Tuesday Poster Session
Category: GI Bleeding
P5189 - Evaluating the Role of Antimicrobial Prophylaxis in Child-Pugh A/B Cirrhosis With Upper GI Bleeding: Insights From a Multicenter Retrospective Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Majd Haj-Rubaeih, MBBS (she/her/hers)
Rochester Regional Health, Unity Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Mostafa Najim, MBBS2, Farooq Chaudhary, MBBS3, Hamza Akhtar, MD4, Ryan Tam, 5, Waddah Abd El-Radi, MD3, Keerthi Mannumbeth. Renjith, MD3, Marina Takawy, MD3, Majd Haj-Rubaeih, MBBS3, Yousef Waly, MB, BCh, BAO3, Adeena Maryyum, 6, Asim Mushtaq, MD7, Erik Olson, DO4
1Unity Hospital, Rochester, NY; 2Unity Hospital - Rochester Regional Health, Rochester, NY; 3Rochester Regional Health, Unity Hospital, Rochester, NY; 4Rochester General Hospital, Rochester, NY; 5Lake Erie College of Osteopathic Medicine, Rochester, NY; 6Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 7Rochester Regional Health, Rochester, NY
Introduction: Upper gastrointestinal bleeding (UGIB) in cirrhosis patients presents a considerable risk of infectious complications and mortality. Antimicrobial prophylaxis is advocated to prevent infections; however, its efficacy in Child-Pugh (CP) class A and B patients remains uncertain. This study evaluated the impact of antimicrobial prophylaxis on outcomes of UGIB among cirrhotic CP class A/B patients with UGIB.
Methods: Patients with CP class A/B cirrhosis hospitalized for UGIB at two Rochester Regional Health hospitals from January 2020 - March 2024 were enrolled retrospectively. Patients with CP class C cirrhosis and those with bacterial infections were excluded. Patients were stratified into two groups based on antimicrobial prophylaxis receipt. Outcomes evaluated included infection incidence within 30 days, rebleeding during hospitalization, in-hospital mortality, 30-day mortality, and 30-day readmission rates.
Results: We included 150 cirrhotic patients (CP class A or B) admitted for UGIB, of whom 101 received antimicrobial prophylaxis, while 49 did not. Of patients who received antimicrobial prophylaxis, a higher proportion had variceal bleeding as the etiology for bleeding compared to those who did not receive antimicrobial prophylaxis (64.4% vs. 44.9%, P=0.02) (Table 1). A moderate to large amount of ascites was more prevalent in the prophylaxis group compared to those without prophylaxis (27.72% vs. 10.20%, P=0.02), with no other notable differences in baseline characteristics. Outcome analysis indicated lower infection rates in the prophylaxis group (11.9%) compared to the non-prophylaxis group (18.4%), although this difference was not statistically significant (OR 0.58, 95% CI 0.22–1.55, P=0.28) (Table 2). There were no significant differences between the groups in terms of rebleeding rates, in-hospital mortality, 30-day mortality, and 30-day readmission.
Discussion: Antimicrobial prophylaxis in CP class A and B cirrhotic patients admitted with UGIB was associated with a nonsignificant reduction in overall infection rates without impacting rebleeding, mortality or readmission. These findings suggest that antibiotic treatment administered as needed may be adequate for patients with CP class A/B cirrhosis experiencing UGIB. However, prospective studies with larger sample sizes are warranted to validate our findings and inform clinical practice guidelines.
