GI bleeding after propensity score matching (PSM)
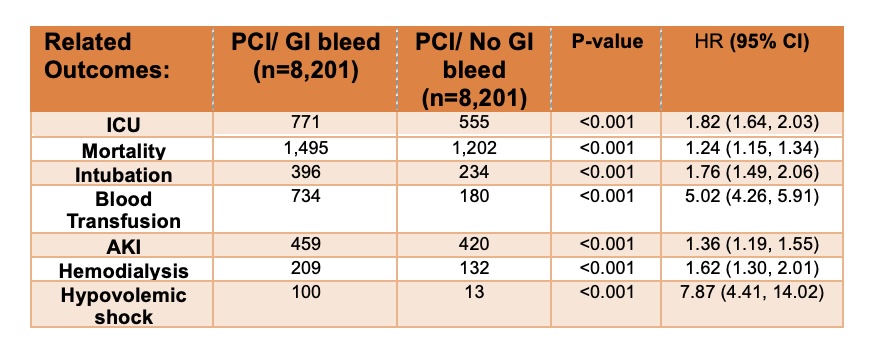
Figure: Table 2: Adverse Outcomes in PCI Patients With vs Without GI Bleeding
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Khaled Alsabbagh Alchirazi, MD1, Rahul Karna, MD2, Muaz Alsabbagh, MD3, Kinan Obeidat, MD4, Fouad Jaber, MD5, Mohammad Bilal, MD, FACG6. P5195 - One-Year Risk of Non-Variceal Gastrointestinal Bleeding Following PCI: A Real-World Comparative Analysis of Antiplatelet Regimens Using a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Aurora Health Care, Brookfield, WI; 2University of Minnesota Medical Center, Minneapolis, MN; 3Detroit Medical Center/Wayne State University, Cleveland, OH; 4University of Texas Medical Branch, Santa Fe, TX; 5Baylor College of Medicine, Houston, TX; 6University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Non-variceal upper gastrointestinal bleeding (NVUGIB) is a challenging problem to manage following percutaneous coronary intervention (PCI), particularly in patients receiving dual antiplatelet therapy (DAPT). Newer P2Y12 inhibitors, while offering improved cardiovascular outcomes, may elevate bleeding risk. This study aimed to determine the 1-year incidence of NVUGIB post-PCI and to compare bleeding risk across commonly used antiplatelet regimens using a large real-world cohort.
Methods: We queried the TriNetX database to identify adults (≥18 years) who had ST-elevation myocardial infarction (STEMI) or non-STEMI and underwent PCI between 2014 and 2023. Patients were stratified into three groups based on antiplatelet therapy post-PCI: (1) general DAPT users, (2) aspirin (ASA) + clopidogrel, and (3) ASA + ticagrelor or prasugrel. Exclusion criteria included prior GI bleeding, liver cirrhosis, or anticoagulation use. We performed 1:1 propensity-score matching (PSM) for demographics, comorbidities, alcohol use, tobacco use, thrombocytopenia, proton pump inhibitor use and NSAID use. The primary outcome was 1-year incidence of NVGIB. Secondary outcomes were 1-year overall mortality rate, prolonged mechanical ventilation, shock, upper endoscopy, Intensive care unit need, acute kidney injury, need for hemodialysis and need for blood transfusion. Hazard ratios (HR) with 95% confidence intervals (CI) were calculated to express the risk of each variable. P-value of < 0.05 was considered statistically significant.
Results: After PSM, 49,355 patients were included in the PCI cohort, with 3091 (6.3%) developing NVUGIB within 1 year. Among 37,953 patients on ASA + clopidogrel, 2543 (6.7%) experienced NVUGIB. In the ASA + ticagrelor/prasugrel group (n = 23,834), 1563 patients (6.6%) developed NVUGIB. In a matched comparison between patients who underwent PCI and developed NVUGIB versus those who did not, NVUGIB was associated with significantly higher rates of intensive care unit admission (HR 1.82), intubation (HR 1.76), acute kidney injury (HR 1.36), hypovolemic shock (HR 7.87), need for blood transfusion (HR 5.02), hemodialysis (HR 1.62), and mortality (HR 1.24).
Discussion: The 1-year risk of NVUGIB following PCI was significant and varied across antiplatelet regimens. Patients on ASA + clopidogrel had the highest bleeding risk. NVUGIB has a substantial impact on mortality, morbidity, and in-hospital health care resource utilization.
