Tuesday Poster Session
Category: IBD
P5506 - Pulmonary Granulomas in Crohn’s Disease: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GS
Gurwinder Sidhu, MD (he/him/his)
UBC Department of Medicine
Vancouver, BC, Canada
Presenting Author(s)
Bachviet AH. Nguyen, MD1, Gurwinder Sidhu, MD2, Astrid-Jane Williams, MD3, Gregory Rosenfeld, MD, MHSc3
1University of British Columbia Department of Medicine, Surrey, BC, Canada; 2UBC Department of Medicine, Vancouver, BC, Canada; 3UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction: Granulomas are inflammatory lesions consisting of an organized collection of macrophages and other immune cells, associated with infection or autoimmune conditions. Crohn’s disease (CD) is an autoimmune condition characterized by patchy areas of transmural inflammation occurring throughout the gastrointestinal tract with numerous extraintestinal manifestations (EIM), the most common being arthritis, erythema nodosum, and uveitis.
We describe a rare case of multiple pulmonary granulomas secondary to active CD.
Case Description/
Methods: A 38 year old female with a 3 pack-year history of smoking and ileocolonic CD diagnosed at age 24 not on therapy presented with left shoulder pain and chronic cough.
A chest CT with IV contrast was performed which demonstrated >10 bilateral nodular/mass-like spiculated pulmonary lesions affecting all lobes with minimal peripheral ground-glass opacities. The largest such lesion was localized subpleurally at the posterior left base, measuring 4.3 cm.
A biopsy showed a non-caseating granuloma with negative elastic fiber changes, negative bacterial and fungal stains/smears, and no evidence of malignancy. Mantoux test and ANA were negative, and CRP was 56.6. She was treated with antibiotics and improved but her pulmonary symptoms recurred after 6 months concurrent with a flare of her CD (calprotectin 1260). A repeat chest CT showed mild centrilobular emphysema, mild bronchiectasis, and 3 new lesions in the right lower lobe without significant adenopathy. A bronchoscopy of the right lower lobe was unremarkable with normal eosinophils. On a review of her previous biopsy, the consensus was that this was pulmonary CD. She received oral prednisolone followed by symptomatic relief on twice weekly IV infliximab. She then switched to risankizumab due to infliximab-induced hepatitis which resolved her gastrointestinal and pulmonary symptoms. At 3 years of follow-up, fecal calprotectin was 36 and repeat chest CT demonstrated resolution of most pulmonary nodules.
Discussion: A pulmonary EIM should be considered in a patient with CD and lung granulomas but can initially be mistaken for an infectious process. Once pulmonary CD is confirmed, the patient should also be investigated for a concurrent flare of their CD as literature review indicates that pulmonary manifestations are not always congruent with luminal disease activity. Steroids and biologics are used to manage CD-associated pulmonary granulomas.
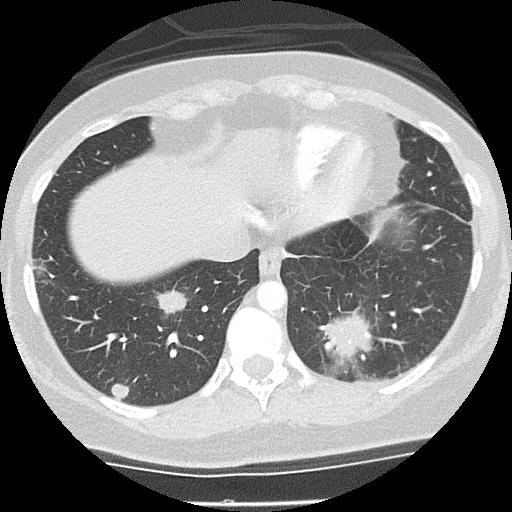
Figure: Figure 1: The initial chest CT with IV contrast demonstrating >10 bilateral nodular/mass-like spiculated pulmonary lesions affecting all lobes. These were relatively circumscribed, with spiculated margins for most, and minimal peripheral ground-glass opacities. The largest such lesion was localized subpleurally at the posterior left base, measuring 4.3 cm. Additionally, several mildly prominent hilar and perihilar lymph nodes of up to 1 cm short axis were present bilaterally.
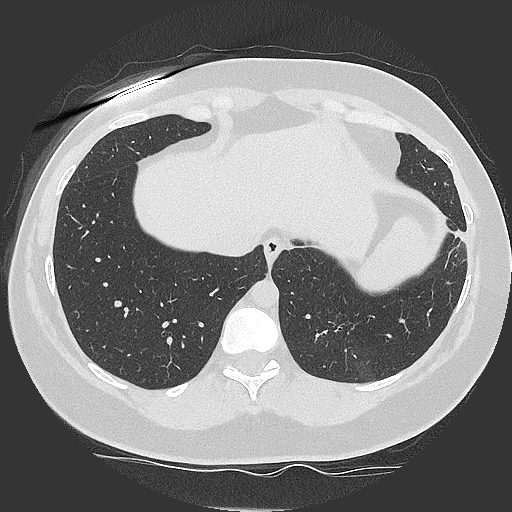
Figure: Figure 2: A repeat chest CT with IV contrast demonstrating resolution of most of the pulmonary nodules, although ground-glass changes were present in the LLL and RUL that likely represented chronic scarring.
Disclosures:
Bachviet Nguyen indicated no relevant financial relationships.
Gurwinder Sidhu indicated no relevant financial relationships.
Astrid-Jane Williams indicated no relevant financial relationships.
Gregory Rosenfeld indicated no relevant financial relationships.