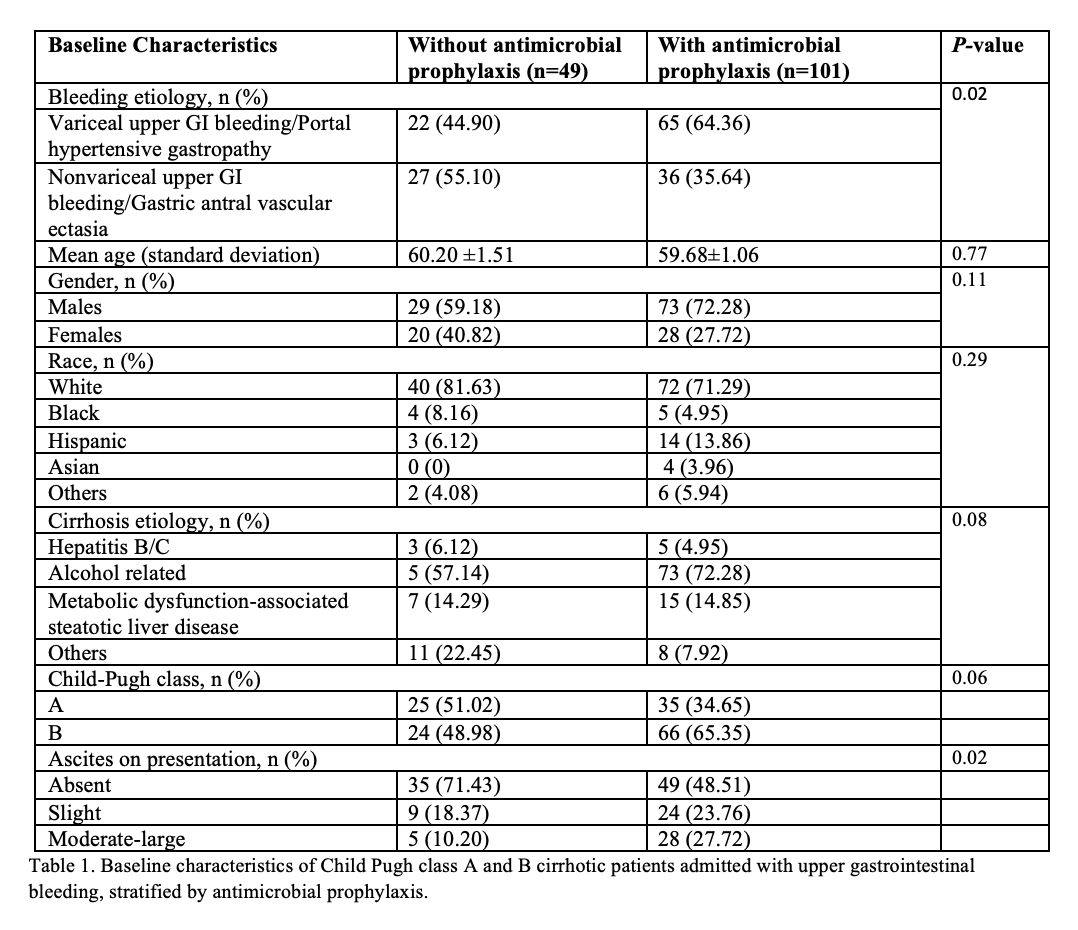
Figure: Table 1. Baseline characteristics of Child Pugh class A and B cirrhotic patients admitted with upper gastrointestinal bleeding, stratified by antimicrobial prophylaxis.
