Tuesday Poster Session
Category: IBD
P5416 - Cervical Cancer Screening Rates Among Females With Inflammatory Bowel Disease Receiving Immunosuppressive Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taylor A. Karl, MD (she/her/hers)
University of Colorado Anschutz Medical Campus
Durham, NC
Presenting Author(s)
Taylor A. Karl, MD1, Nancy Wu, MD, PhD2, Frank I. Scott, MD, MSCE3
1University of Colorado Anschutz Medical Campus, Durham, NC; 2University of Colorado Anschutz Medical Campus, Englewood, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO
Introduction: Cervical cancer is the fourth most common cancer among females globally with incidence rates (IRs) exceeding World Health Organization targets. Most cases result from oncogenic human papilloma virus (HPV) infection. Since HPV vaccines do not prevent all high-risk strains, secondary prevention with screening is crucial. Females with inflammatory bowel disease (IBD) on immunosuppression (IS) may face a higher risk for persistent HPV infection and cervical cancer. Limited data exist on cervical cancer screening rates in US females with IBD on IS, especially in the post-HPV vaccine era, and under current guidelines. We examined the IR of cervical cancer screening in females with IBD on IS.
Methods: We conducted a retrospective cohort study of females with IBD on IS at a tertiary academic medical center from January 1, 2016, to December 31, 2023. Eligible patients were assigned female at birth, aged 18-65 years, diagnosed with IBD, and followed in gastroenterology clinic for ≤ 1 year. Exclusion criteria included prior hysterectomy, abnormal results prior to IS, or IS use for secondary reasons. Collected data included demographics, IBD characteristics, IBD therapy, HPV vaccination, and contraceptive use. Screening adherence was defined by the 2022 Crohn’s and Colitis Foundation Health Maintenance Checklist. Nonadherence was defined as failure to maintain annual pap cytology or cytology with HPV co-testing every three years. Wilcoxon rank sum, Fischer’s exact, and chi-squared tests evaluated differences between groups. The IR was calculated using total screening events per total person-time. The exact Poisson test compared the observed IR to the lower bound of the recommended reference rate, 33.3 per 100 person-years.
Results: We identified 195 female patients on IS. Nonadherence to cervical cancer screening occurred in 56.9% of patients. Shorter follow-up, private insurance status, non-smoking history, and intrauterine device use were significantly associated with adherence (Table 1). The IR for cervical cancer screening was 24.3 per 100 person-years (p = 0.0003, 95% CI 0.238, 0.302).
Discussion: Females with IBD on IS at a tertiary academic center undergo cervical cancer screening significantly less frequently than recommended. Future analyses will assess incidence rates in a diverse population, rates of abnormal screening outcomes, and adjusted predictors of nonadherence using multivariable regression.
