Tuesday Poster Session
Category: Infections and Microbiome
P5577 - Explosive Rise in Alpha-Gal Syndrome: A Real-World Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- VJ
Vinay Jahagirdar, MD
Virginia Commonwealth University Medical Center
Richmond, VA
Presenting Author(s)
Kaanthi Rama, MD1, Vinay Jahagirdar, MD2, Prabhat Kumar, MD1, Raseen Tariq, MD1, Stephen J. Bickston, MD, FACG1, Ravi Vachhani, MD1
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA
Introduction: Alpha-gal syndrome (AGS) is an IgE-mediated allergy to galactose-α-1,3-galactose, a carbohydrate found in mammalian meat, with sensitization linked to tick bites—particularly the Lone Star tick in the U.S. AGS is unique due to delayed-onset symptoms and frequent gastrointestinal (GI) manifestations such as abdominal pain, diarrhea, and nausea. Despite rising recognition, population-level demographic and clinical features remain poorly characterized.
Methods: This retrospective observational study used the TriNetX US Collaborative Network to identify adults with alpha-gal specific IgE ≥0.1 kU/L from 2010 to 2025. The study was IRB-exempt. Demographics, diagnosis codes, and medication usage prior to or on the date of testing were extracted. Geographic distribution was based on the location of the healthcare organization headquarters. Incidence proportion was defined as the number of patients newly meeting the event definition (positive IgE) in each 2-year window (numerator), divided by patients whose records overlapped the window, had no prior alpha-gal sensitization, and met cohort criteria (denominator). Incidence rates (cases/100 patient-years) were then calculated by dividing incidence proportion by the window duration and multiplying by 100.
Results: Among 3,828 patients tested for alpha-gal IgE, 749 (23%) were positive (Fig. A). Median age was 63 years (IQR 52–72); 48% were female, 78% White. Most patients were in the Northeast (69%) or South (23%) (Fig. B). Median BMI was 26 (IQR 23–29). Common comorbidities included joint disorders (76%), hyperlipidemia (60%), food allergy (59%), vitamin D deficiency (39%), asthma (27%), and Lyme disease (17%). Frequent medications: albuterol (30%), cetirizine (29%), diphenhydramine (21%), pantoprazole (22%). Incidence proportion rose from 1.8% (2013–2014) to 14.2% (2019–2020), 38% (2021–2022), and 100% (2023–2024). Corresponding incidence rates increased from 0.95 (2013-2014) to 94.55 cases/100 PY (2023-2024) (Fig. C).
Discussion: This is the largest real-world AGS cohort to date, showing regional clustering and characteristic comorbidity patterns. The 100-fold rise in incidence rates among those who tested positive from 2013 to 2024 reflects increased clinical recognition and testing. AGS should be considered in patients with unexplained abdominal pain or diarrhea, especially in endemic areas. Awareness among gastroenterologists is essential for timely diagnosis and management.
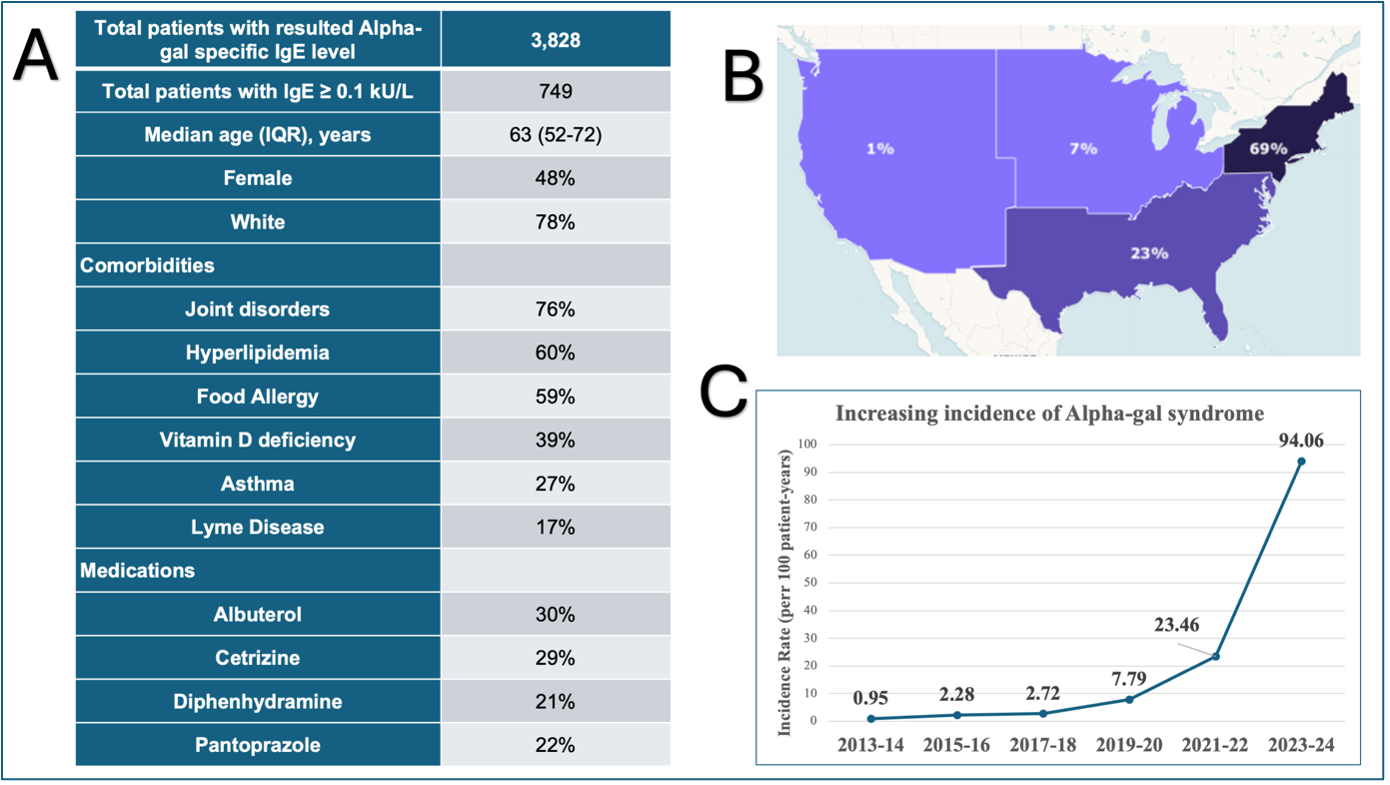
Figure: Figure: Demographic, clinical, geographic, and temporal characteristics of patients with alpha-gal syndrome (AGS). (A) Summary of patient demographics, comorbidities, and commonly prescribed medications among 749 individuals with alpha-gal specific IgE ≥ 0.1 kU/L identified from a cohort of 3,828 tested patients. (B) Geographic distribution of AGS cases by U.S. region, with the majority residing in the Northeast (69%) and South (23%). (C) Temporal trend in incidence rate of AGS, showing a marked increase from 0.95 to 94.6 cases per 100 patient-years between 2013 and 2024.
