Tuesday Poster Session
Category: Interventional Endoscopy
P5675 - Comparative Outcomes of Deep Sedation and General Anesthesia in Therapeutic Endoscopy With Complexity Stratification
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HP
Harsh Patel, MD
NewYork-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Harsh Patel, MD1, Kin Li, MD2, Muhammad Bouso, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Arshish Dua, MD2
1NewYork-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Procedural complexity regarding EUS (endoscopic ultrasound) and ERCP (endoscopic retrograde cholangiopancreatography) continues to increase in the modern age. Appropriate anesthesia administration is imperative for technical success and procedural safety. Limited societal guidance currently exists concerning anesthesia choice specific to procedural complexity with high variation in anesthesia protocols between institutions. This retrospective study assessed safety, efficacy, procedural complexity, and related outcomes concerning the administration of deep sedation (monitored anesthesia care) and general anesthesia in advanced therapeutic procedures at a tertiary academic center.
Methods: A retrospective review of 982 procedural encounters who underwent EUS and/or ERCP from 2022-2024 was conducted (Figure 1). Procedural stratifications by type and complexity, as well as baseline demographics were obtained. Anesthetic risk assessments and scores were additionally recorded. Logistic regression analysis evaluating outcomes was conducted for anesthesia administered, procedural type, and complexity with risk associations described up to 60 days post-procedure
Results: No significant difference in baseline demographics was noted other than higher ASA scores in general anesthesia procedures as well as the general anesthesia ERCP subset compared to deep sedation ((3.05 vs 2.83, p < 0.01); (3.01 vs 2.87, p< 0.00032)). Endoscopists reported adverse events were lower in the deep sedation group when compared with general anesthesia (0.8% vs 4.0% p< 0.01). Anesthesia reported adverse events were not significant between groups (0% vs 