Tuesday Poster Session
Category: GI Bleeding
P5185 - Impact of Heart Failure Type on Outcomes in Patients Hospitalized for Gastrointestinal Bleeding: A National Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Maria Grba, DO (she/her/hers)
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Maria Grba, DO1, Denise Nunez, DO1, Patricia Zarza Gulino, MD1, Bhanu Siva Mohan Pinnam, MD1, Saksham Kohli, MBBS1, Gedion Yilma Amdetsion, MD2, Abhin Sapkota, MBBS1, Alejandro Nieto Dominguez, 2, Daniel Guifarro Rivera, MD3, Seema R. Gandhi, MD2
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Cook County Health, Chicago, IL; 3Cook County Health and Hospital Systems, Chicago, IL
Introduction: Gastrointestinal bleed (GIB), specifically nonvariceal upper gastrointestinal (NVUGIB) and lower gastrointestinal bleed (LGIB), are common causes of hospitalizations and are associated with adverse outcomes. Studies have shown that patients with heart failure who are admitted for NVUGIB and LGIB are at increased risk of mortality. However, there is limited information on differences in outcomes between types of heart failure. Our study aims to compare outcomes and adverse events of patients with heart failure with preserved ejection fraction (HFpEF) versus reduced ejection fraction (HFrEF) admitted for GIB.
Methods: Using the National Inpatient Sample (2016-2021), we identified adult patients admitted for NVUGIB and/or LGIB using the International Classification of Disease, Tenth Revision (ICD-10) codes. Patients were stratified by the presence of either concomitant HFpEF or HFrEF. Multivariate regression using STATA 18 was utilized to analyze the difference in outcomes, adverse events, and resource utilization, adjusting for demographics, comorbidities, and hospital characteristics.
