Tuesday Poster Session
Category: IBD
P5349 - The Association Between Lichen Planus and Inflammatory Bowel Disease: A Multicenter Population-Based Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AI
Abdulrahman Ibn Awadh, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Abdulrahman Ibn Awadh, MD1, Nawaf Alhazmi, MD1, Elleson Harper, BS1, Jaime A. Perez, PhD1, Gregory S. Cooper, MD2, Preetika Sinh, MD3, Jeffry A.. Katz, MD1, Fabio Cominelli, MD, PhD1, Miguel Regueiro, MD4, Emad Mansoor, MD1
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3Medical College of Wisconsin, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH
Introduction: Both lichen planus (LP) and inflammatory bowel disease (IBD) exhibit T cell-dominant immunopathology and are associated with autoimmune comorbidities. Despite conceptual links in immunological literature, original research examining associations between LP and IBD remains limited. This study assessed associations between IBD and lichen planus.
Methods: We accessed data through a large-scale health research network from 102 healthcare organizations across the United States, representing >150 million patients (TriNetX, Cambridge, MA; exempt from IRB review; data accessed April 28, 2025). We identified adult patients (≥18 years) with ≥2 instances of Crohn's disease (CD; ICD-10: K50) or ulcerative colitis (UC; ICD-10: K51). We excluded patients with one index diagnosis, both CD and UC diagnoses, and those with psoriasis (ICD-10: L40) or atopic dermatitis (ICD-10: L20). We collected patient demographics, medications, comorbidities, and lichen planus diagnoses (ICD-10: L43).
Results: We identified 160,343 CD patients and 146,970 UC patients. LP prevalence was 0.3% (n=446) in CD and 0.4% (n=546) in UC. LP diagnosis followed IBD diagnosis in 66.4% of CD and 63.4% of UC cases. IBD patients with LP were significantly older with female predominance. UC patients with LP showed high rates in the 70-80 age group (30.8% vs 11.8%). Higher viral infection prevalence was observed in IBD-LP patients, including COVID-19 (6.8% vs 2.3% in UC, p< 0.001; 6.7% vs 1.5% in CD, p< 0.001) and herpes zoster (6.6% vs 1.2% in UC, p< 0.001; 5.6% vs 0.8% in CD, p< 0.001). Hepatitis C was significantly more prevalent in IBD-LP patients. Known LP-triggering medications (NSAIDs, beta blockers, thiazides, ACE inhibitors) were more prevalent in IBD-LP patients.
Discussion: This analysis reveals significant associations between IBD and lichen planus with clinical implications. Results emphasize need for dermatologic surveillance in IBD patients, especially those receiving LP-triggering medications or with viral infections. Medication review should be standard for IBD patients developing LP. Older age and female predominance patterns may guide screening strategies, establishing IBD patients as high-risk for LP development.
