Tuesday Poster Session
Category: IBD
P5417 - Empiric Antibiotic Use With Rescue Infliximab Does Not Improve Outcomes in Acute Severe Ulcerative Colitis: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Dominic Ofosu-Amakye, MD (he/him/his)
Piedmont Athens Regional Medical Centre
Collierville, TN
Presenting Author(s)
Kofi Clarke, MD1, Dominic Ofosu-Amakye, MD2, Shannon Dalessio, MSc1, Kara Dijoseph, MD1, Emmanuelle Williams, MD1, Andrew Tinsley, MD1, Matthew Coates, MD, PhD3
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Piedmont Athens Regional Medical Centre, Athens, GA; 3Penn State College of Medicine, Hershey, PA
Introduction: Acute Severe Ulcerative Colitis (ASUC) can be life-threatening and may result in poor outcomes. Approximately 30–50% of patients fail to respond to initial corticosteroid treatment and infliximab is often used as rescue therapy. In clinical settings, antibiotics are sometimes empirically administered with infliximab, though evidence supporting improved outcomes is lacking. We evaluated the impact of concurrent antibiotic use with infliximab in ASUC.
Methods: A retrospective cohort study was conducted using the TriNetX platform. ICD-10 code K51, procedure codes, visit diagnosis codes, and keywords such as “antibiotics” and “infliximab” were used to identify eligible patients from 01/01/2013 to 12/31/2022.
We compared 2 cohorts
Propensity score matching was performed for baseline characteristics. Primary outcome was all-cause mortality. Secondary outcomes included IBD-related surgery, ICU care, emergency department (ED) utilization, and sepsis.
Results: A total of 1,028 patients out of 2,788 met criteria and were included in the analysis.
Table 1 summarizes baseline characteristics. Males formed the majority (51.5% in Cohort 1, 53.3% in Cohort 2); mean age was 40 years in both groups.
Table 2 summarizes outcomes: A total of 10 deaths occurred in each group (risk difference = 0; OR = 1.0). 39 patients in Cohort 1 vs. 29 in Cohort 2 developed sepsis (risk difference = 0.973%; OR = 1.3; 95% CI: 0.833–2.214).
Discussion: Mucosal injury in ASUC may lead to bacterial translocation, with increased risk of sepsis. This has prompted empiric antibiotic use in clinical practice.
There was no difference in mortality or major outcomes between patients who did and did not receive antibiotics with infliximab. Antibiotic use was not associated with reduced sepsis risk and may contribute to higher healthcare costs and antimicrobial resistance. These results highlight the importance of antimicrobial stewardship and the need for further prospective studies.
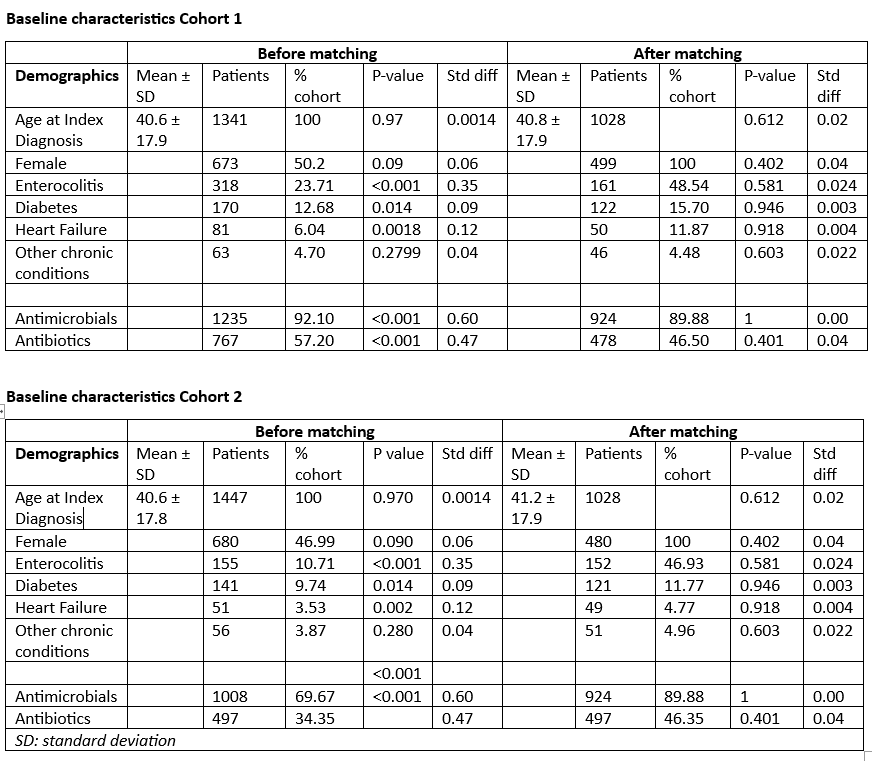
Figure: Table 1 baseline characteristics of study participants
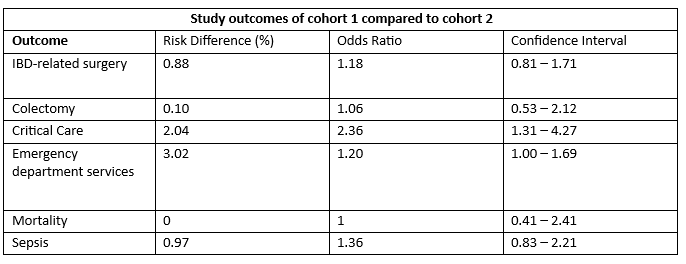
Figure: Study Outcomes of cohort 1 compared to cohort 2
