Tuesday Poster Session
Category: GI Bleeding
P5194 - Retrospective Study on the Utility of Hemoglobin Drop as a Predictor of Endoscopic Findings and Therapeutic Interventions in Inpatients Who Develop Upper Gastrointestinal Bleeding Post-Admission
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Obada Daaboul, MD
Southern Illinois University
Springfield, IL
Presenting Author(s)
Obada Daaboul, MD1, Mulham Alom, MD2, Muhammed Yaman Swied, MBBS1, Randall S.. Robbs, MBA1, Michael Buhnerkempe, PhD1, Harris Siddiqui, MD1, Abdul Swied, MD1
1Southern Illinois University, Springfield, IL; 2Internal Medicine, Southern Illinois University School of Medicine, Springfield, IL
Introduction: Upper gastrointestinal bleeding (UGIB) is a common reason for inpatient gastroenterology (GI) consultation. Many hospitalized patients develop signs or symptoms suggestive of UGIB, such as acute anemia, even when admitted for other conditions. While a drop in hemoglobin (Hgb) is a frequent finding, its ability to predict positive esophagogastroduodenoscopy (EGD) results or the need for interventions remains underexplored. This study examines the predictive value of Hgb decline in patients who were admitted with relatively normal levels.
Methods: This retrospective study analyzed 987 patients who underwent EGD for suspected UGIB between 2019 and 2024, excluding those with UGIB at admission. A total of 247 inpatients who developed UGIB or GI-related anemia during hospitalization were included. The study evaluated the predictive value of ΔHGB, defined as the change in hemoglobin from admission to the day of acute drop, for identifying positive EGD findings. Patients were grouped by ΔHGB ≥ 2 versus < 2, and treatment needs were compared. Descriptive statistics summarized key data, and chi-square tests were used to calculate odds ratios, 95% confidence intervals (CI), and p-values, with significance set at p < 0.05.
Results: The average ΔHGB was 3.02 ± 2.07 g/dL, with 65.9% showing a ΔHGB ≥ 2 g/dL. Patients with a ΔHGB ≥ 2 g/dL had higher odds of positive EGD findings and a greater need for medical, endoscopic, and interventional radiology (IR) interventions compared to those with a ΔHGB < 2. However, only the association with IR intervention reached statistical significance.
Discussion: Our analysis revealed that a ΔHGB ≥ 2 g/dL was associated with higher odds of positive EGD findings and an increased need for medical, endoscopic, and IR interventions compared to a ΔHGB < 2 g/dL. However, most associations were not statistically significant, likely due to limited sample size. The only statistically significant finding was the association between ΔHGB ≥ 2 and the need for IR intervention, though this result had a wide confidence interval. In conclusion, this analysis highlights the possibility of using ΔHGB ≥ 2 to predict positive EGD findings and the need for medical, endoscopic, or IR interventions. Further research with a larger sample size is necessary to investigate this concept more comprehensively.