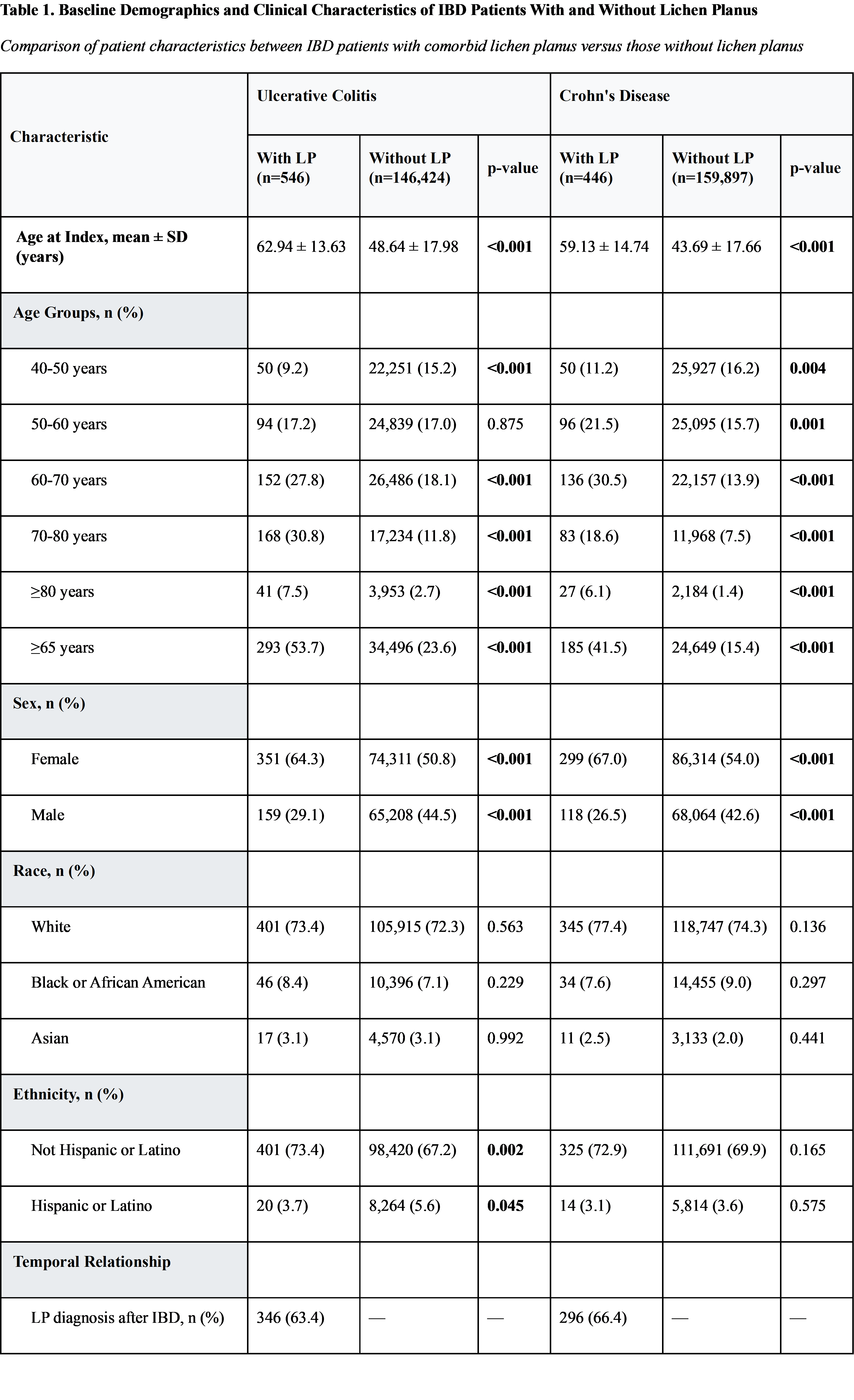
Figure: Abbreviations: IBD, inflammatory bowel disease; LP, lichen planus; SD, standard deviation.
Notes: Data presented as n (%) unless otherwise specified. P-values in bold indicate statistical significance (p < 0.05). Chi-square tests were used for categorical variables and t-tests for continuous variables. Missing data categories not shown for brevity.
