Tuesday Poster Session
Category: IBD
P5489 - Meta-Analysis and Systematic Reviews: Bowel Preparation With Polyethylene Glycol vs Non-Polyethylene Glycol in IBD Patients
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- PB
Prajjwol D. Bhatta, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Prajjwol D. Bhatta, MD1, Smriti D. Bhetuwal, RN1, John Shrestha, MBBS2, Nathan P. Heller, MD1, Tausif Syed, MD1, Mahesh Nepal, MD1, Ahmed Shehadah, MD3, Hamza Akhtar, MD1
1Rochester General Hospital, Rochester, NY; 2Rochester General hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Inadequate bowel preparation increases the chances of missing small or large polyps, decreases cecal intubation rate, prolongs colonoscopy time, and may lead to cancellation or rescheduling of the procedure. Inflammatory bowel disease (IBD) patients require colonoscopy from the beginning to aid in diagnosis, monitor disease activity, evaluate treatment response and allow frequent surveillance for colon cancer. IBD patients experiences the highest embarrassment, pain and lowest satisfaction score. Most guidelines recommend the use of PEG solutions over non-PEG in IBD patients which limits the overall acceptance of non-PEG solutions. However, the use of non-PEG solutions as per disease severity is now being considered. Therefore, the primary aim of this systematic review and meta-analysis is to assess if non-PEG solutions are equally efficacious as PEG solutions in IBD patients.
Methods: Multiple databases were searched through June 2024 for studies comparing PEG vs non-PEG in IBD patients. The primary outcome of our study was successful bowel preparation if Boston Bowel Preparation Scale (BBPS) of ≥6, Ottawa Bowel Preparation Score of ≤5, Harefield Cleansing Scale [HCS] ≥A or B. Secondary outcome was willingness to repeat. Meta-analysis was performed to determine the pooled risk ratio (RR) using random effects model.