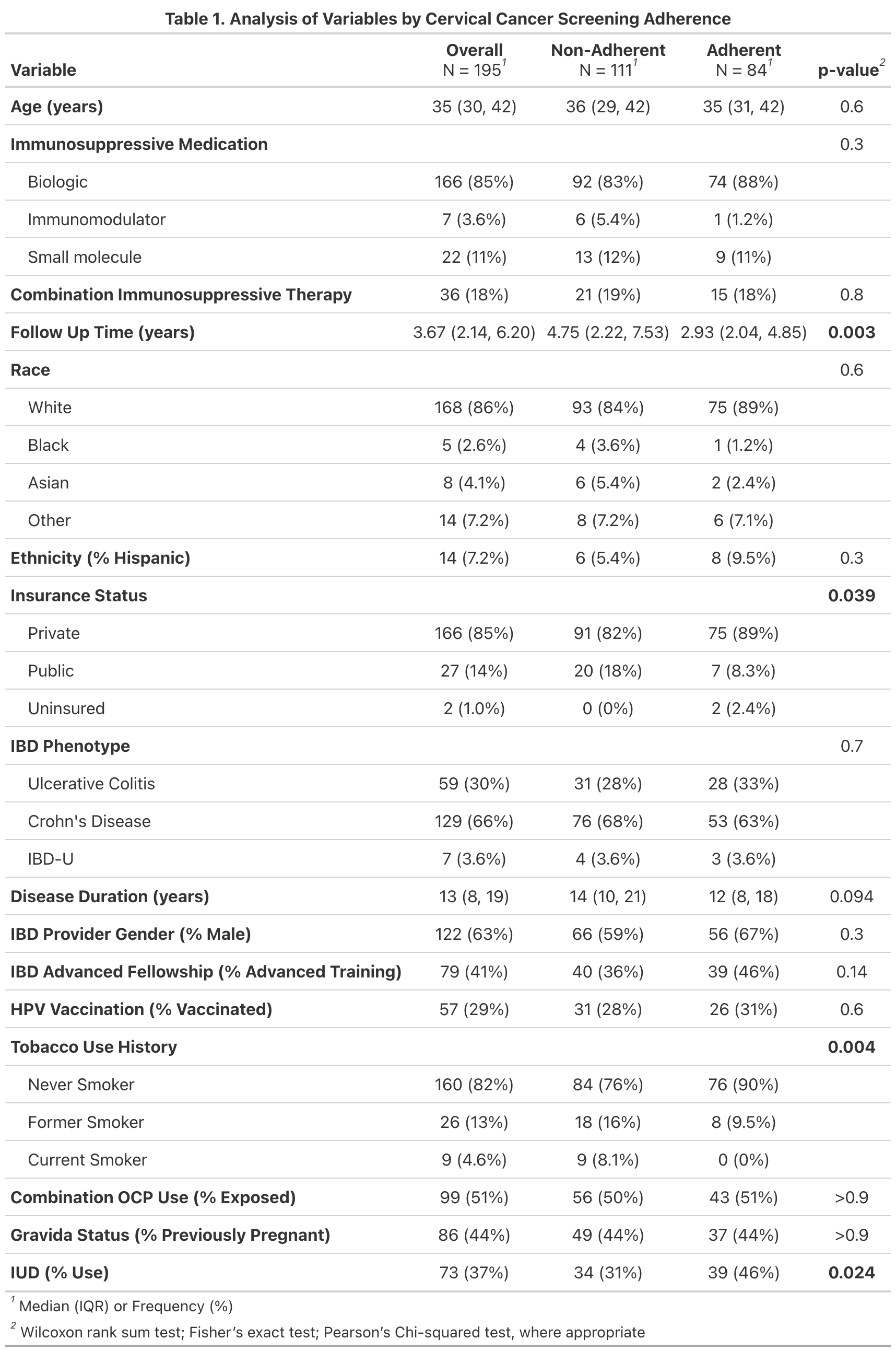
Figure: Table 1. Analysis of Variables by Cervical Cancer Screening Adherence
Disclosures:
Taylor Karl indicated no relevant financial relationships.
Nancy Wu indicated no relevant financial relationships.
Frank Scott indicated no relevant financial relationships.
Taylor A. Karl, MD1, Nancy Wu, MD, PhD2, Frank I. Scott, MD, MSCE3. P5416 - Cervical Cancer Screening Rates Among Females With Inflammatory Bowel Disease Receiving Immunosuppressive Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Durham, NC; 2University of Colorado Anschutz Medical Campus, Englewood, CO; 3University of Colorado Anschutz Medical Campus, Aurora, CO
Introduction: Cervical cancer is the fourth most common cancer among females globally with incidence rates (IRs) exceeding World Health Organization targets. Most cases result from oncogenic human papilloma virus (HPV) infection. Since HPV vaccines do not prevent all high-risk strains, secondary prevention with screening is crucial. Females with inflammatory bowel disease (IBD) on immunosuppression (IS) may face a higher risk for persistent HPV infection and cervical cancer. Limited data exist on cervical cancer screening rates in US females with IBD on IS, especially in the post-HPV vaccine era, and under current guidelines. We examined the IR of cervical cancer screening in females with IBD on IS.
Methods: We conducted a retrospective cohort study of females with IBD on IS at a tertiary academic medical center from January 1, 2016, to December 31, 2023. Eligible patients were assigned female at birth, aged 18-65 years, diagnosed with IBD, and followed in gastroenterology clinic for ≤ 1 year. Exclusion criteria included prior hysterectomy, abnormal results prior to IS, or IS use for secondary reasons. Collected data included demographics, IBD characteristics, IBD therapy, HPV vaccination, and contraceptive use. Screening adherence was defined by the 2022 Crohn’s and Colitis Foundation Health Maintenance Checklist. Nonadherence was defined as failure to maintain annual pap cytology or cytology with HPV co-testing every three years. Wilcoxon rank sum, Fischer’s exact, and chi-squared tests evaluated differences between groups. The IR was calculated using total screening events per total person-time. The exact Poisson test compared the observed IR to the lower bound of the recommended reference rate, 33.3 per 100 person-years.
Results: We identified 195 female patients on IS. Nonadherence to cervical cancer screening occurred in 56.9% of patients. Shorter follow-up, private insurance status, non-smoking history, and intrauterine device use were significantly associated with adherence (Table 1). The IR for cervical cancer screening was 24.3 per 100 person-years (p = 0.0003, 95% CI 0.238, 0.302).