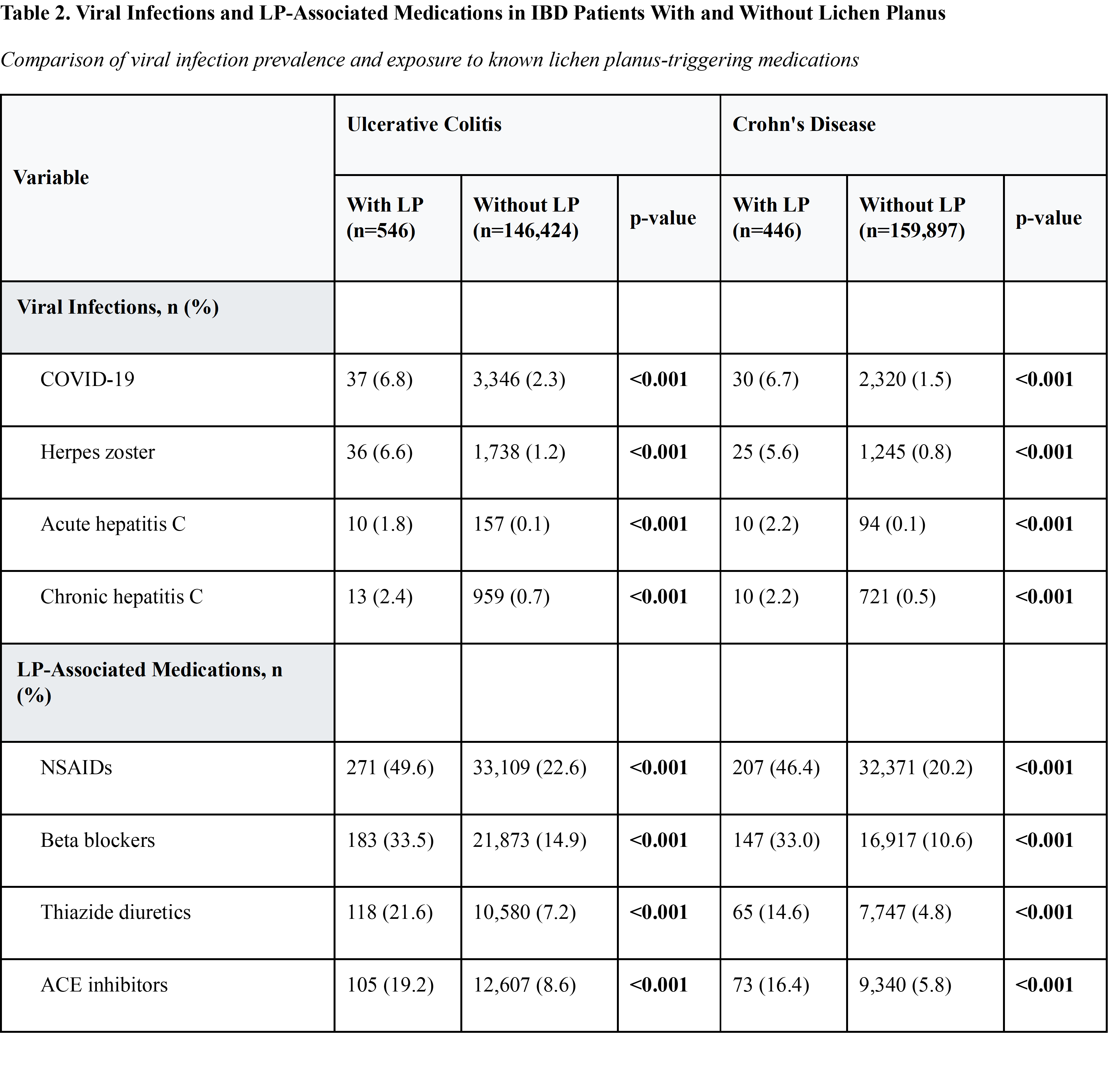
Figure: Abbreviations: ACE, angiotensin-converting enzyme; IBD, inflammatory bowel disease; LP, lichen planus; NSAIDs, nonsteroidal anti-inflammatory drugs.
Notes: Data presented as n (%). P-values in bold indicate statistical significance (p < 0.05). Chi-square tests were used for all comparisons. All medications listed are known triggers for lichen planus development. Viral infections were identified using ICD-10 diagnostic codes during the study period.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Preetika Sinh indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Miguel Regueiro indicated no relevant financial relationships.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Abdulrahman Ibn Awadh, MD1, Nawaf Alhazmi, MD1, Elleson Harper, BS1, Jaime A. Perez, PhD1, Gregory S. Cooper, MD2, Preetika Sinh, MD3, Jeffry A.. Katz, MD1, Fabio Cominelli, MD, PhD1, Miguel Regueiro, MD4, Emad Mansoor, MD1. P5349 - The Association Between Lichen Planus and Inflammatory Bowel Disease: A Multicenter Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 3Medical College of Wisconsin, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH
Introduction: Both lichen planus (LP) and inflammatory bowel disease (IBD) exhibit T cell-dominant immunopathology and are associated with autoimmune comorbidities. Despite conceptual links in immunological literature, original research examining associations between LP and IBD remains limited. This study assessed associations between IBD and lichen planus.