Results: Four randomized controlled trials involving a total of 479 participants were included in the final analysis. 254 participants received PEG whereas 225 participants received non-PEG. Random-effects meta-analysis of four RCTs showed no significant difference in bowel preparation success between PEG and non-PEG regimens (RR=1.01, 95% CI 0.88–1.16, I²=0%). Three RCTs (n=384) found no significant difference in willingness to repeat bowel preparation between PEG and non-PEG regimens (RR = 0.92, 95% CI 0.78–1.08, I² = 0%).
Discussion: Our findings suggest that there is no significant difference in bowel preparation success (RR=1.01) or willingness to repeat (RR=0.92) between PEG and non-PEG regimens in IBD patients. The findings suggest that non-PEG regimens may be considered suitable alternatives to PEG, especially in patients who struggle with PEG due to volume or taste. The low heterogeneity in both primary and secondary outcomes strengthens our confidence in the findings. However, given the limited number of studies and small sample sizes, further large-scale trials are needed to confirm the safety and efficacy of non-PEG preparations in different IBD subgroups.
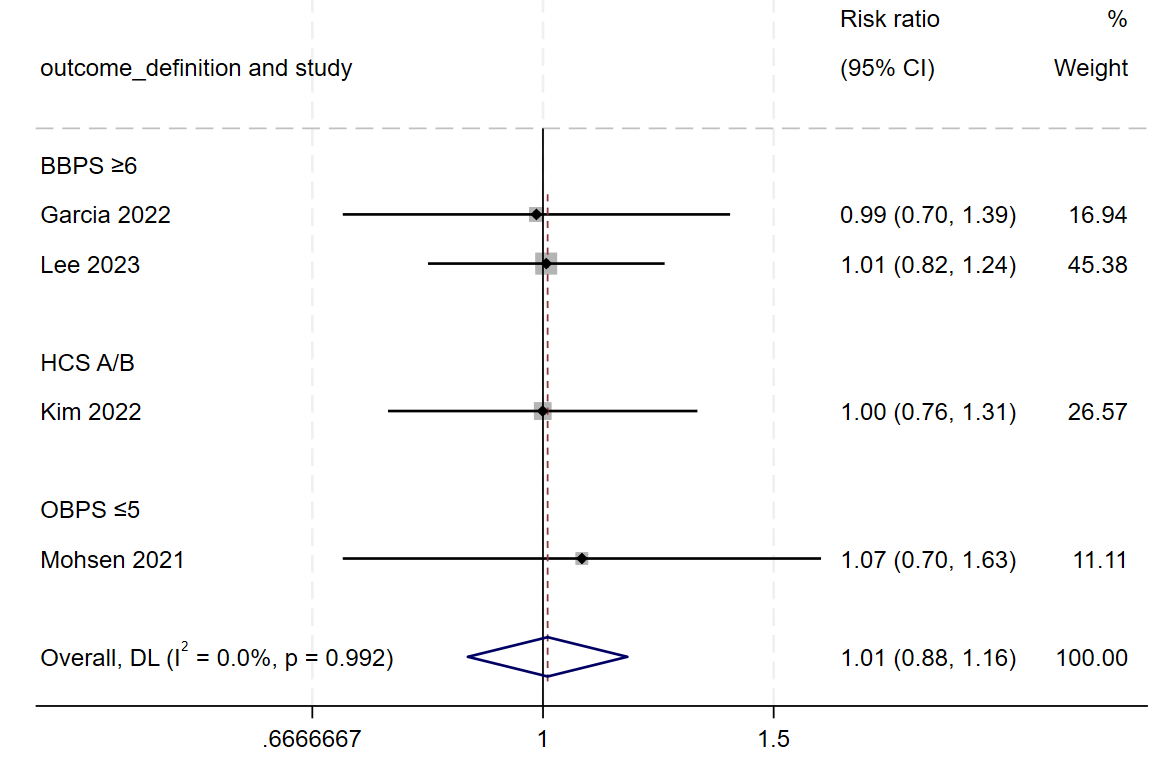
Figure: Figure1: Forest plot of successful bowel preparation in IBD patients comparing PEG vs. non-PEG regimens.
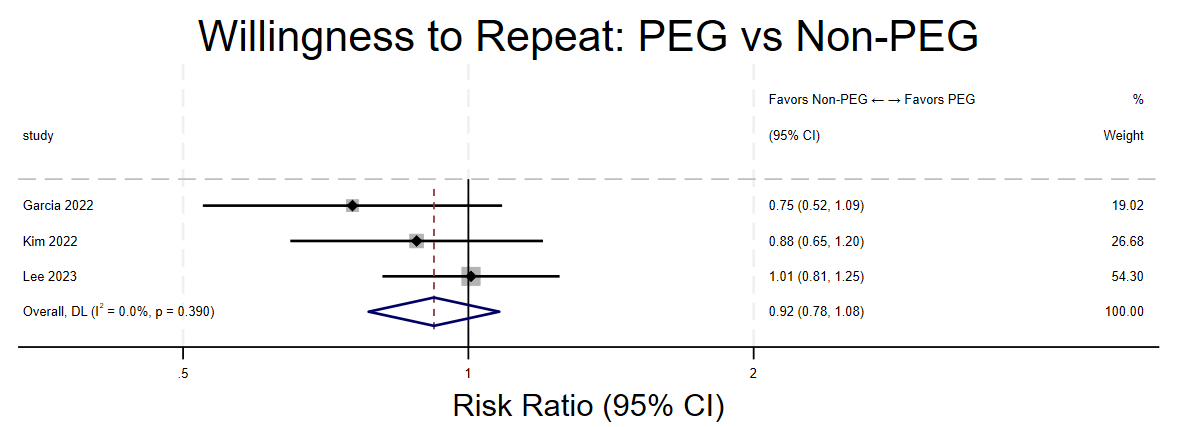
Figure: Figure2: Forest plot comparing willingness to repeat PEG vs. non-PEG
Disclosures:
Prajjwol Bhatta indicated no relevant financial relationships.
Smriti Bhetuwal indicated no relevant financial relationships.
John Shrestha indicated no relevant financial relationships.
Nathan Heller indicated no relevant financial relationships.
Tausif Syed indicated no relevant financial relationships.
Mahesh Nepal indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Hamza Akhtar indicated no relevant financial relationships.
