Tuesday Poster Session
Category: GI Bleeding
P5266 - A Case of Lower GI Bleeding Due to an Inverted Colonic Diverticulum
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Emily Minor, MD, PhD
University of Virginia
Charlottesville, VA
Presenting Author(s)
Emily Minor, MD, PhD1, Jacob A.. Frenchman, BS2, Brian Donahue, BA2, Vanessa Shami, MD, FACG3
1University of Virginia, Charlottesville, VA; 2University of Virginia School of Medicine, Charlottesville, VA; 3The University of Virginia, Charlottesville, VA
Introduction: Colonic diverticular bleeding is the leading cause of acute lower GI bleeds (LGIB), accounting for 20-40% of cases. Patients typically present with painless hematochezia, which self-resolves, and rarely requires endoscopic management. Inverted colon diverticula (ICD) occur in less than one percent of cases. They can be difficult to identify and treat given their polypoid appearance, and thus have an increased risk of iatrogenic complications, such as biopsy and resultant perforation. We present a unique case of an ICD with a visible vessel that was successfully treated with endoscopic banding ligation (EBL).
Case Description/
Methods: A 76-year-old male with chronic lymphocytic leukemia (not on treatment) and localized prostate cancer (not on anticoagulation) presented with acute onset large volume hematochezia. His labs were notable for a five-point drop in hemoglobin (from baseline of 14, down to 9). He underwent colonoscopy for suspected LGIB, which was significant for pan-colonic diverticulosis and a pale, ICD in the ascending colon with an actively bleeding vessel (Figures). The lesion was successfully treated with endoscopic band ligation with prompt hemostasis. The patient had no further episodes of bleeding, and was discharged the following day. At 2 weeks post-procedure, bleeding had not re-ocurred.
Discussion: Diverticular bleeds spontaneously resolve in 66-93% of cases and thus rarely require endoscopic intervention. However, when re-bleeding occurs, it increases healthcare utilization, morbidity, and mortality. Localization of a diverticular bleed is notably challenging, and optimal endoscopic management remains controversial, as coagulation, clipping, and ligation are regarded as equivalent in primary hemostasis and preventing early bleed recurrence.
In our case, after visualization of the bleeding ICD, it was carefully inspected to better classify the lesion as it appeared to mimic a polyp. However, under NBI imaging, the surface of the lesion was denuded and did not have any characteristics of a polyp; therefore, electrocautery and excision were not attempted. EBL was the chosen hemostatic modality as the ICD had a polypoid shape which was ideal for banding and this treatment modality is unlikely to cause perforation. We present a rare example of a successfully treated large-volume diverticular bleed due to an inverted colonic diverticulum with optimal anatomy for endoscopic band ligation.
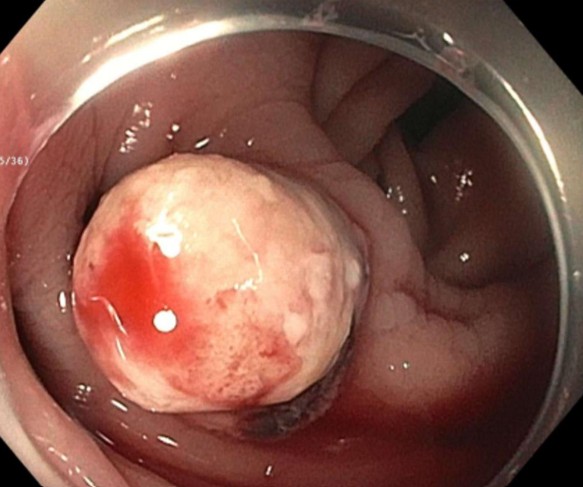
Figure: Inverted colonic diverticulum with visible bleeding vessel
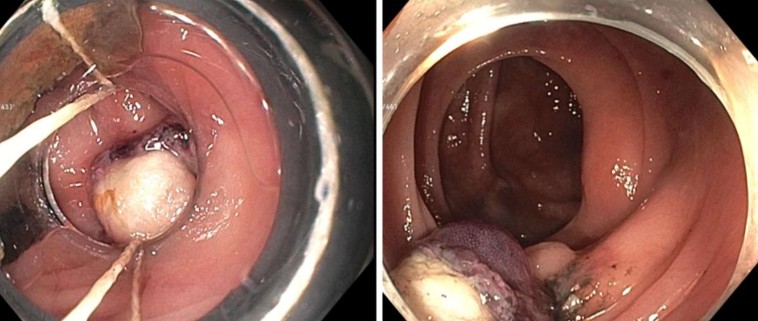
Figure: A: Inverted colonic diverticulum being treated with endoscopic band ligation. B: Inverted colonic diverticulum with successful hemostasis following endoscopic band ligation.
Disclosures:
Emily Minor indicated no relevant financial relationships.
Jacob Frenchman indicated no relevant financial relationships.
Brian Donahue indicated no relevant financial relationships.
Vanessa Shami: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus America – Consultant. Pentax America – Consultant.