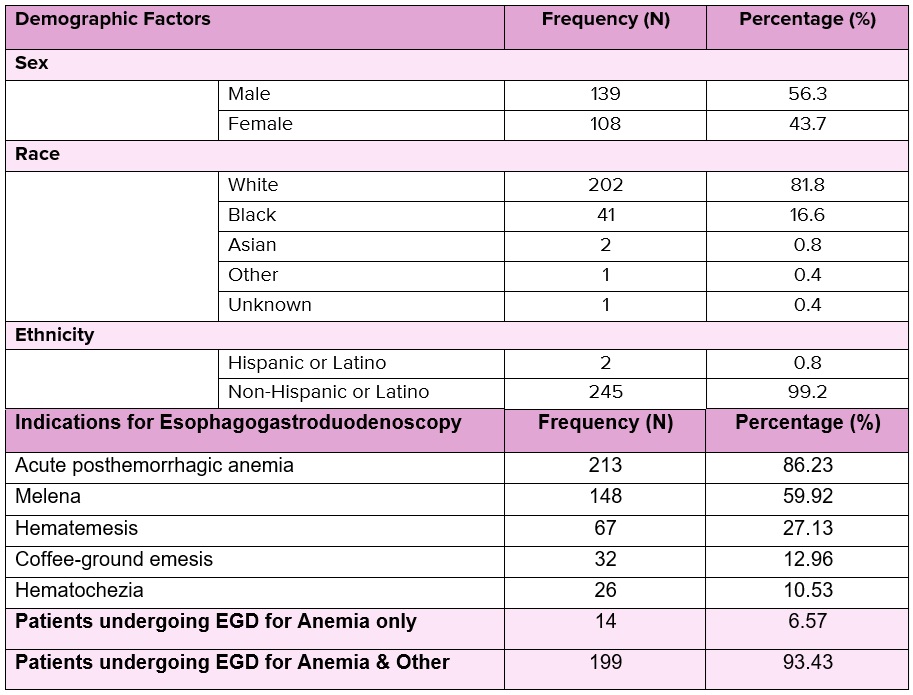
Figure: Demographic characteristics and clinical indications for esophagogastroduodenoscopy (EGD)
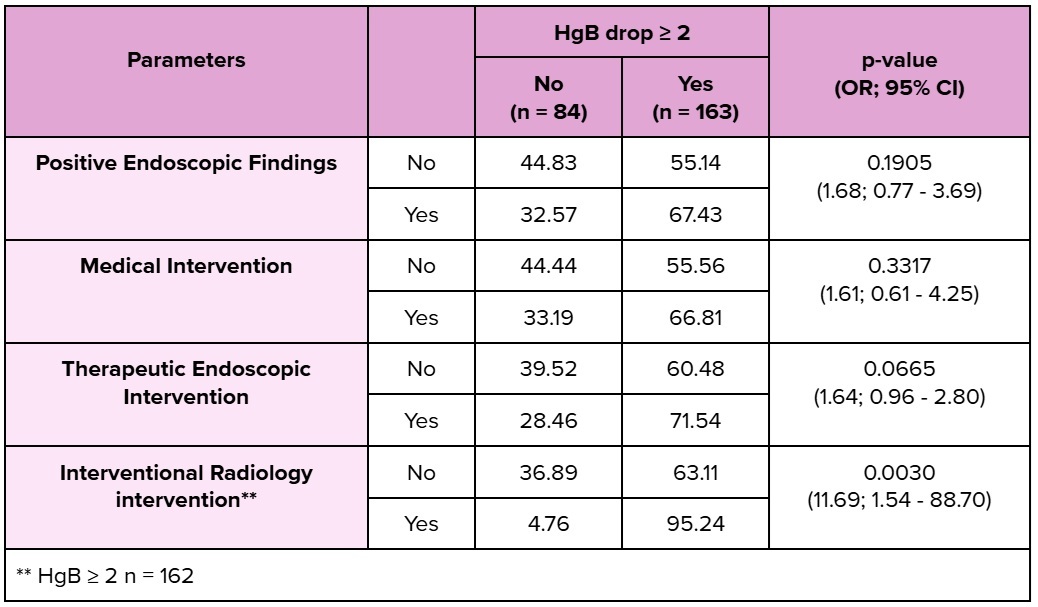
Figure: Distribution of clinical parameters and interventions in patients stratified by hemoglobin drop ≥ 2 g/dL
Disclosures:
Obada Daaboul indicated no relevant financial relationships.
Mulham Alom indicated no relevant financial relationships.
Muhammed Yaman Swied indicated no relevant financial relationships.
Randall Robbs indicated no relevant financial relationships.
Michael Buhnerkempe indicated no relevant financial relationships.