Prajjwol D. Bhatta, MD1, Smriti D. Bhetuwal, RN1, John Shrestha, MBBS2, Nathan P. Heller, MD1, Tausif Syed, MD1, Mahesh Nepal, MD1, Ahmed Shehadah, MD3, Hamza Akhtar, MD1. P5489 - Meta-Analysis and Systematic Reviews: Bowel Preparation With Polyethylene Glycol vs Non-Polyethylene Glycol in IBD Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Rochester General hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Binghamton, NY
Introduction: Inadequate bowel preparation increases the chances of missing small or large polyps, decreases cecal intubation rate, prolongs colonoscopy time, and may lead to cancellation or rescheduling of the procedure. Inflammatory bowel disease (IBD) patients require colonoscopy from the beginning to aid in diagnosis, monitor disease activity, evaluate treatment response and allow frequent surveillance for colon cancer. IBD patients experiences the highest embarrassment, pain and lowest satisfaction score. Most guidelines recommend the use of PEG solutions over non-PEG in IBD patients which limits the overall acceptance of non-PEG solutions. However, the use of non-PEG solutions as per disease severity is now being considered. Therefore, the primary aim of this systematic review and meta-analysis is to assess if non-PEG solutions are equally efficacious as PEG solutions in IBD patients.
Methods: Multiple databases were searched through June 2024 for studies comparing PEG vs non-PEG in IBD patients. The primary outcome of our study was successful bowel preparation if Boston Bowel Preparation Scale (BBPS) of ≥6, Ottawa Bowel Preparation Score of ≤5, Harefield Cleansing Scale [HCS] ≥A or B. Secondary outcome was willingness to repeat. Meta-analysis was performed to determine the pooled risk ratio (RR) using random effects model.