Emily Minor, MD, PhD1, Jacob A.. Frenchman, BS2, Brian Donahue, BA2, Vanessa Shami, MD, FACG3. P5266 - A Case of Lower GI Bleeding Due to an Inverted Colonic Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Virginia, Charlottesville, VA; 2University of Virginia School of Medicine, Charlottesville, VA; 3The University of Virginia, Charlottesville, VA
Introduction: Colonic diverticular bleeding is the leading cause of acute lower GI bleeds (LGIB), accounting for 20-40% of cases. Patients typically present with painless hematochezia, which self-resolves, and rarely requires endoscopic management. Inverted colon diverticula (ICD) occur in less than one percent of cases. They can be difficult to identify and treat given their polypoid appearance, and thus have an increased risk of iatrogenic complications, such as biopsy and resultant perforation. We present a unique case of an ICD with a visible vessel that was successfully treated with endoscopic banding ligation (EBL).
Case Description/
Methods: A 76-year-old male with chronic lymphocytic leukemia (not on treatment) and localized prostate cancer (not on anticoagulation) presented with acute onset large volume hematochezia. His labs were notable for a five-point drop in hemoglobin (from baseline of 14, down to 9). He underwent colonoscopy for suspected LGIB, which was significant for pan-colonic diverticulosis and a pale, ICD in the ascending colon with an actively bleeding vessel (Figures). The lesion was successfully treated with endoscopic band ligation with prompt hemostasis. The patient had no further episodes of bleeding, and was discharged the following day. At 2 weeks post-procedure, bleeding had not re-ocurred.
Discussion: Diverticular bleeds spontaneously resolve in 66-93% of cases and thus rarely require endoscopic intervention. However, when re-bleeding occurs, it increases healthcare utilization, morbidity, and mortality. Localization of a diverticular bleed is notably challenging, and optimal endoscopic management remains controversial, as coagulation, clipping, and ligation are regarded as equivalent in primary hemostasis and preventing early bleed recurrence.
In our case, after visualization of the bleeding ICD, it was carefully inspected to better classify the lesion as it appeared to mimic a polyp. However, under NBI imaging, the surface of the lesion was denuded and did not have any characteristics of a polyp; therefore, electrocautery and excision were not attempted. EBL was the chosen hemostatic modality as the ICD had a polypoid shape which was ideal for banding and this treatment modality is unlikely to cause perforation. We present a rare example of a successfully treated large-volume diverticular bleed due to an inverted colonic diverticulum with optimal anatomy for endoscopic band ligation.
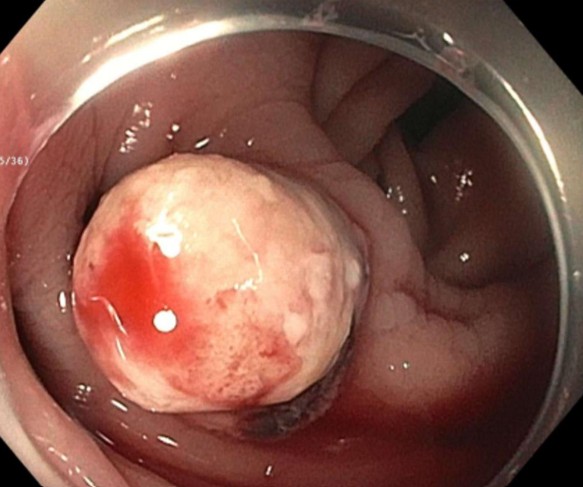
Figure: Inverted colonic diverticulum with visible bleeding vessel
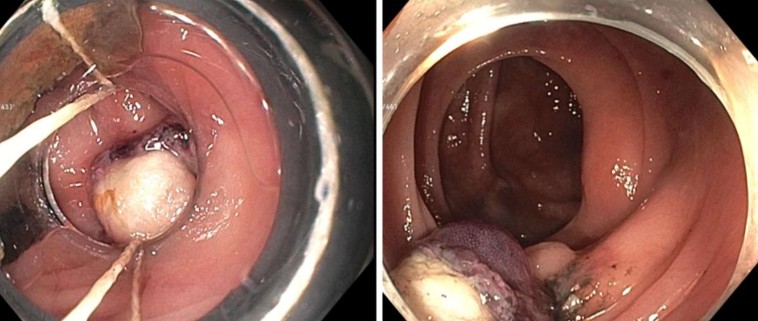
Figure: A: Inverted colonic diverticulum being treated with endoscopic band ligation. B: Inverted colonic diverticulum with successful hemostasis following endoscopic band ligation.
Disclosures:
Emily Minor indicated no relevant financial relationships.
Jacob Frenchman indicated no relevant financial relationships.
Brian Donahue indicated no relevant financial relationships.
Vanessa Shami: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus America – Consultant. Pentax America – Consultant.
Emily Minor, MD, PhD1, Jacob A.. Frenchman, BS2, Brian Donahue, BA2, Vanessa Shami, MD, FACG3. P5266 - A Case of Lower GI Bleeding Due to an Inverted Colonic Diverticulum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