1.2%, OR 0.0093, p value 0.99), although no events were noted in the general anesthesia group. Completion of the intended procedure was higher in deep sedation groups (98.3% vs 94.9%, OR 3.03, p = 0.011). Successful biliary access, anesthesia-related hospital readmission, and procedural-related hospital admission were not significant between groups
Discussion: Deep sedation is associated with fewer endoscopist-reported and similar anesthesia-reported adverse events when compared with general anesthesia. Completion of the intended procedure was higher with deep sedation however no differences were noted in successful biliary access. ASGE complexity and ASA score appear to be higher in patients undergoing general anesthesia. Further prospective analysis is required to fully delineate these associations to aid in anesthesia selection concerning advanced endoscopic procedures
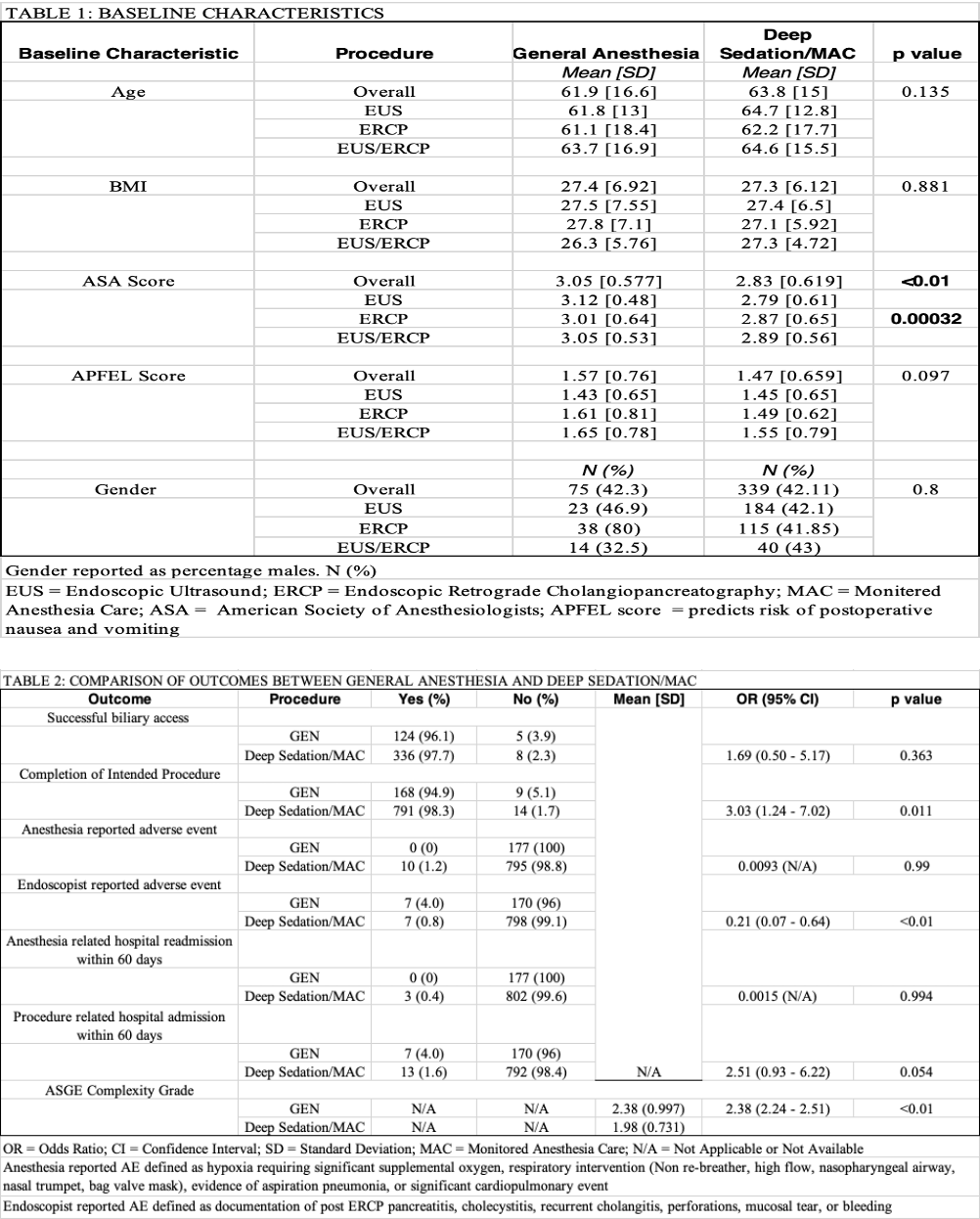
Figure: Figure 1: Flowsheet of included procedural encounters subdivided based on anesthesia type and procedures performed
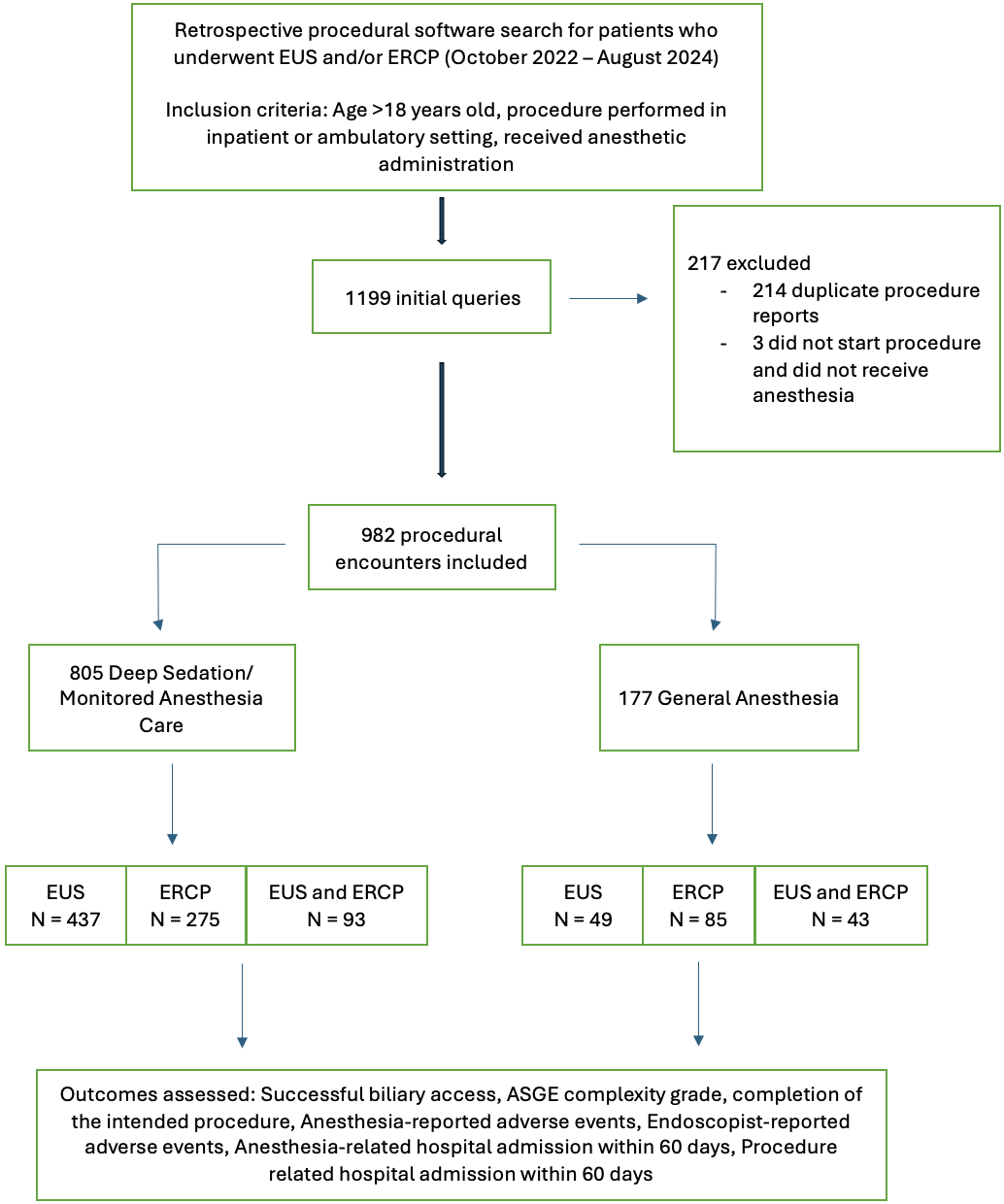
Figure: Figure 2: Baseline characteristics and outcomes
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Kin Li indicated no relevant financial relationships.
Muhammad Bouso indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Karthik Chandrasekaran indicated no relevant financial relationships.
Arshish Dua indicated no relevant financial relationships.
Harsh Patel, MD1, Kin Li, MD2, Muhammad Bouso, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Arshish Dua, MD2. P5675 - Comparative Outcomes of Deep Sedation and General Anesthesia in Therapeutic Endoscopy With Complexity Stratification, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Procedural complexity regarding EUS (endoscopic ultrasound) and ERCP (endoscopic retrograde cholangiopancreatography) continues to increase in the modern age. Appropriate anesthesia administration is imperative for technical success and procedural safety. Limited societal guidance currently exists concerning anesthesia choice specific to procedural complexity with high variation in anesthesia protocols between institutions. This retrospective study assessed safety, efficacy, procedural complexity, and related outcomes concerning the administration of deep sedation (monitored anesthesia care) and general anesthesia in advanced therapeutic procedures at a tertiary academic center.