Disclosures:
Kofi Clarke: Takeda – Clinical Trial Support.
Dominic Ofosu-Amakye indicated no relevant financial relationships.
Shannon Dalessio indicated no relevant financial relationships.
Kara Dijoseph indicated no relevant financial relationships.
Emmanuelle Williams indicated no relevant financial relationships.
Andrew Tinsley indicated no relevant financial relationships.
Matthew Coates indicated no relevant financial relationships.
Kofi Clarke, MD1, Dominic Ofosu-Amakye, MD2, Shannon Dalessio, MSc1, Kara Dijoseph, MD1, Emmanuelle Williams, MD1, Andrew Tinsley, MD1, Matthew Coates, MD, PhD3. P5417 - Empiric Antibiotic Use With Rescue Infliximab Does Not Improve Outcomes in Acute Severe Ulcerative Colitis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Piedmont Athens Regional Medical Centre, Athens, GA; 3Penn State College of Medicine, Hershey, PA
Introduction: Acute Severe Ulcerative Colitis (ASUC) can be life-threatening and may result in poor outcomes. Approximately 30–50% of patients fail to respond to initial corticosteroid treatment and infliximab is often used as rescue therapy. In clinical settings, antibiotics are sometimes empirically administered with infliximab, though evidence supporting improved outcomes is lacking. We evaluated the impact of concurrent antibiotic use with infliximab in ASUC.
Methods: A retrospective cohort study was conducted using the TriNetX platform. ICD-10 code K51, procedure codes, visit diagnosis codes, and keywords such as “antibiotics” and “infliximab” were used to identify eligible patients from 01/01/2013 to 12/31/2022.
We compared 2 cohorts
- 1: Patients who received infliximab on or within one day of admission and antibiotics on or within one day after infliximab administration (n = 1,341).
- 2: Patients who received infliximab on or within one day of admission but did not receive antibiotics within three days after infliximab administration (n = 1,447).
Propensity score matching was performed for baseline characteristics. Primary outcome was all-cause mortality. Secondary outcomes included IBD-related surgery, ICU care, emergency department (ED) utilization, and sepsis.
Results: A total of 1,028 patients out of 2,788 met criteria and were included in the analysis.
Table 1 summarizes baseline characteristics. Males formed the majority (51.5% in Cohort 1, 53.3% in Cohort 2); mean age was 40 years in both groups.
Table 2 summarizes outcomes: A total of 10 deaths occurred in each group (risk difference = 0; OR = 1.0). 39 patients in Cohort 1 vs. 29 in Cohort 2 developed sepsis (risk difference = 0.973%; OR = 1.3; 95% CI: 0.833–2.214).
Discussion: Mucosal injury in ASUC may lead to bacterial translocation, with increased risk of sepsis. This has prompted empiric antibiotic use in clinical practice.