Methods: We accessed data through a large-scale health research network from 102 healthcare organizations across the United States, representing >150 million patients (TriNetX, Cambridge, MA; exempt from IRB review; data accessed April 28, 2025). We identified adult patients (≥18 years) with ≥2 instances of Crohn's disease (CD; ICD-10: K50) or ulcerative colitis (UC; ICD-10: K51). We excluded patients with one index diagnosis, both CD and UC diagnoses, and those with psoriasis (ICD-10: L40) or atopic dermatitis (ICD-10: L20). We collected patient demographics, medications, comorbidities, and lichen planus diagnoses (ICD-10: L43).
Results: We identified 160,343 CD patients and 146,970 UC patients. LP prevalence was 0.3% (n=446) in CD and 0.4% (n=546) in UC. LP diagnosis followed IBD diagnosis in 66.4% of CD and 63.4% of UC cases. IBD patients with LP were significantly older with female predominance. UC patients with LP showed high rates in the 70-80 age group (30.8% vs 11.8%). Higher viral infection prevalence was observed in IBD-LP patients, including COVID-19 (6.8% vs 2.3% in UC, p< 0.001; 6.7% vs 1.5% in CD, p< 0.001) and herpes zoster (6.6% vs 1.2% in UC, p< 0.001; 5.6% vs 0.8% in CD, p< 0.001). Hepatitis C was significantly more prevalent in IBD-LP patients. Known LP-triggering medications (NSAIDs, beta blockers, thiazides, ACE inhibitors) were more prevalent in IBD-LP patients.
Discussion: This analysis reveals significant associations between IBD and lichen planus with clinical implications. Results emphasize need for dermatologic surveillance in IBD patients, especially those receiving LP-triggering medications or with viral infections. Medication review should be standard for IBD patients developing LP. Older age and female predominance patterns may guide screening strategies, establishing IBD patients as high-risk for LP development.
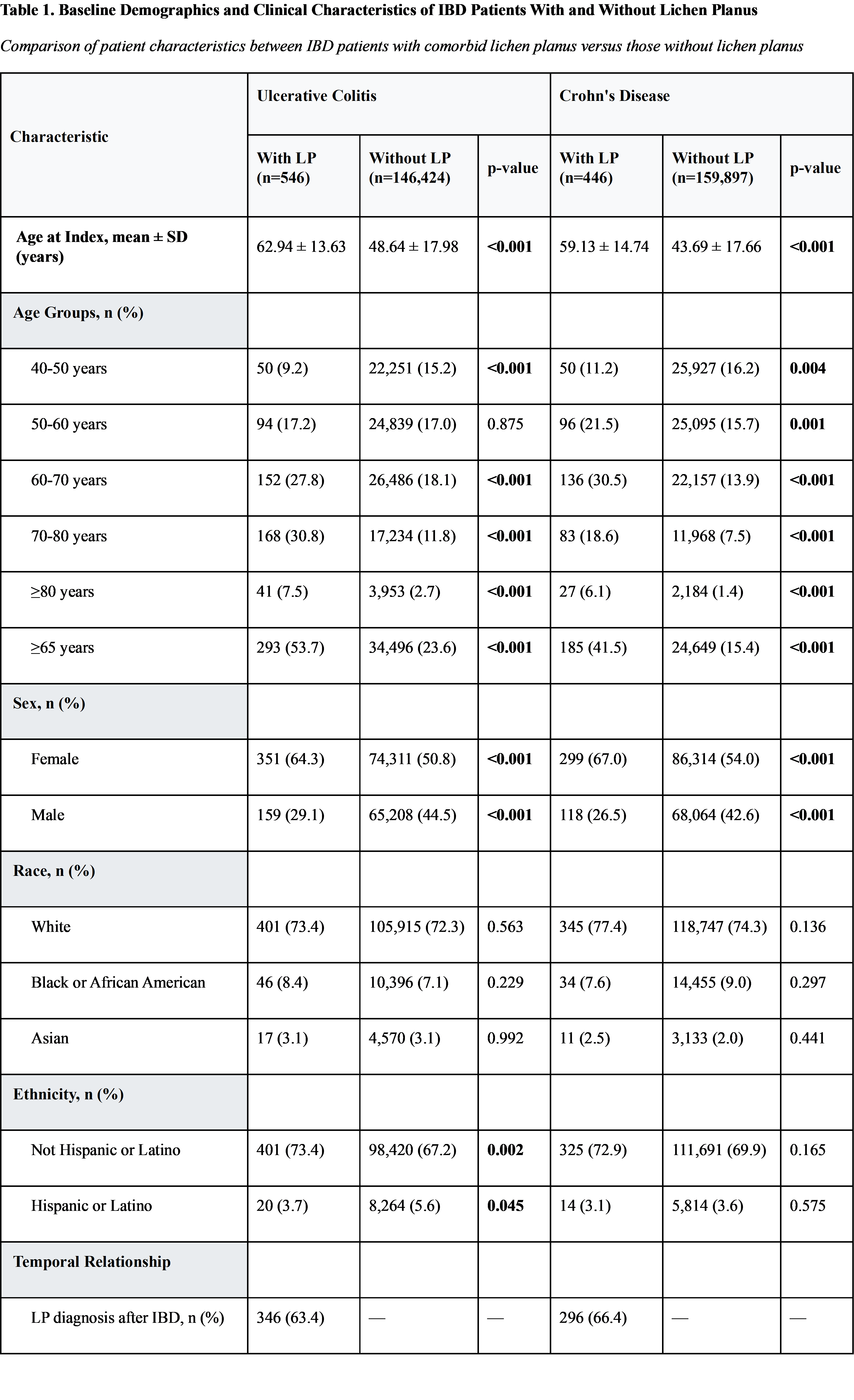
Figure: Abbreviations: IBD, inflammatory bowel disease; LP, lichen planus; SD, standard deviation.
Notes: Data presented as n (%) unless otherwise specified. P-values in bold indicate statistical significance (p < 0.05). Chi-square tests were used for categorical variables and t-tests for continuous variables. Missing data categories not shown for brevity.