Harris Siddiqui indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Obada Daaboul, MD1, Mulham Alom, MD2, Muhammed Yaman Swied, MBBS1, Randall S.. Robbs, MBA1, Michael Buhnerkempe, PhD1, Harris Siddiqui, MD1, Abdul Swied, MD1. P5194 - Retrospective Study on the Utility of Hemoglobin Drop as a Predictor of Endoscopic Findings and Therapeutic Interventions in Inpatients Who Develop Upper Gastrointestinal Bleeding Post-Admission, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Southern Illinois University, Springfield, IL; 2Internal Medicine, Southern Illinois University School of Medicine, Springfield, IL
Introduction: Upper gastrointestinal bleeding (UGIB) is a common reason for inpatient gastroenterology (GI) consultation. Many hospitalized patients develop signs or symptoms suggestive of UGIB, such as acute anemia, even when admitted for other conditions. While a drop in hemoglobin (Hgb) is a frequent finding, its ability to predict positive esophagogastroduodenoscopy (EGD) results or the need for interventions remains underexplored. This study examines the predictive value of Hgb decline in patients who were admitted with relatively normal levels.
Methods: This retrospective study analyzed 987 patients who underwent EGD for suspected UGIB between 2019 and 2024, excluding those with UGIB at admission. A total of 247 inpatients who developed UGIB or GI-related anemia during hospitalization were included. The study evaluated the predictive value of ΔHGB, defined as the change in hemoglobin from admission to the day of acute drop, for identifying positive EGD findings. Patients were grouped by ΔHGB ≥ 2 versus < 2, and treatment needs were compared. Descriptive statistics summarized key data, and chi-square tests were used to calculate odds ratios, 95% confidence intervals (CI), and p-values, with significance set at p < 0.05.
Results: The average ΔHGB was 3.02 ± 2.07 g/dL, with 65.9% showing a ΔHGB ≥ 2 g/dL. Patients with a ΔHGB ≥ 2 g/dL had higher odds of positive EGD findings and a greater need for medical, endoscopic, and interventional radiology (IR) interventions compared to those with a ΔHGB < 2. However, only the association with IR intervention reached statistical significance.