Results: A total of 302,639 patients admitted for NVUGIB or LGIB with concomitant heart failure were identified, of which 183,575 (60.66%) had HFpEF and 119,065 (39.34%) had HFrEF. HFpEF patients were generally older and more often female than HFrEF patients, while a larger proportion of HFrEF patients had higher Charlson Comorbidity Index (CCI) scores, indicating greater comorbidity burden. HFrEF patients had significantly higher odds of in-hospital mortality (adjusted odds ratio [aOR] 1.40, p< 0.001), ICU stay (aOR 1.26, p< 0.001), AKI (aOR 1.08, p< 0.001), shock (aOR 1.40, p< 0.001), cardiac arrest (aOR 1.49, p< 0.001), and need for blood transfusion (aOR 1.04, p=0.048). There was no significant difference between groups in the likelihood of sepsis or VTE events. There was no statistically significant difference in LOS between groups; however, the HFrEF cohort had significantly higher mean hospitalization charges (+$2,017, p=0.004).
Discussion: We found that patients with HFrEF admitted for NVUGIB or LGIB have significantly worse outcomes and greater healthcare utilization than patients with HFpEF. Further studies to understand the pathophysiologic basis of these differences could provide insight into tailored therapy.
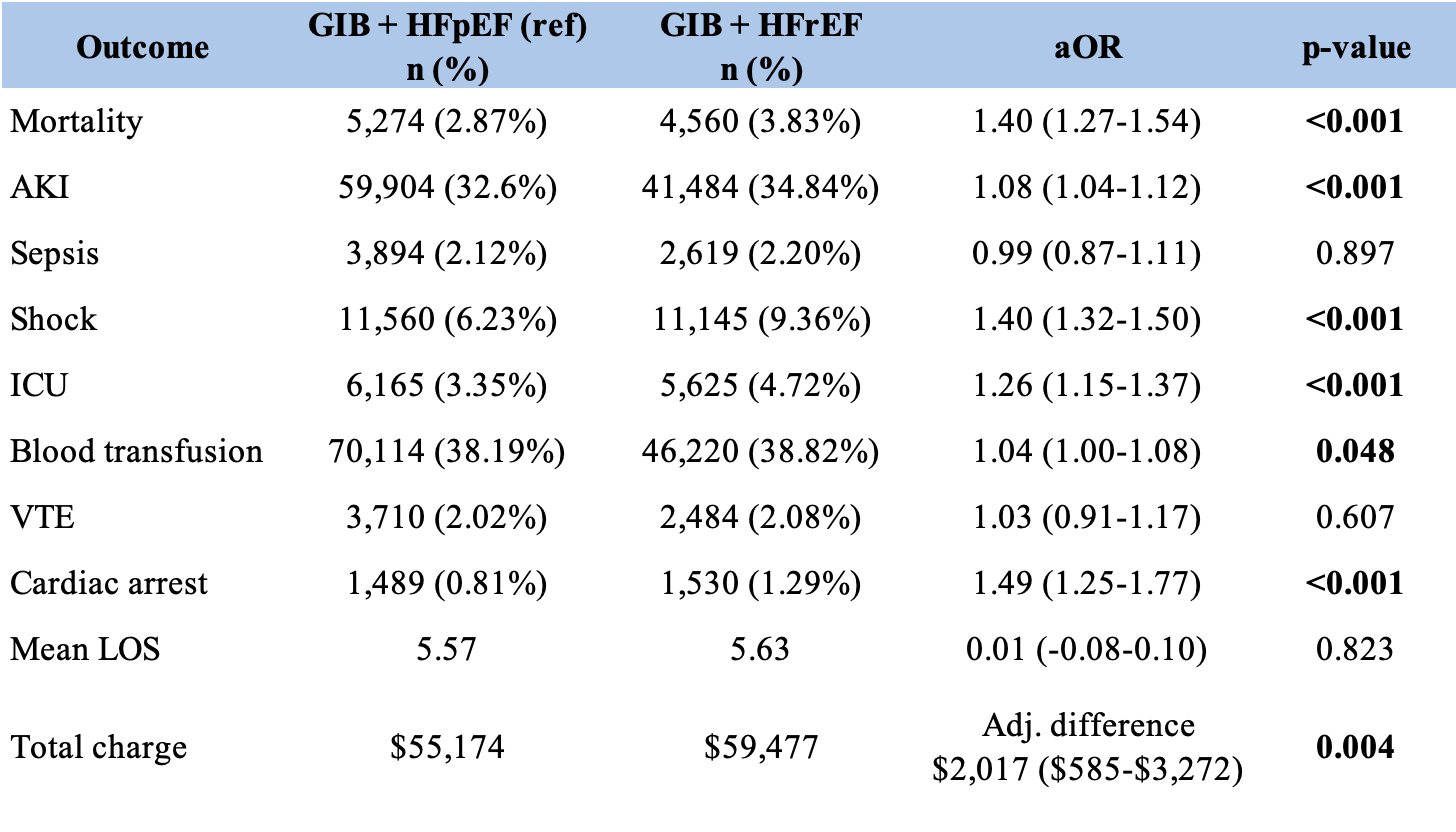
Figure: Baseline hospitalization characteristics for patients with gastrointestinal bleed stratified by heart failure type
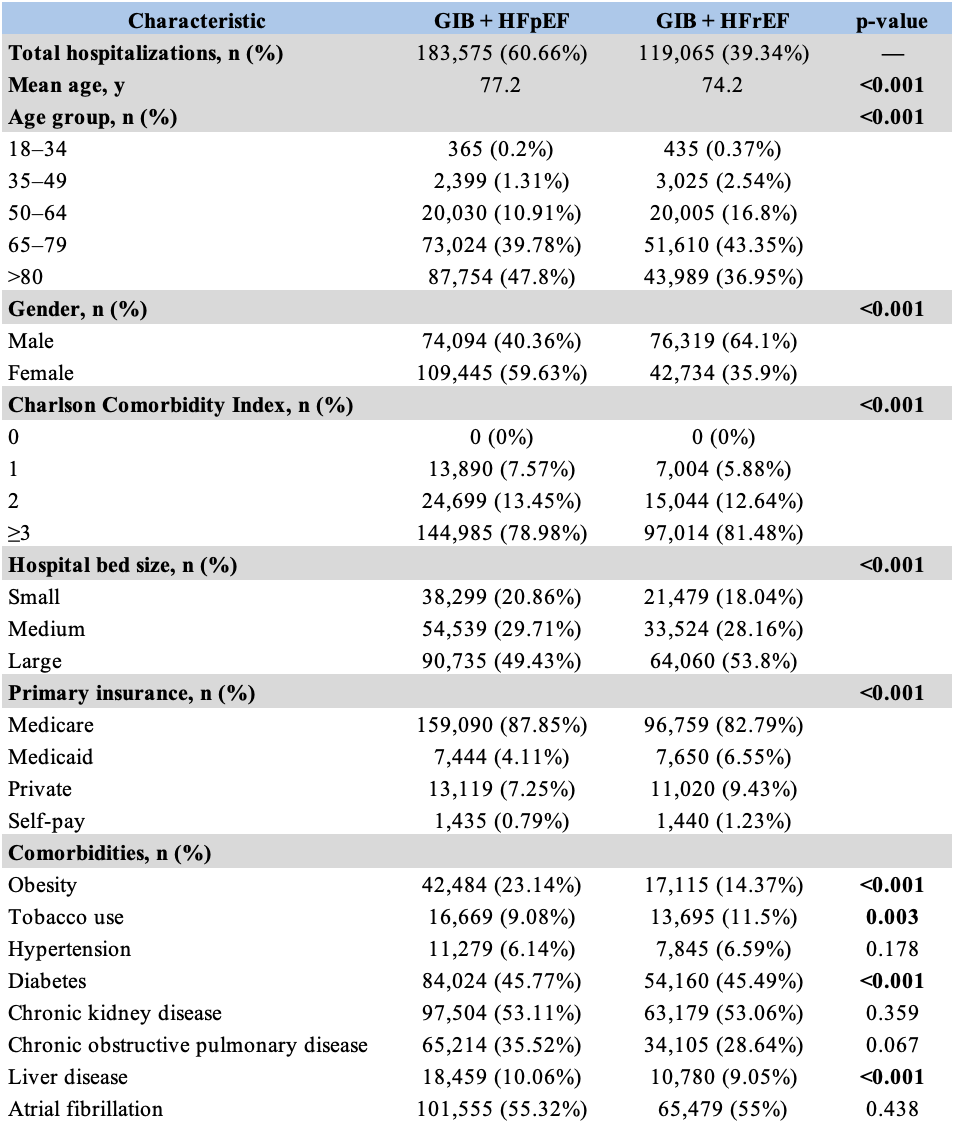
Figure: Outcomes, adverse events, and healthcare utilization
Disclosures:
Maria Grba indicated no relevant financial relationships.
Denise Nunez indicated no relevant financial relationships.
Patricia Zarza Gulino indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Maria Grba, DO1, Denise Nunez, DO1, Patricia Zarza Gulino, MD1, Bhanu Siva Mohan Pinnam, MD1, Saksham Kohli, MBBS1, Gedion Yilma Amdetsion, MD2, Abhin Sapkota, MBBS1, Alejandro Nieto Dominguez, 2, Daniel Guifarro Rivera, MD3, Seema R. Gandhi, MD2. P5185 - Impact of Heart Failure Type on Outcomes in Patients Hospitalized for Gastrointestinal Bleeding: A National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Cook County Health, Chicago, IL; 3Cook County Health and Hospital Systems, Chicago, IL