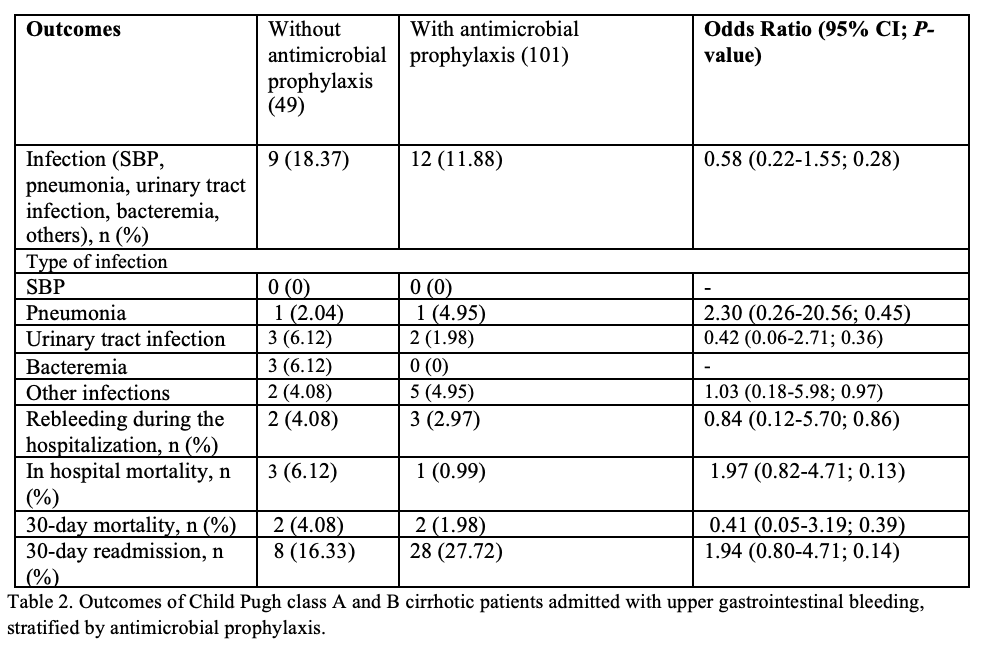
Figure: Table 2. Outcomes of Child Pugh class A and B cirrhotic patients admitted with upper gastrointestinal bleeding, stratified by antimicrobial prophylaxis.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Mostafa Najim indicated no relevant financial relationships.
Farooq Chaudhary indicated no relevant financial relationships.
Hamza Akhtar indicated no relevant financial relationships.
Ryan Tam indicated no relevant financial relationships.
Waddah Abd El-Radi indicated no relevant financial relationships.
Keerthi Renjith indicated no relevant financial relationships.
Marina Takawy indicated no relevant financial relationships.
Majd Haj-Rubaeih indicated no relevant financial relationships.
Yousef Waly indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Asim Mushtaq indicated no relevant financial relationships.
Erik Olson indicated no relevant financial relationships.
Ali Jaan, MD1, Mostafa Najim, MBBS2, Farooq Chaudhary, MBBS3, Hamza Akhtar, MD4, Ryan Tam, 5, Waddah Abd El-Radi, MD3, Keerthi Mannumbeth. Renjith, MD3, Marina Takawy, MD3, Majd Haj-Rubaeih, MBBS3, Yousef Waly, MB, BCh, BAO3, Adeena Maryyum, 6, Asim Mushtaq, MD7, Erik Olson, DO4. P5189 - Evaluating the Role of Antimicrobial Prophylaxis in Child-Pugh A/B Cirrhosis With Upper GI Bleeding: Insights From a Multicenter Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Unity Hospital, Rochester, NY; 2Unity Hospital - Rochester Regional Health, Rochester, NY; 3Rochester Regional Health, Unity Hospital, Rochester, NY; 4Rochester General Hospital, Rochester, NY; 5Lake Erie College of Osteopathic Medicine, Rochester, NY; 6Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 7Rochester Regional Health, Rochester, NY
Introduction: Upper gastrointestinal bleeding (UGIB) in cirrhosis patients presents a considerable risk of infectious complications and mortality. Antimicrobial prophylaxis is advocated to prevent infections; however, its efficacy in Child-Pugh (CP) class A and B patients remains uncertain. This study evaluated the impact of antimicrobial prophylaxis on outcomes of UGIB among cirrhotic CP class A/B patients with UGIB.
Methods: Patients with CP class A/B cirrhosis hospitalized for UGIB at two Rochester Regional Health hospitals from January 2020 - March 2024 were enrolled retrospectively. Patients with CP class C cirrhosis and those with bacterial infections were excluded. Patients were stratified into two groups based on antimicrobial prophylaxis receipt. Outcomes evaluated included infection incidence within 30 days, rebleeding during hospitalization, in-hospital mortality, 30-day mortality, and 30-day readmission rates.