Disclosures:
Kaanthi Rama indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Raseen Tariq indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Ravi Vachhani indicated no relevant financial relationships.
Kaanthi Rama, MD1, Vinay Jahagirdar, MD2, Prabhat Kumar, MD1, Raseen Tariq, MD1, Stephen J. Bickston, MD, FACG1, Ravi Vachhani, MD1. P5577 - Explosive Rise in Alpha-Gal Syndrome: A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Richmond, VA; 2Virginia Commonwealth University Medical Center, Richmond, VA
Introduction: Alpha-gal syndrome (AGS) is an IgE-mediated allergy to galactose-α-1,3-galactose, a carbohydrate found in mammalian meat, with sensitization linked to tick bites—particularly the Lone Star tick in the U.S. AGS is unique due to delayed-onset symptoms and frequent gastrointestinal (GI) manifestations such as abdominal pain, diarrhea, and nausea. Despite rising recognition, population-level demographic and clinical features remain poorly characterized.
Methods: This retrospective observational study used the TriNetX US Collaborative Network to identify adults with alpha-gal specific IgE ≥0.1 kU/L from 2010 to 2025. The study was IRB-exempt. Demographics, diagnosis codes, and medication usage prior to or on the date of testing were extracted. Geographic distribution was based on the location of the healthcare organization headquarters. Incidence proportion was defined as the number of patients newly meeting the event definition (positive IgE) in each 2-year window (numerator), divided by patients whose records overlapped the window, had no prior alpha-gal sensitization, and met cohort criteria (denominator). Incidence rates (cases/100 patient-years) were then calculated by dividing incidence proportion by the window duration and multiplying by 100.
Results: Among 3,828 patients tested for alpha-gal IgE, 749 (23%) were positive (Fig. A). Median age was 63 years (IQR 52–72); 48% were female, 78% White. Most patients were in the Northeast (69%) or South (23%) (Fig. B). Median BMI was 26 (IQR 23–29). Common comorbidities included joint disorders (76%), hyperlipidemia (60%), food allergy (59%), vitamin D deficiency (39%), asthma (27%), and Lyme disease (17%). Frequent medications: albuterol (30%), cetirizine (29%), diphenhydramine (21%), pantoprazole (22%). Incidence proportion rose from 1.8% (2013–2014) to 14.2% (2019–2020), 38% (2021–2022), and 100% (2023–2024). Corresponding incidence rates increased from 0.95 (2013-2014) to 94.55 cases/100 PY (2023-2024) (Fig. C).
Discussion: This is the largest real-world AGS cohort to date, showing regional clustering and characteristic comorbidity patterns. The 100-fold rise in incidence rates among those who tested positive from 2013 to 2024 reflects increased clinical recognition and testing. AGS should be considered in patients with unexplained abdominal pain or diarrhea, especially in endemic areas. Awareness among gastroenterologists is essential for timely diagnosis and management.
