Tuesday Poster Session
Category: IBD
P5348 - Post Arthroplasty Surgical Outcomes in Patients With Inflammatory Bowel Disease on Advanced Therapies
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PL
Passisd Laoveeravat, MD
University of Kentucky
Jacksonville, FL
Presenting Author(s)
Passisd Laoveeravat, MD1, Tarek Odah, MD, MPH2, Jana G. Hashash, MD, MSc, FACG2, Francis A.. Farraye, MD, MSc, MACG2
1University of Kentucky, Lexington, KY; 2Mayo Clinic, Jacksonville, FL
Introduction: The impact of corticosteroid and biologic therapy use amongst patients with IBD on postoperative complications in arthroplasties remains uncertain. This study aims to evaluate the association between preoperative corticosteroids or biologic use in patients with IBD and the risk of prosthetic joint infections (PJI), prosthesis dislocation, and wound disruption following arthroplasty.
Methods: This retrospective cohort study utilized TriNetX, a large real-world database, to examine postoperative complications in patients with IBD undergoing hip or knee arthroplasty. Patients prescribed corticosteroids, anti tumor necrosis factors (TNFs), or other IBD biologic therapies, within 3 months prior to surgery were included. Each group was matched 1:1 to controls who did not receive therapies using propensity scores. Outcomes included early and late PJI, prosthesis dislocation, and wound disruption.
Results: Among 3,222 patients on non steroid biologic therapies for IBD and controls, we found the increased dislocation risk, 1.48% vs 0.9% (OR:1.67, 95%CI: 1.06–2.63, p=0.027). Early PJI (< 3 months) occurred in 1.57% vs 1.08% (OR:1.47, 95% CI: 0.94–2.28, p=0.087). Of 3,404 patients, late PJI (3–12 months) occurred in 0.62% vs 0.46% (OR:1.36, 95%CI: 0.69–2.65, p=0.373). Wound disruption was 1.71% vs 1.16% (OR:1.48, 95%CI: 0.97–2.26, p=0.065).
In a subgroup of 2,338 patients on anti TNFs, early PJI was 1.36% vs 1.26% (OR:1.08, 95% CI: 0.65–1.80, p=0.76), wound disruption 1.53% vs 1.65% (OR:0.93, 95% CI: 0.58–1.47, p=0.75). The dislocation was significantly higher in the anti TNF group (1.31% vs 0.57%, OR:2.33, 95% CI: 1.41–4.74, p=0.02).
Of 4,475 patients with IBD on corticosteroids, the early PJI risk was increased, 1.12% vs 0.66% (OR:1.71, 95% CI: 1.08–2.72, p=0.021). The dislocation rate was also higher with 1.21% vs 0.52% (OR:2.34, 95% CI: 1.43–3.83, p=0.001). Wound disruption was 1.23% vs 1.07% (OR:1.16, 95% CI: 0.78–1.72, p=0.466) (Table 1).
Discussion: Preoperative steroid use in patients with IBD was associated with increased risks of PJI and dislocation after arthroplasty. Preoperative use of anti-TNFs was not associated with infection or wound complications, though anti-TNF and other biologics were associated with higher dislocation risk. These findings highlight the importance of individualized perioperative management to mitigate surgical complications while maintaining IBD control. Further research is needed to optimize surgical guidelines for patients with IBD undergoing arthroplasty.
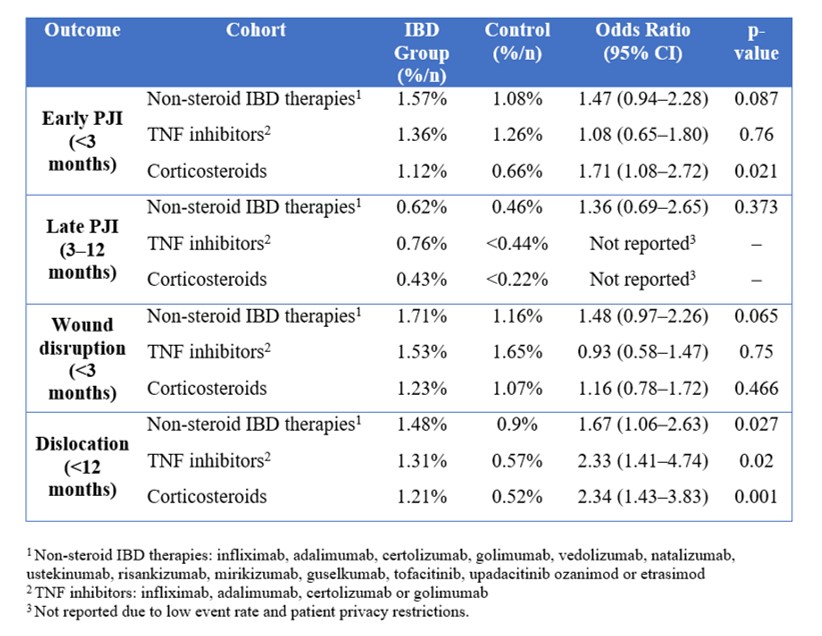
Figure: Table 1. Impact of Preoperative IBD Therapies on Arthroplasty Outcomes
Disclosures:
Passisd Laoveeravat indicated no relevant financial relationships.
Tarek Odah indicated no relevant financial relationships.