Introduction: Gastrointestinal bleed (GIB), specifically nonvariceal upper gastrointestinal (NVUGIB) and lower gastrointestinal bleed (LGIB), are common causes of hospitalizations and are associated with adverse outcomes. Studies have shown that patients with heart failure who are admitted for NVUGIB and LGIB are at increased risk of mortality. However, there is limited information on differences in outcomes between types of heart failure. Our study aims to compare outcomes and adverse events of patients with heart failure with preserved ejection fraction (HFpEF) versus reduced ejection fraction (HFrEF) admitted for GIB.
Methods: Using the National Inpatient Sample (2016-2021), we identified adult patients admitted for NVUGIB and/or LGIB using the International Classification of Disease, Tenth Revision (ICD-10) codes. Patients were stratified by the presence of either concomitant HFpEF or HFrEF. Multivariate regression using STATA 18 was utilized to analyze the difference in outcomes, adverse events, and resource utilization, adjusting for demographics, comorbidities, and hospital characteristics.
Results: A total of 302,639 patients admitted for NVUGIB or LGIB with concomitant heart failure were identified, of which 183,575 (60.66%) had HFpEF and 119,065 (39.34%) had HFrEF. HFpEF patients were generally older and more often female than HFrEF patients, while a larger proportion of HFrEF patients had higher Charlson Comorbidity Index (CCI) scores, indicating greater comorbidity burden. HFrEF patients had significantly higher odds of in-hospital mortality (adjusted odds ratio [aOR] 1.40, p< 0.001), ICU stay (aOR 1.26, p< 0.001), AKI (aOR 1.08, p< 0.001), shock (aOR 1.40, p< 0.001), cardiac arrest (aOR 1.49, p< 0.001), and need for blood transfusion (aOR 1.04, p=0.048). There was no significant difference between groups in the likelihood of sepsis or VTE events. There was no statistically significant difference in LOS between groups; however, the HFrEF cohort had significantly higher mean hospitalization charges (+$2,017, p=0.004).