Discussion: Females with IBD on IS at a tertiary academic center undergo cervical cancer screening significantly less frequently than recommended. Future analyses will assess incidence rates in a diverse population, rates of abnormal screening outcomes, and adjusted predictors of nonadherence using multivariable regression.
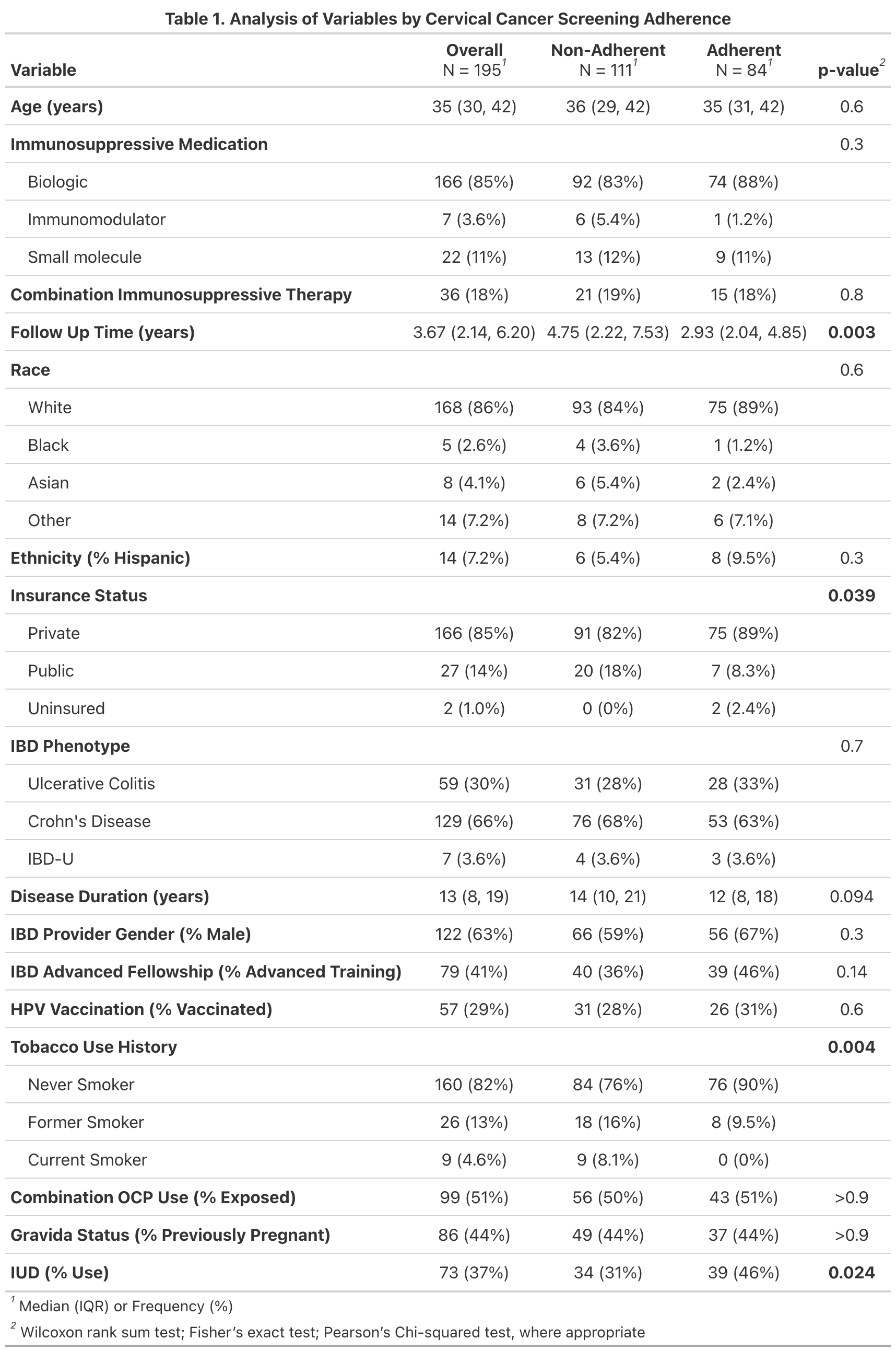
Figure: Table 1. Analysis of Variables by Cervical Cancer Screening Adherence
Disclosures:
Taylor Karl indicated no relevant financial relationships.
Nancy Wu indicated no relevant financial relationships.
Frank Scott indicated no relevant financial relationships.
Taylor A. Karl, MD1, Nancy Wu, MD, PhD2, Frank I. Scott, MD, MSCE3. P5416 - Cervical Cancer Screening Rates Among Females With Inflammatory Bowel Disease Receiving Immunosuppressive Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