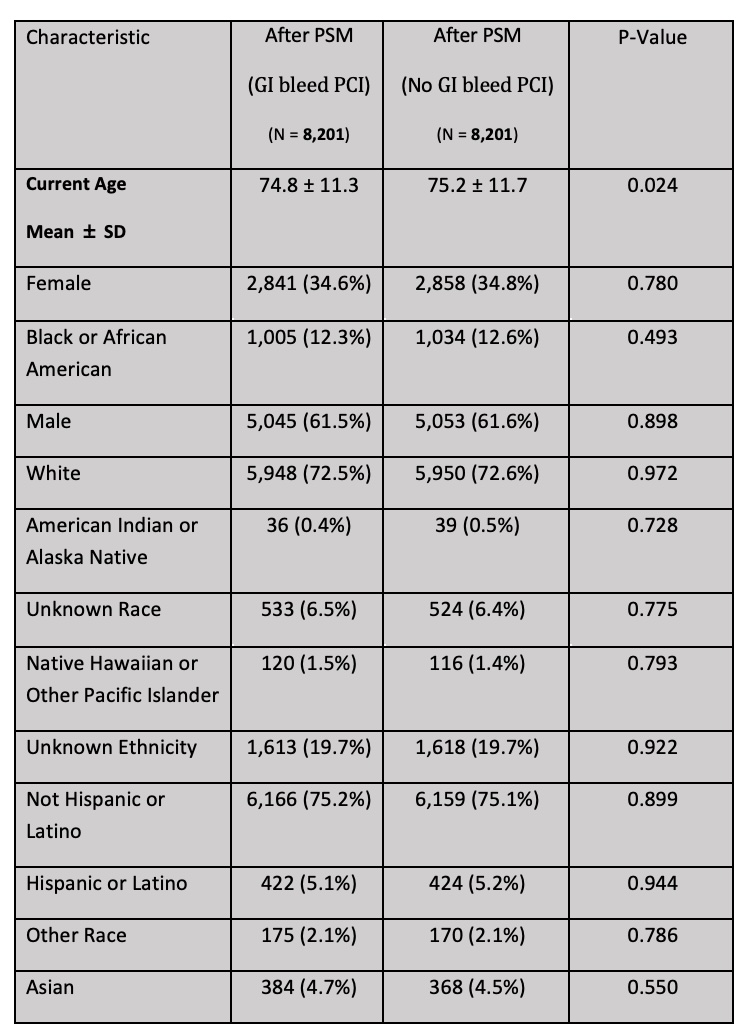
Figure: Table 1: Baseline demographic characteristics of patients undergoing PCI with and without GI bleeding after propensity score matching (PSM)
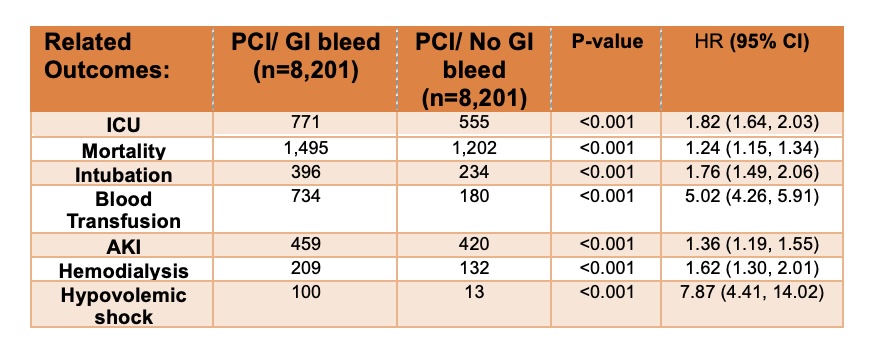
Figure: Table 2: Adverse Outcomes in PCI Patients With vs Without GI Bleeding
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Muaz Alsabbagh indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Khaled Alsabbagh Alchirazi, MD1, Rahul Karna, MD2, Muaz Alsabbagh, MD3, Kinan Obeidat, MD4, Fouad Jaber, MD5, Mohammad Bilal, MD, FACG6. P5195 - One-Year Risk of Non-Variceal Gastrointestinal Bleeding Following PCI: A Real-World Comparative Analysis of Antiplatelet Regimens Using a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