Results: We included 150 cirrhotic patients (CP class A or B) admitted for UGIB, of whom 101 received antimicrobial prophylaxis, while 49 did not. Of patients who received antimicrobial prophylaxis, a higher proportion had variceal bleeding as the etiology for bleeding compared to those who did not receive antimicrobial prophylaxis (64.4% vs. 44.9%, P=0.02) (Table 1). A moderate to large amount of ascites was more prevalent in the prophylaxis group compared to those without prophylaxis (27.72% vs. 10.20%, P=0.02), with no other notable differences in baseline characteristics. Outcome analysis indicated lower infection rates in the prophylaxis group (11.9%) compared to the non-prophylaxis group (18.4%), although this difference was not statistically significant (OR 0.58, 95% CI 0.22–1.55, P=0.28) (Table 2). There were no significant differences between the groups in terms of rebleeding rates, in-hospital mortality, 30-day mortality, and 30-day readmission.
Discussion: Antimicrobial prophylaxis in CP class A and B cirrhotic patients admitted with UGIB was associated with a nonsignificant reduction in overall infection rates without impacting rebleeding, mortality or readmission. These findings suggest that antibiotic treatment administered as needed may be adequate for patients with CP class A/B cirrhosis experiencing UGIB. However, prospective studies with larger sample sizes are warranted to validate our findings and inform clinical practice guidelines.
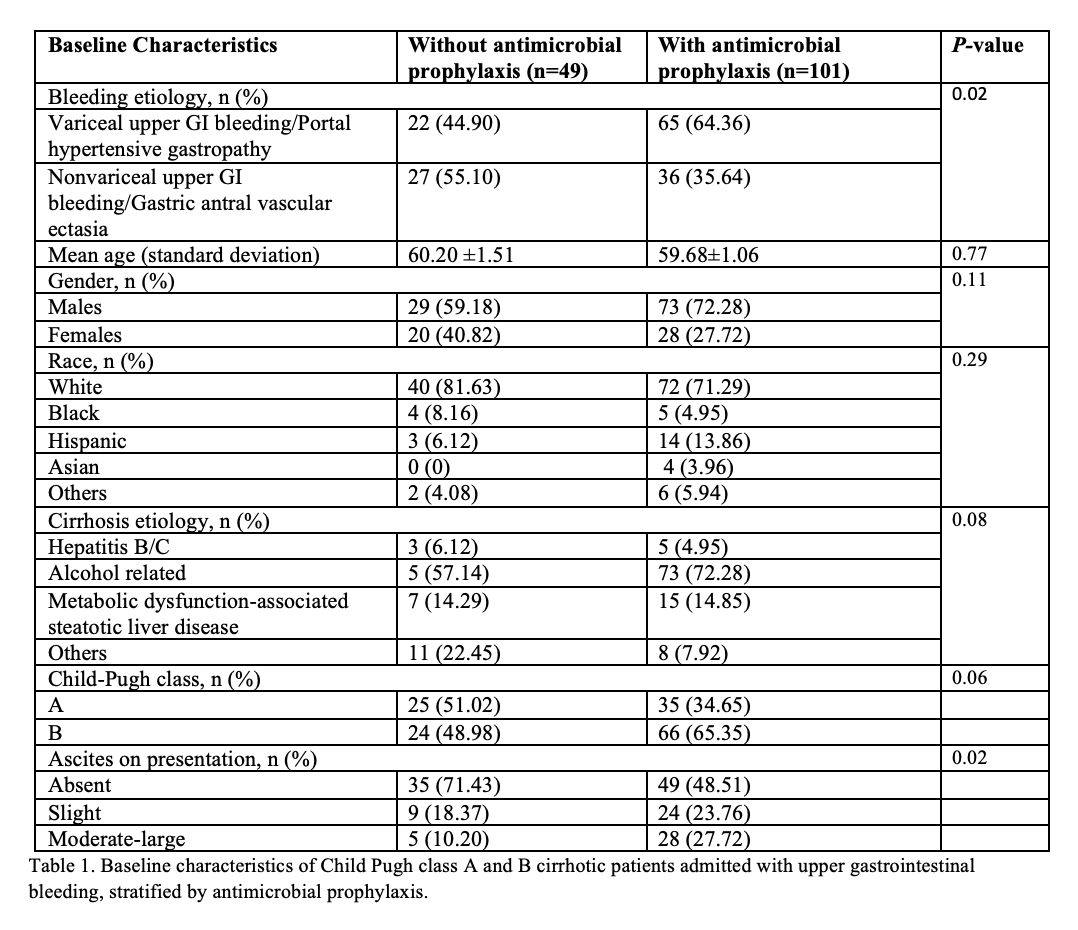
Figure: Table 1. Baseline characteristics of Child Pugh class A and B cirrhotic patients admitted with upper gastrointestinal bleeding, stratified by antimicrobial prophylaxis.