There was no difference in mortality or major outcomes between patients who did and did not receive antibiotics with infliximab. Antibiotic use was not associated with reduced sepsis risk and may contribute to higher healthcare costs and antimicrobial resistance. These results highlight the importance of antimicrobial stewardship and the need for further prospective studies.
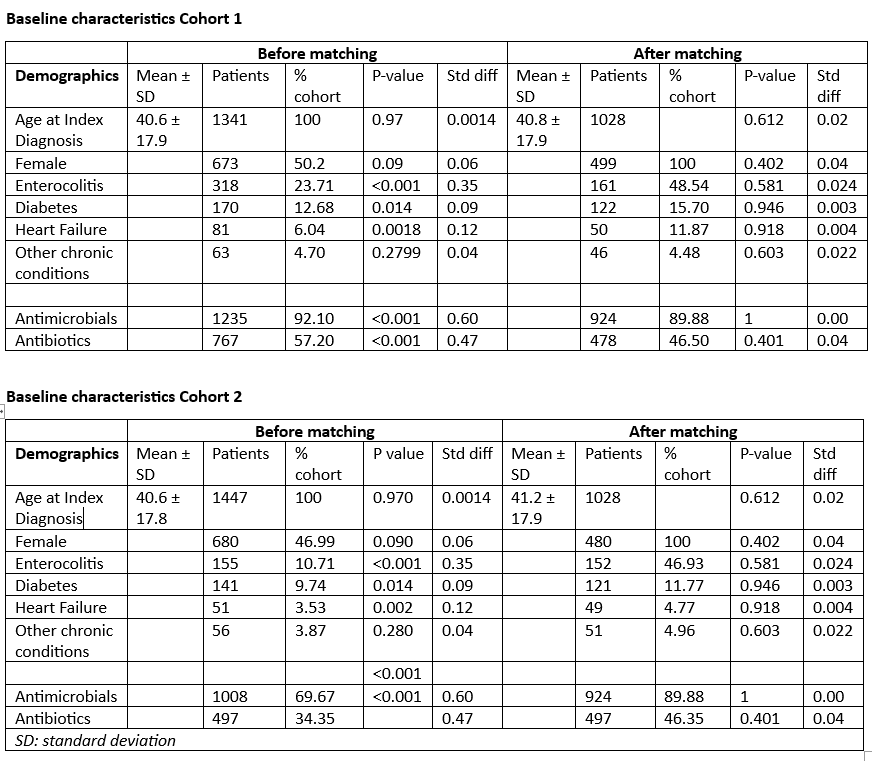
Figure: Table 1 baseline characteristics of study participants
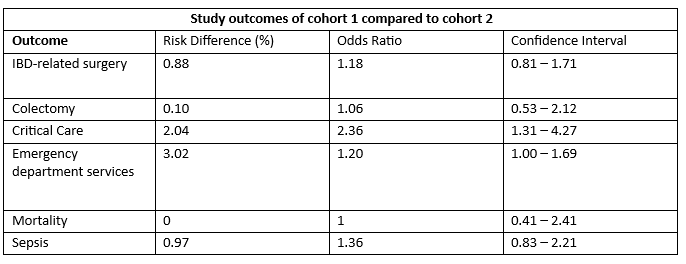
Figure: Study Outcomes of cohort 1 compared to cohort 2
Disclosures:
Kofi Clarke: Takeda – Clinical Trial Support.
Dominic Ofosu-Amakye indicated no relevant financial relationships.
Shannon Dalessio indicated no relevant financial relationships.
Kara Dijoseph indicated no relevant financial relationships.
Emmanuelle Williams indicated no relevant financial relationships.
Andrew Tinsley indicated no relevant financial relationships.
Matthew Coates indicated no relevant financial relationships.
Kofi Clarke, MD1, Dominic Ofosu-Amakye, MD2, Shannon Dalessio, MSc1, Kara Dijoseph, MD1, Emmanuelle Williams, MD1, Andrew Tinsley, MD1, Matthew Coates, MD, PhD3. P5417 - Empiric Antibiotic Use With Rescue Infliximab Does Not Improve Outcomes in Acute Severe Ulcerative Colitis: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