Discussion: Our analysis revealed that a ΔHGB ≥ 2 g/dL was associated with higher odds of positive EGD findings and an increased need for medical, endoscopic, and IR interventions compared to a ΔHGB < 2 g/dL. However, most associations were not statistically significant, likely due to limited sample size. The only statistically significant finding was the association between ΔHGB ≥ 2 and the need for IR intervention, though this result had a wide confidence interval. In conclusion, this analysis highlights the possibility of using ΔHGB ≥ 2 to predict positive EGD findings and the need for medical, endoscopic, or IR interventions. Further research with a larger sample size is necessary to investigate this concept more comprehensively.
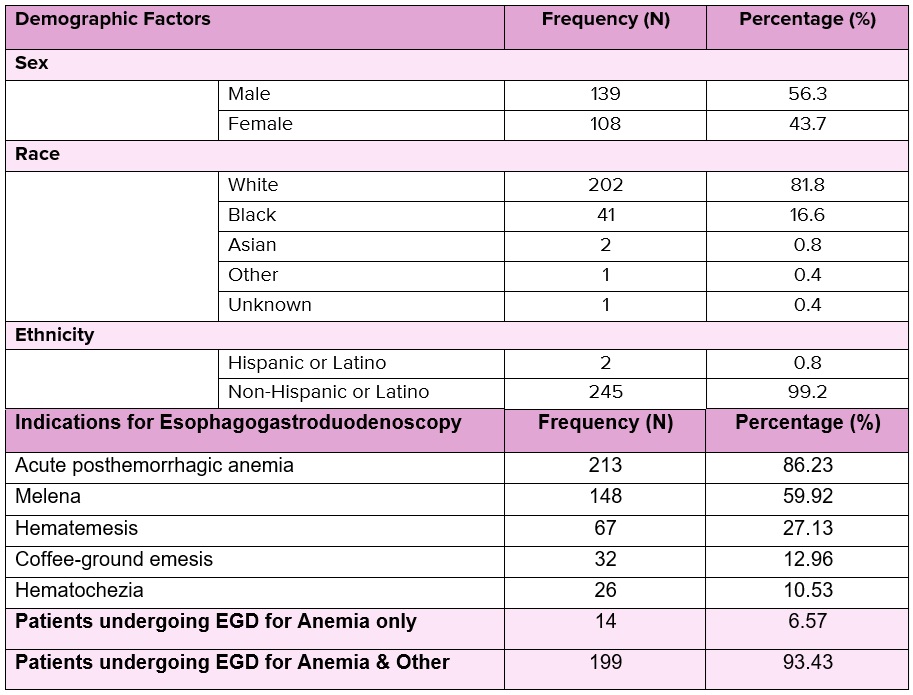
Figure: Demographic characteristics and clinical indications for esophagogastroduodenoscopy (EGD)
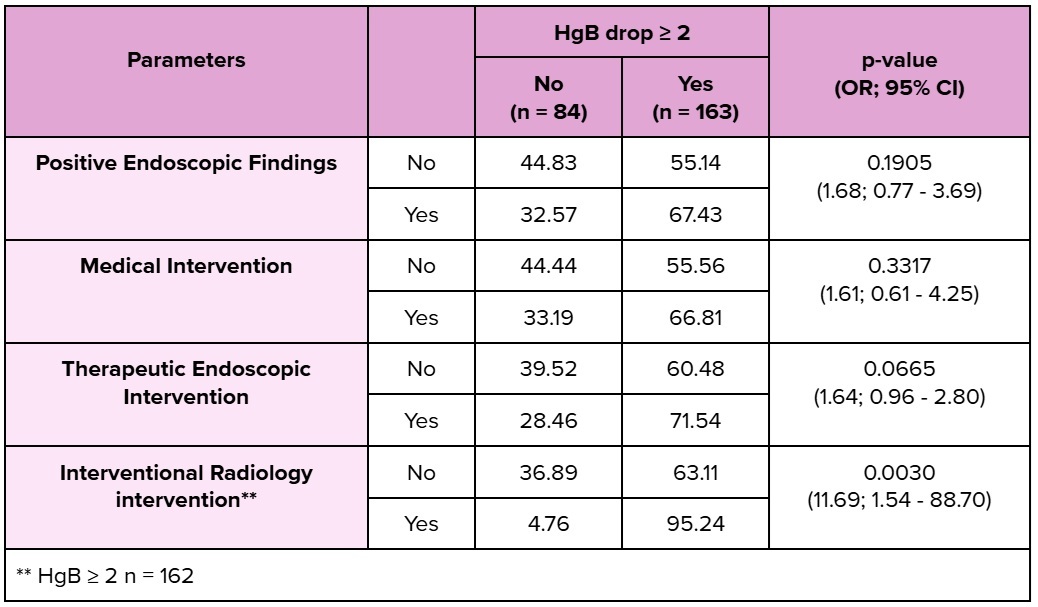
Figure: Distribution of clinical parameters and interventions in patients stratified by hemoglobin drop ≥ 2 g/dL
Disclosures:
Obada Daaboul indicated no relevant financial relationships.
Mulham Alom indicated no relevant financial relationships.
Muhammed Yaman Swied indicated no relevant financial relationships.
Randall Robbs indicated no relevant financial relationships.
Michael Buhnerkempe indicated no relevant financial relationships.
Harris Siddiqui indicated no relevant financial relationships.
Abdul Swied indicated no relevant financial relationships.
Obada Daaboul, MD1, Mulham Alom, MD2, Muhammed Yaman Swied, MBBS1, Randall S.. Robbs, MBA1, Michael Buhnerkempe, PhD1, Harris Siddiqui, MD1, Abdul Swied, MD1. P5194 - Retrospective Study on the Utility of Hemoglobin Drop as a Predictor of Endoscopic Findings and Therapeutic Interventions in Inpatients Who Develop Upper Gastrointestinal Bleeding Post-Admission, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
