Tuesday Poster Session
Category: GI Bleeding
P5257 - Jejunal Diverticular Bleeding: From Diagnostic Challenges to the Need for Multimodal Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samar Pal S. Sandhu, MBBS
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Tanuj Chokshi, DO1, Brandon M. Cunha, BS2, Yasutoshi Shiratori, MD1, Seth Lapin, DO1
1Maimonides Medical Center, Brooklyn, NY; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ
Introduction: Jejunal diverticula can be asymptomatic or have symptoms ranging from abdominal pain, malabsorption, to acute emergencies such as obstruction, severe bleeding, or perforation. We present a case of a severe jejunal diverticular bleeding requiring multidisciplinary management.
Case Description/
Methods: A 75-year-old male with a history of hypertension, gout, chronic kidney disease, and rheumatoid arthritis was admitted with abdominal pain, maroon stools, and hemoglobin of 6.1 g/dL. Esophagogastroduodenoscopy (EGD) showed a gastric and duodenal ulcer without hemorrhage or perforation. However, the patient continued to have melena and became hemodynamically unstable, requiring a massive transfusion protocol (MTP). Angiography revealed a small area of dense vascularity in the right gastric artery, which was embolized.
Over the next few days, the patient continued to have melena and ongoing transfusion needs. CT angiography showed pooling of contrast within a jejunal diverticulum, and IR was reconsulted for embolization of the Superior mesenteric artery (SMA); however, the decision was deferred due to lack of collateral circulation and associated high risk of bowel ischemia and necrosis. A Push enteroscopy revealed a large jejunal diverticulum with active oozing from a visible vessel. Hemostasis was achieved using epinephrine injection, hot coagulation, and a topical hemostatic agent.
Within 24 hours, the patient developed acute abdominal pain and hypotension. CT angiography imaging demonstrated pneumoperitoneum consistent with visceral perforation. Emergent laparotomy revealed a perforated jejunal diverticulum, requiring resection with primary anastomosis. The patient stabilized postoperatively with no further bleeding. The patient then had a protracted stay with the development of deep venous thrombosis, necessitating an IVC filter placement.
Discussion: Jejunal diverticula are a rare but potentially life-threatening source of gastrointestinal bleeding. Their lower incidence is partly due to their anatomical location requiring interventions like capsule video endoscopy, single/double balloon enteroscopy, or angiography when hemodynamically significant for diagnosis and management. Our case highlights the challenges and complications ranging from the risk of ischemic injury from angiographic embolization to perforation from endoscopic intervention. Surgical intervention, though effective, is associated with increased morbidity. Thus, necessitating a multimodal case-based approach.

Figure: EGD showing non bleeding gastric and duodenal ulcer
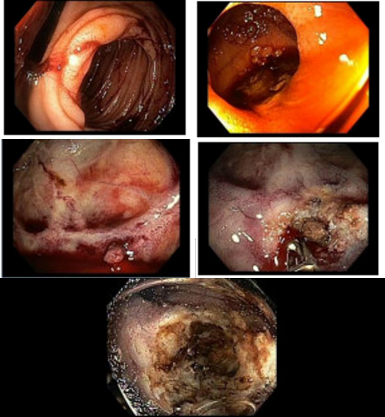
Figure: Push enteroscopy showing jejunal diverticular bleed before and after hemostasis
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Brandon Cunha indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Seth Lapin indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Tanuj Chokshi, DO1, Brandon M. Cunha, BS2, Yasutoshi Shiratori, MD1, Seth Lapin, DO1. P5257 - Jejunal Diverticular Bleeding: From Diagnostic Challenges to the Need for Multimodal Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Rowan-Virtua School of Osteopathic Medicine, Stratford, NJ
Introduction: Jejunal diverticula can be asymptomatic or have symptoms ranging from abdominal pain, malabsorption, to acute emergencies such as obstruction, severe bleeding, or perforation. We present a case of a severe jejunal diverticular bleeding requiring multidisciplinary management.
Case Description/
Methods: A 75-year-old male with a history of hypertension, gout, chronic kidney disease, and rheumatoid arthritis was admitted with abdominal pain, maroon stools, and hemoglobin of 6.1 g/dL. Esophagogastroduodenoscopy (EGD) showed a gastric and duodenal ulcer without hemorrhage or perforation. However, the patient continued to have melena and became hemodynamically unstable, requiring a massive transfusion protocol (MTP). Angiography revealed a small area of dense vascularity in the right gastric artery, which was embolized.
Over the next few days, the patient continued to have melena and ongoing transfusion needs. CT angiography showed pooling of contrast within a jejunal diverticulum, and IR was reconsulted for embolization of the Superior mesenteric artery (SMA); however, the decision was deferred due to lack of collateral circulation and associated high risk of bowel ischemia and necrosis. A Push enteroscopy revealed a large jejunal diverticulum with active oozing from a visible vessel. Hemostasis was achieved using epinephrine injection, hot coagulation, and a topical hemostatic agent.
Within 24 hours, the patient developed acute abdominal pain and hypotension. CT angiography imaging demonstrated pneumoperitoneum consistent with visceral perforation. Emergent laparotomy revealed a perforated jejunal diverticulum, requiring resection with primary anastomosis. The patient stabilized postoperatively with no further bleeding. The patient then had a protracted stay with the development of deep venous thrombosis, necessitating an IVC filter placement.
Discussion: Jejunal diverticula are a rare but potentially life-threatening source of gastrointestinal bleeding. Their lower incidence is partly due to their anatomical location requiring interventions like capsule video endoscopy, single/double balloon enteroscopy, or angiography when hemodynamically significant for diagnosis and management. Our case highlights the challenges and complications ranging from the risk of ischemic injury from angiographic embolization to perforation from endoscopic intervention. Surgical intervention, though effective, is associated with increased morbidity. Thus, necessitating a multimodal case-based approach.

Figure: EGD showing non bleeding gastric and duodenal ulcer
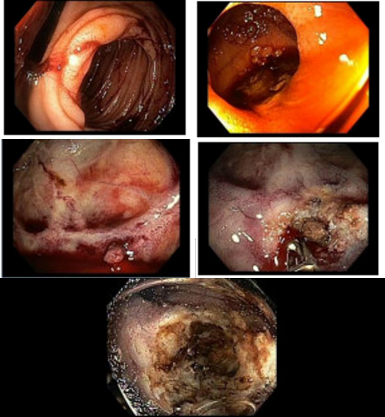
Figure: Push enteroscopy showing jejunal diverticular bleed before and after hemostasis
Disclosures:
Samar Pal Sandhu indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Brandon Cunha indicated no relevant financial relationships.
Yasutoshi Shiratori indicated no relevant financial relationships.
Seth Lapin indicated no relevant financial relationships.
Samar Pal S. Sandhu, MBBS1, Nakul Mahajan, MBBS1, Syed Mujtaba Baqir, MD1, Tanuj Chokshi, DO1, Brandon M. Cunha, BS2, Yasutoshi Shiratori, MD1, Seth Lapin, DO1. P5257 - Jejunal Diverticular Bleeding: From Diagnostic Challenges to the Need for Multimodal Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