Jana Hashash: BMS – Ad Board.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Passisd Laoveeravat, MD1, Tarek Odah, MD, MPH2, Jana G. Hashash, MD, MSc, FACG2, Francis A.. Farraye, MD, MSc, MACG2. P5348 - Post Arthroplasty Surgical Outcomes in Patients With Inflammatory Bowel Disease on Advanced Therapies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2Mayo Clinic, Jacksonville, FL
Introduction: The impact of corticosteroid and biologic therapy use amongst patients with IBD on postoperative complications in arthroplasties remains uncertain. This study aims to evaluate the association between preoperative corticosteroids or biologic use in patients with IBD and the risk of prosthetic joint infections (PJI), prosthesis dislocation, and wound disruption following arthroplasty.
Methods: This retrospective cohort study utilized TriNetX, a large real-world database, to examine postoperative complications in patients with IBD undergoing hip or knee arthroplasty. Patients prescribed corticosteroids, anti tumor necrosis factors (TNFs), or other IBD biologic therapies, within 3 months prior to surgery were included. Each group was matched 1:1 to controls who did not receive therapies using propensity scores. Outcomes included early and late PJI, prosthesis dislocation, and wound disruption.
Results: Among 3,222 patients on non steroid biologic therapies for IBD and controls, we found the increased dislocation risk, 1.48% vs 0.9% (OR:1.67, 95%CI: 1.06–2.63, p=0.027). Early PJI (< 3 months) occurred in 1.57% vs 1.08% (OR:1.47, 95% CI: 0.94–2.28, p=0.087). Of 3,404 patients, late PJI (3–12 months) occurred in 0.62% vs 0.46% (OR:1.36, 95%CI: 0.69–2.65, p=0.373). Wound disruption was 1.71% vs 1.16% (OR:1.48, 95%CI: 0.97–2.26, p=0.065).
In a subgroup of 2,338 patients on anti TNFs, early PJI was 1.36% vs 1.26% (OR:1.08, 95% CI: 0.65–1.80, p=0.76), wound disruption 1.53% vs 1.65% (OR:0.93, 95% CI: 0.58–1.47, p=0.75). The dislocation was significantly higher in the anti TNF group (1.31% vs 0.57%, OR:2.33, 95% CI: 1.41–4.74, p=0.02).
Of 4,475 patients with IBD on corticosteroids, the early PJI risk was increased, 1.12% vs 0.66% (OR:1.71, 95% CI: 1.08–2.72, p=0.021). The dislocation rate was also higher with 1.21% vs 0.52% (OR:2.34, 95% CI: 1.43–3.83, p=0.001). Wound disruption was 1.23% vs 1.07% (OR:1.16, 95% CI: 0.78–1.72, p=0.466) (Table 1).
Discussion: Preoperative steroid use in patients with IBD was associated with increased risks of PJI and dislocation after arthroplasty. Preoperative use of anti-TNFs was not associated with infection or wound complications, though anti-TNF and other biologics were associated with higher dislocation risk. These findings highlight the importance of individualized perioperative management to mitigate surgical complications while maintaining IBD control. Further research is needed to optimize surgical guidelines for patients with IBD undergoing arthroplasty.
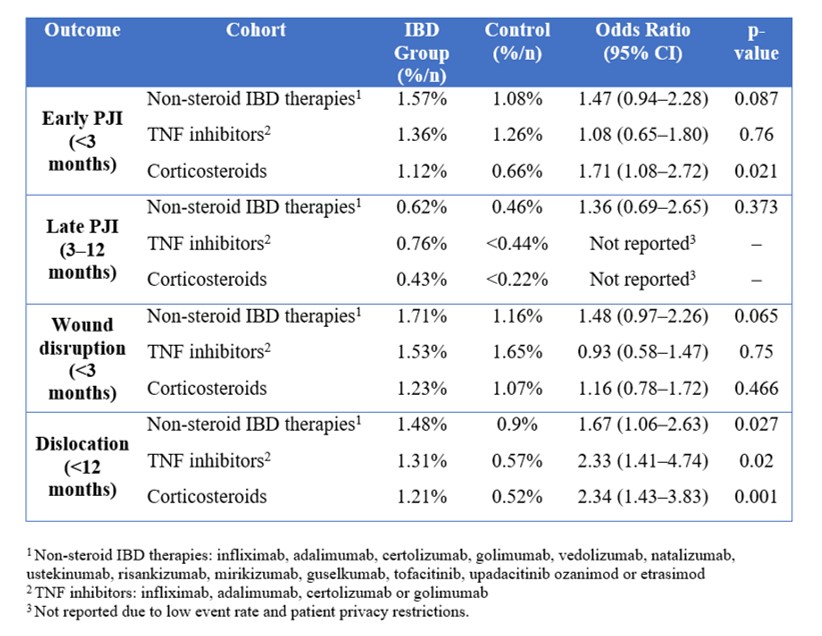
Figure: Table 1. Impact of Preoperative IBD Therapies on Arthroplasty Outcomes
Disclosures:
Passisd Laoveeravat indicated no relevant financial relationships.
Tarek Odah indicated no relevant financial relationships.
Jana Hashash: BMS – Ad Board.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Passisd Laoveeravat, MD1, Tarek Odah, MD, MPH2, Jana G. Hashash, MD, MSc, FACG2, Francis A.. Farraye, MD, MSc, MACG2. P5348 - Post Arthroplasty Surgical Outcomes in Patients With Inflammatory Bowel Disease on Advanced Therapies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