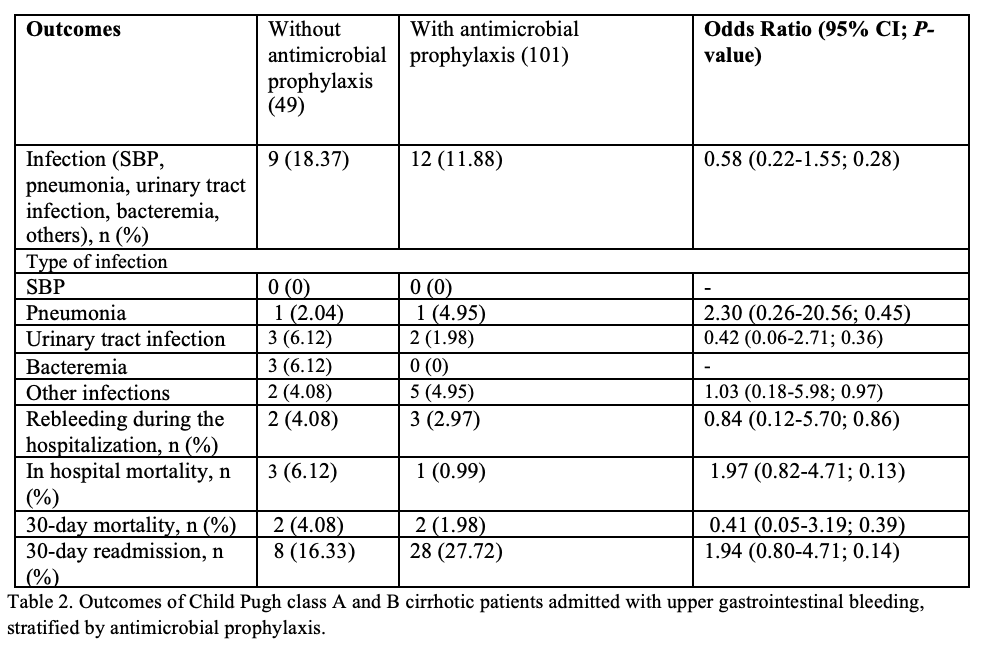
Figure: Table 2. Outcomes of Child Pugh class A and B cirrhotic patients admitted with upper gastrointestinal bleeding, stratified by antimicrobial prophylaxis.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Mostafa Najim indicated no relevant financial relationships.
Farooq Chaudhary indicated no relevant financial relationships.
Hamza Akhtar indicated no relevant financial relationships.
Ryan Tam indicated no relevant financial relationships.
Waddah Abd El-Radi indicated no relevant financial relationships.
Keerthi Renjith indicated no relevant financial relationships.
Marina Takawy indicated no relevant financial relationships.
Majd Haj-Rubaeih indicated no relevant financial relationships.
Yousef Waly indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Asim Mushtaq indicated no relevant financial relationships.
Erik Olson indicated no relevant financial relationships.
Ali Jaan, MD1, Mostafa Najim, MBBS2, Farooq Chaudhary, MBBS3, Hamza Akhtar, MD4, Ryan Tam, 5, Waddah Abd El-Radi, MD3, Keerthi Mannumbeth. Renjith, MD3, Marina Takawy, MD3, Majd Haj-Rubaeih, MBBS3, Yousef Waly, MB, BCh, BAO3, Adeena Maryyum, 6, Asim Mushtaq, MD7, Erik Olson, DO4. P5189 - Evaluating the Role of Antimicrobial Prophylaxis in Child-Pugh A/B Cirrhosis With Upper GI Bleeding: Insights From a Multicenter Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