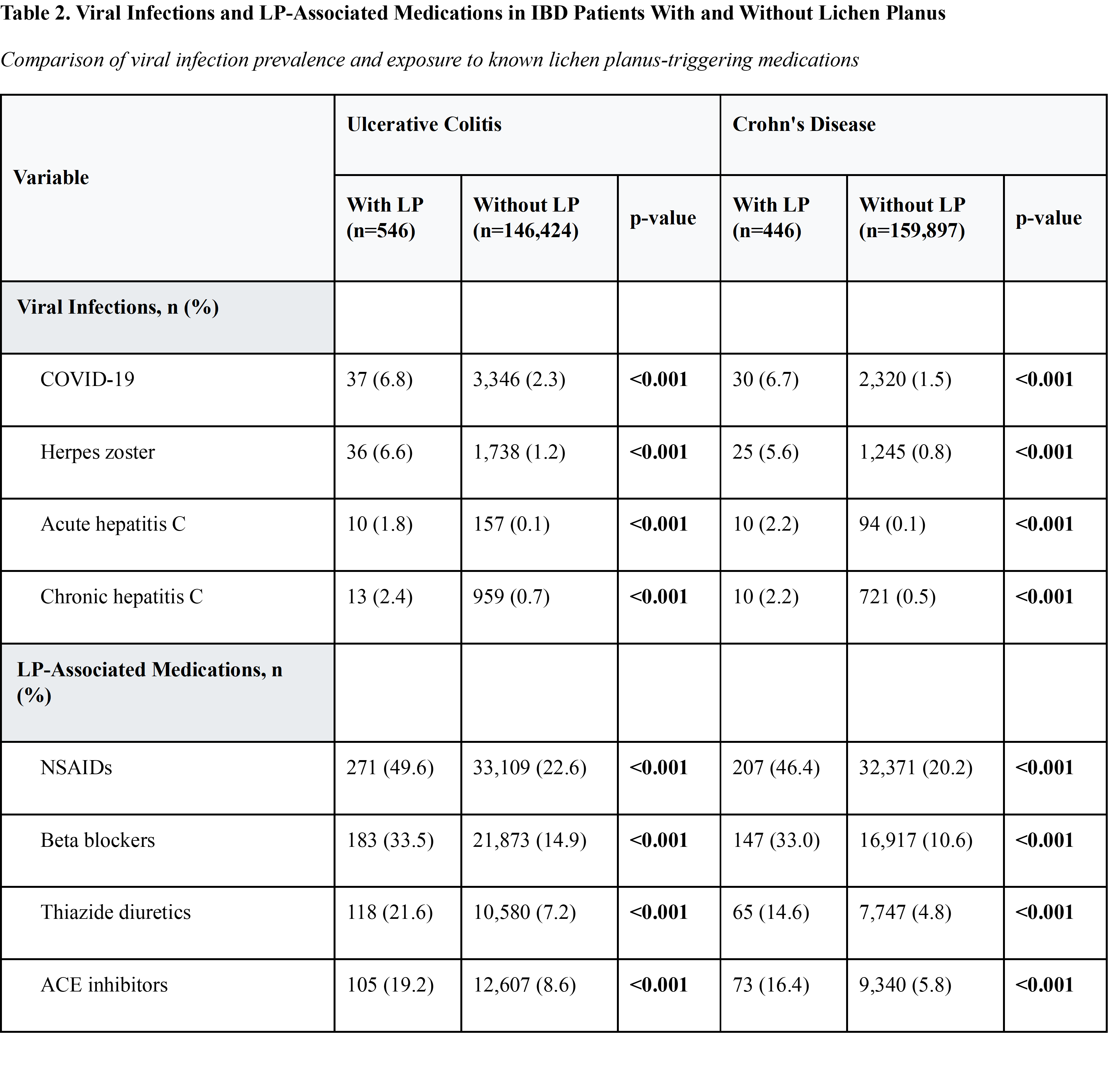
Figure: Abbreviations: ACE, angiotensin-converting enzyme; IBD, inflammatory bowel disease; LP, lichen planus; NSAIDs, nonsteroidal anti-inflammatory drugs.
Notes: Data presented as n (%). P-values in bold indicate statistical significance (p < 0.05). Chi-square tests were used for all comparisons. All medications listed are known triggers for lichen planus development. Viral infections were identified using ICD-10 diagnostic codes during the study period.
Disclosures:
Abdulrahman Ibn Awadh indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Preetika Sinh indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Fabio Cominelli indicated no relevant financial relationships.
Miguel Regueiro indicated no relevant financial relationships.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Abdulrahman Ibn Awadh, MD1, Nawaf Alhazmi, MD1, Elleson Harper, BS1, Jaime A. Perez, PhD1, Gregory S. Cooper, MD2, Preetika Sinh, MD3, Jeffry A.. Katz, MD1, Fabio Cominelli, MD, PhD1, Miguel Regueiro, MD4, Emad Mansoor, MD1. P5349 - The Association Between Lichen Planus and Inflammatory Bowel Disease: A Multicenter Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