Bachviet AH. Nguyen, MD1, Gurwinder Sidhu, MD2, Astrid-Jane Williams, MD3, Gregory Rosenfeld, MD, MHSc3. P5506 - Pulmonary Granulomas in Crohn’s Disease: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of British Columbia Department of Medicine, Surrey, BC, Canada; 2UBC Department of Medicine, Vancouver, BC, Canada; 3UBC Department of Medicine/IBD Centre of BC, Vancouver, BC, Canada
Introduction: Granulomas are inflammatory lesions consisting of an organized collection of macrophages and other immune cells, associated with infection or autoimmune conditions. Crohn’s disease (CD) is an autoimmune condition characterized by patchy areas of transmural inflammation occurring throughout the gastrointestinal tract with numerous extraintestinal manifestations (EIM), the most common being arthritis, erythema nodosum, and uveitis.
We describe a rare case of multiple pulmonary granulomas secondary to active CD.
Case Description/
Methods: A 38 year old female with a 3 pack-year history of smoking and ileocolonic CD diagnosed at age 24 not on therapy presented with left shoulder pain and chronic cough.
A chest CT with IV contrast was performed which demonstrated >10 bilateral nodular/mass-like spiculated pulmonary lesions affecting all lobes with minimal peripheral ground-glass opacities. The largest such lesion was localized subpleurally at the posterior left base, measuring 4.3 cm.
A biopsy showed a non-caseating granuloma with negative elastic fiber changes, negative bacterial and fungal stains/smears, and no evidence of malignancy. Mantoux test and ANA were negative, and CRP was 56.6. She was treated with antibiotics and improved but her pulmonary symptoms recurred after 6 months concurrent with a flare of her CD (calprotectin 1260). A repeat chest CT showed mild centrilobular emphysema, mild bronchiectasis, and 3 new lesions in the right lower lobe without significant adenopathy. A bronchoscopy of the right lower lobe was unremarkable with normal eosinophils. On a review of her previous biopsy, the consensus was that this was pulmonary CD. She received oral prednisolone followed by symptomatic relief on twice weekly IV infliximab. She then switched to risankizumab due to infliximab-induced hepatitis which resolved her gastrointestinal and pulmonary symptoms. At 3 years of follow-up, fecal calprotectin was 36 and repeat chest CT demonstrated resolution of most pulmonary nodules.
Discussion: A pulmonary EIM should be considered in a patient with CD and lung granulomas but can initially be mistaken for an infectious process. Once pulmonary CD is confirmed, the patient should also be investigated for a concurrent flare of their CD as literature review indicates that pulmonary manifestations are not always congruent with luminal disease activity. Steroids and biologics are used to manage CD-associated pulmonary granulomas.
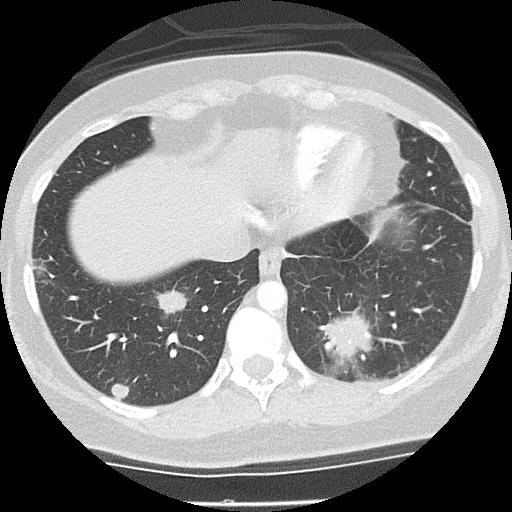
Figure: Figure 1: The initial chest CT with IV contrast demonstrating >10 bilateral nodular/mass-like spiculated pulmonary lesions affecting all lobes. These were relatively circumscribed, with spiculated margins for most, and minimal peripheral ground-glass opacities. The largest such lesion was localized subpleurally at the posterior left base, measuring 4.3 cm. Additionally, several mildly prominent hilar and perihilar lymph nodes of up to 1 cm short axis were present bilaterally.
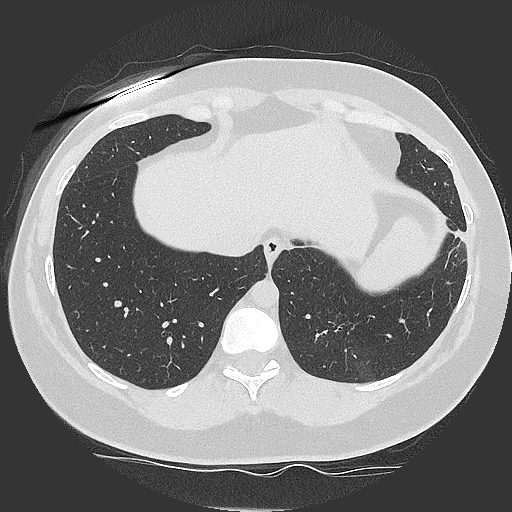
Figure: Figure 2: A repeat chest CT with IV contrast demonstrating resolution of most of the pulmonary nodules, although ground-glass changes were present in the LLL and RUL that likely represented chronic scarring.
Disclosures:
Bachviet Nguyen indicated no relevant financial relationships.
Gurwinder Sidhu indicated no relevant financial relationships.
Astrid-Jane Williams indicated no relevant financial relationships.
Gregory Rosenfeld indicated no relevant financial relationships.
Bachviet AH. Nguyen, MD1, Gurwinder Sidhu, MD2, Astrid-Jane Williams, MD3, Gregory Rosenfeld, MD, MHSc3. P5506 - Pulmonary Granulomas in Crohn’s Disease: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