Discussion: We found that patients with HFrEF admitted for NVUGIB or LGIB have significantly worse outcomes and greater healthcare utilization than patients with HFpEF. Further studies to understand the pathophysiologic basis of these differences could provide insight into tailored therapy.
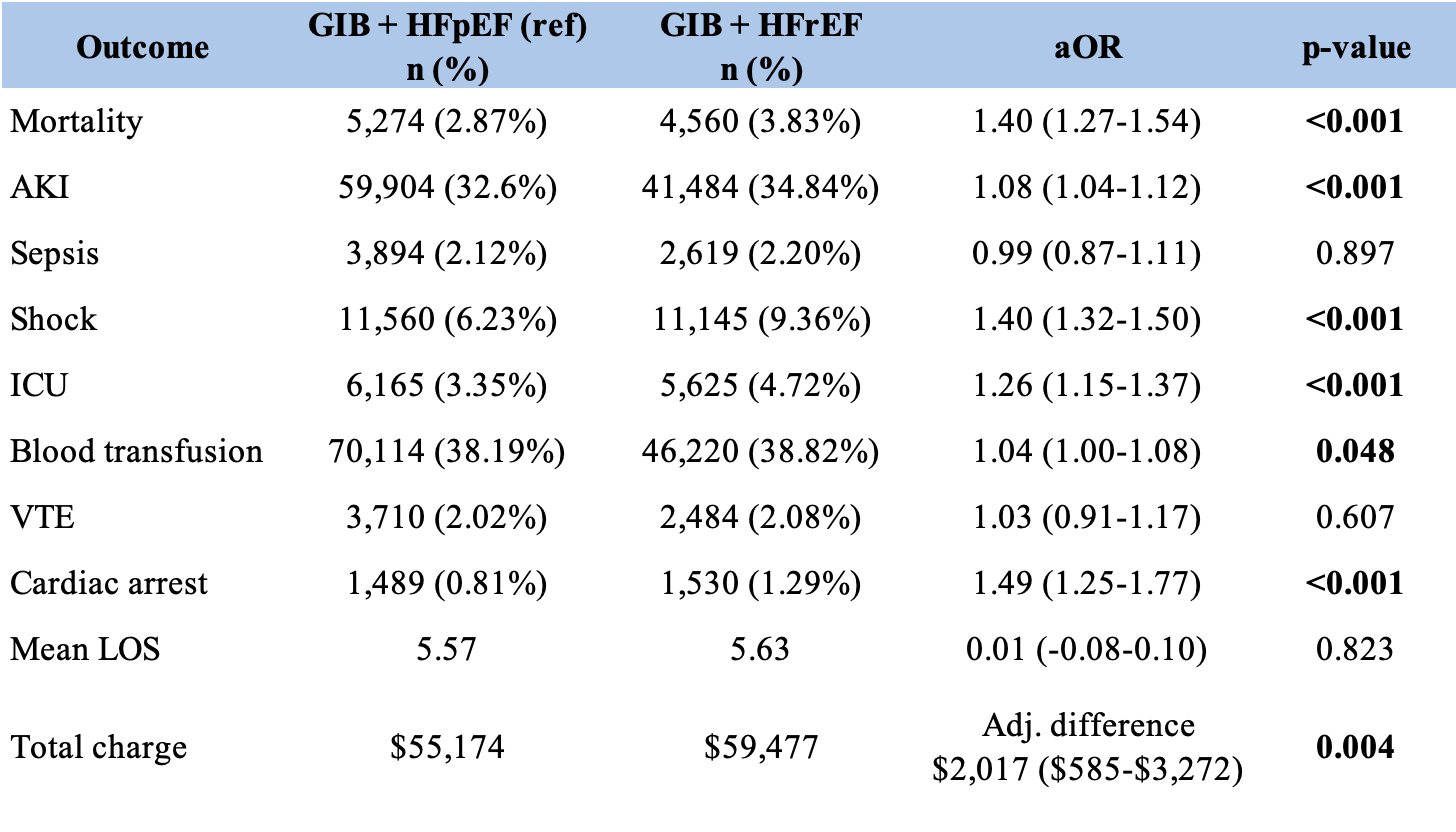
Figure: Baseline hospitalization characteristics for patients with gastrointestinal bleed stratified by heart failure type
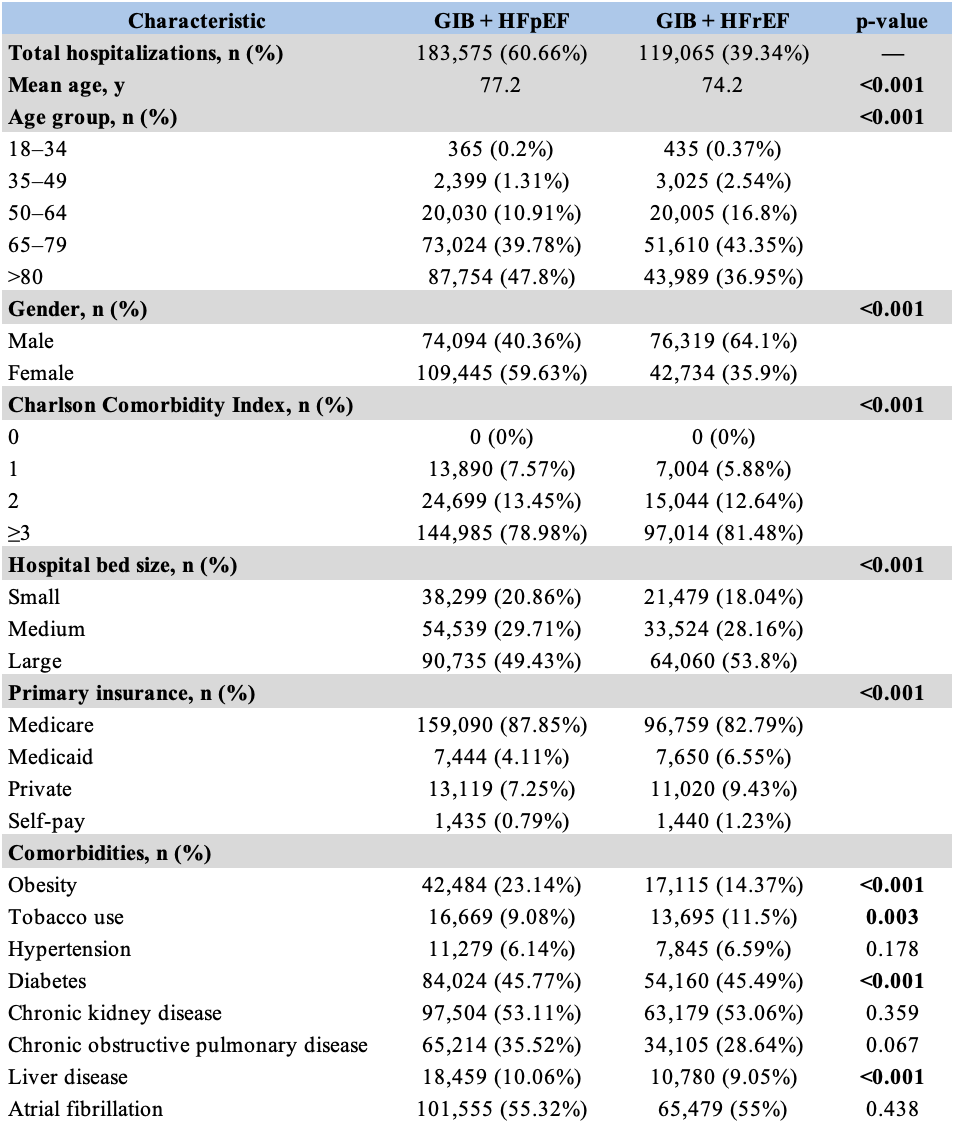
Figure: Outcomes, adverse events, and healthcare utilization
Disclosures:
Maria Grba indicated no relevant financial relationships.
Denise Nunez indicated no relevant financial relationships.
Patricia Zarza Gulino indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Saksham Kohli indicated no relevant financial relationships.
Gedion Yilma Amdetsion indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Daniel Guifarro Rivera indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Maria Grba, DO1, Denise Nunez, DO1, Patricia Zarza Gulino, MD1, Bhanu Siva Mohan Pinnam, MD1, Saksham Kohli, MBBS1, Gedion Yilma Amdetsion, MD2, Abhin Sapkota, MBBS1, Alejandro Nieto Dominguez, 2, Daniel Guifarro Rivera, MD3, Seema R. Gandhi, MD2. P5185 - Impact of Heart Failure Type on Outcomes in Patients Hospitalized for Gastrointestinal Bleeding: A National Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