Results: Four randomized controlled trials involving a total of 479 participants were included in the final analysis. 254 participants received PEG whereas 225 participants received non-PEG. Random-effects meta-analysis of four RCTs showed no significant difference in bowel preparation success between PEG and non-PEG regimens (RR=1.01, 95% CI 0.88–1.16, I²=0%). Three RCTs (n=384) found no significant difference in willingness to repeat bowel preparation between PEG and non-PEG regimens (RR = 0.92, 95% CI 0.78–1.08, I² = 0%).
Discussion: Our findings suggest that there is no significant difference in bowel preparation success (RR=1.01) or willingness to repeat (RR=0.92) between PEG and non-PEG regimens in IBD patients. The findings suggest that non-PEG regimens may be considered suitable alternatives to PEG, especially in patients who struggle with PEG due to volume or taste. The low heterogeneity in both primary and secondary outcomes strengthens our confidence in the findings. However, given the limited number of studies and small sample sizes, further large-scale trials are needed to confirm the safety and efficacy of non-PEG preparations in different IBD subgroups.
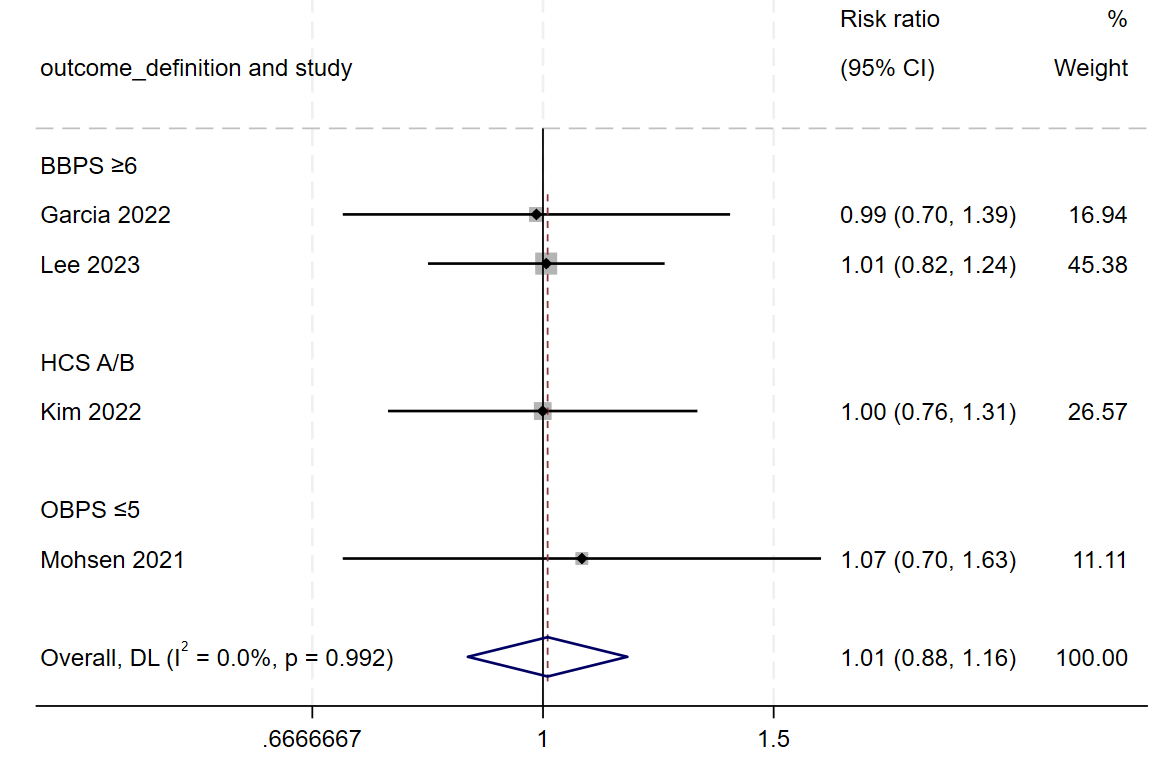
Figure: Figure1: Forest plot of successful bowel preparation in IBD patients comparing PEG vs. non-PEG regimens.
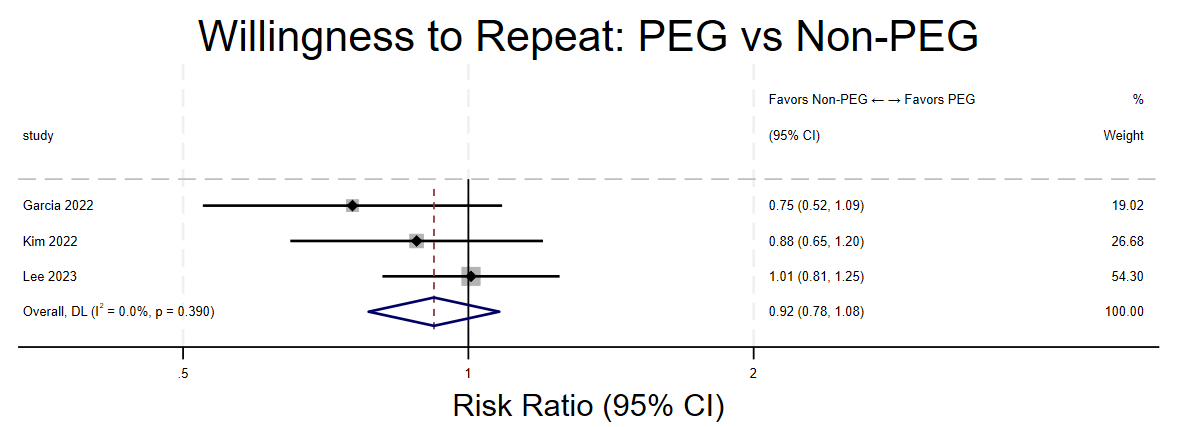
Figure: Figure2: Forest plot comparing willingness to repeat PEG vs. non-PEG
Disclosures:
Prajjwol Bhatta indicated no relevant financial relationships.
Smriti Bhetuwal indicated no relevant financial relationships.
John Shrestha indicated no relevant financial relationships.
Nathan Heller indicated no relevant financial relationships.
Tausif Syed indicated no relevant financial relationships.
Mahesh Nepal indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Hamza Akhtar indicated no relevant financial relationships.
Prajjwol D. Bhatta, MD1, Smriti D. Bhetuwal, RN1, John Shrestha, MBBS2, Nathan P. Heller, MD1, Tausif Syed, MD1, Mahesh Nepal, MD1, Ahmed Shehadah, MD3, Hamza Akhtar, MD1. P5489 - Meta-Analysis and Systematic Reviews: Bowel Preparation With Polyethylene Glycol vs Non-Polyethylene Glycol in IBD Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