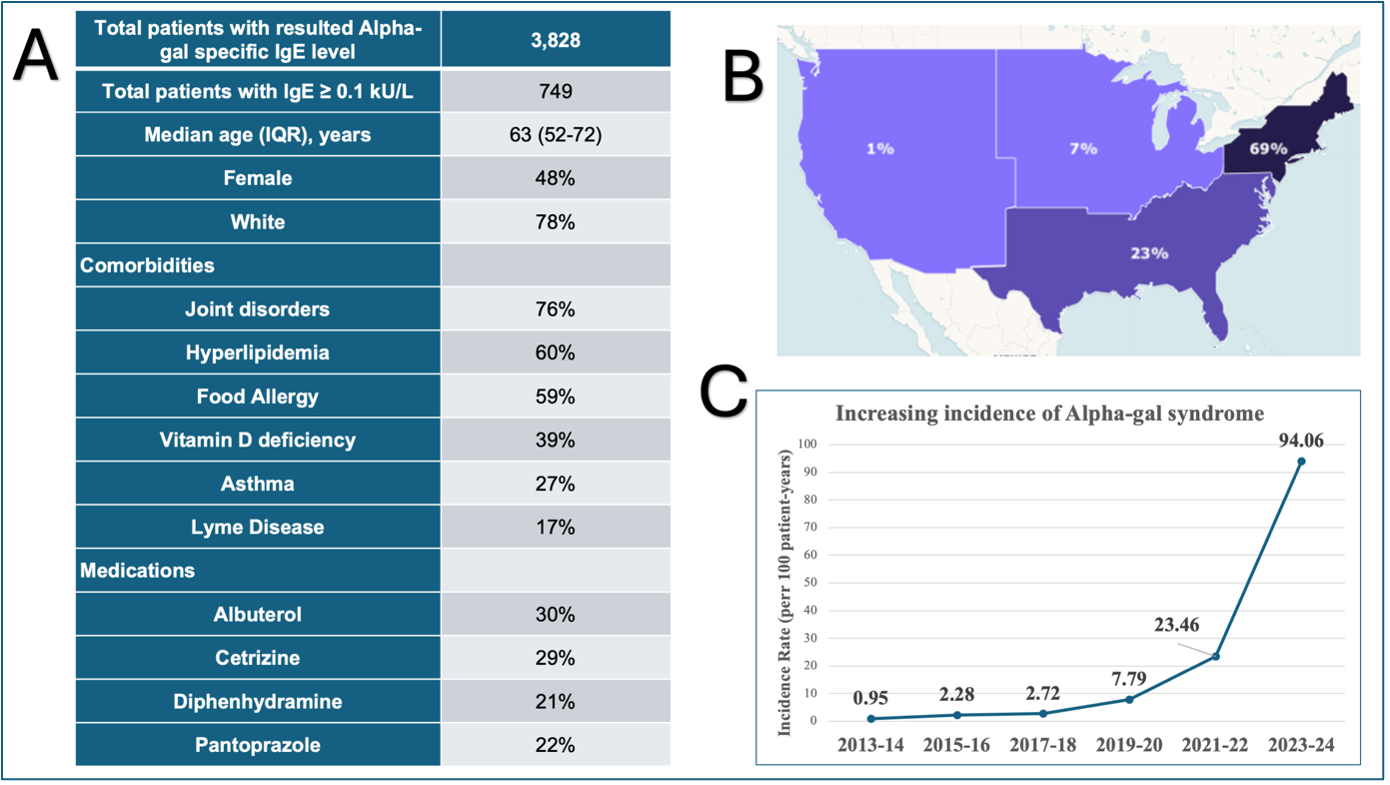
Figure: Figure: Demographic, clinical, geographic, and temporal characteristics of patients with alpha-gal syndrome (AGS). (A) Summary of patient demographics, comorbidities, and commonly prescribed medications among 749 individuals with alpha-gal specific IgE ≥ 0.1 kU/L identified from a cohort of 3,828 tested patients. (B) Geographic distribution of AGS cases by U.S. region, with the majority residing in the Northeast (69%) and South (23%). (C) Temporal trend in incidence rate of AGS, showing a marked increase from 0.95 to 94.6 cases per 100 patient-years between 2013 and 2024.
Disclosures:
Kaanthi Rama indicated no relevant financial relationships.
Vinay Jahagirdar indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Raseen Tariq indicated no relevant financial relationships.
Stephen Bickston indicated no relevant financial relationships.
Ravi Vachhani indicated no relevant financial relationships.
Kaanthi Rama, MD1, Vinay Jahagirdar, MD2, Prabhat Kumar, MD1, Raseen Tariq, MD1, Stephen J. Bickston, MD, FACG1, Ravi Vachhani, MD1. P5577 - Explosive Rise in Alpha-Gal Syndrome: A Real-World Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