Methods: A retrospective review of 982 procedural encounters who underwent EUS and/or ERCP from 2022-2024 was conducted (Figure 1). Procedural stratifications by type and complexity, as well as baseline demographics were obtained. Anesthetic risk assessments and scores were additionally recorded. Logistic regression analysis evaluating outcomes was conducted for anesthesia administered, procedural type, and complexity with risk associations described up to 60 days post-procedure
Results: No significant difference in baseline demographics was noted other than higher ASA scores in general anesthesia procedures as well as the general anesthesia ERCP subset compared to deep sedation ((3.05 vs 2.83, p < 0.01); (3.01 vs 2.87, p< 0.00032)). Endoscopists reported adverse events were lower in the deep sedation group when compared with general anesthesia (0.8% vs 4.0% p< 0.01). Anesthesia reported adverse events were not significant between groups (0% vs 1.2%, OR 0.0093, p value 0.99), although no events were noted in the general anesthesia group. Completion of the intended procedure was higher in deep sedation groups (98.3% vs 94.9%, OR 3.03, p = 0.011). Successful biliary access, anesthesia-related hospital readmission, and procedural-related hospital admission were not significant between groups
Discussion: Deep sedation is associated with fewer endoscopist-reported and similar anesthesia-reported adverse events when compared with general anesthesia. Completion of the intended procedure was higher with deep sedation however no differences were noted in successful biliary access. ASGE complexity and ASA score appear to be higher in patients undergoing general anesthesia. Further prospective analysis is required to fully delineate these associations to aid in anesthesia selection concerning advanced endoscopic procedures
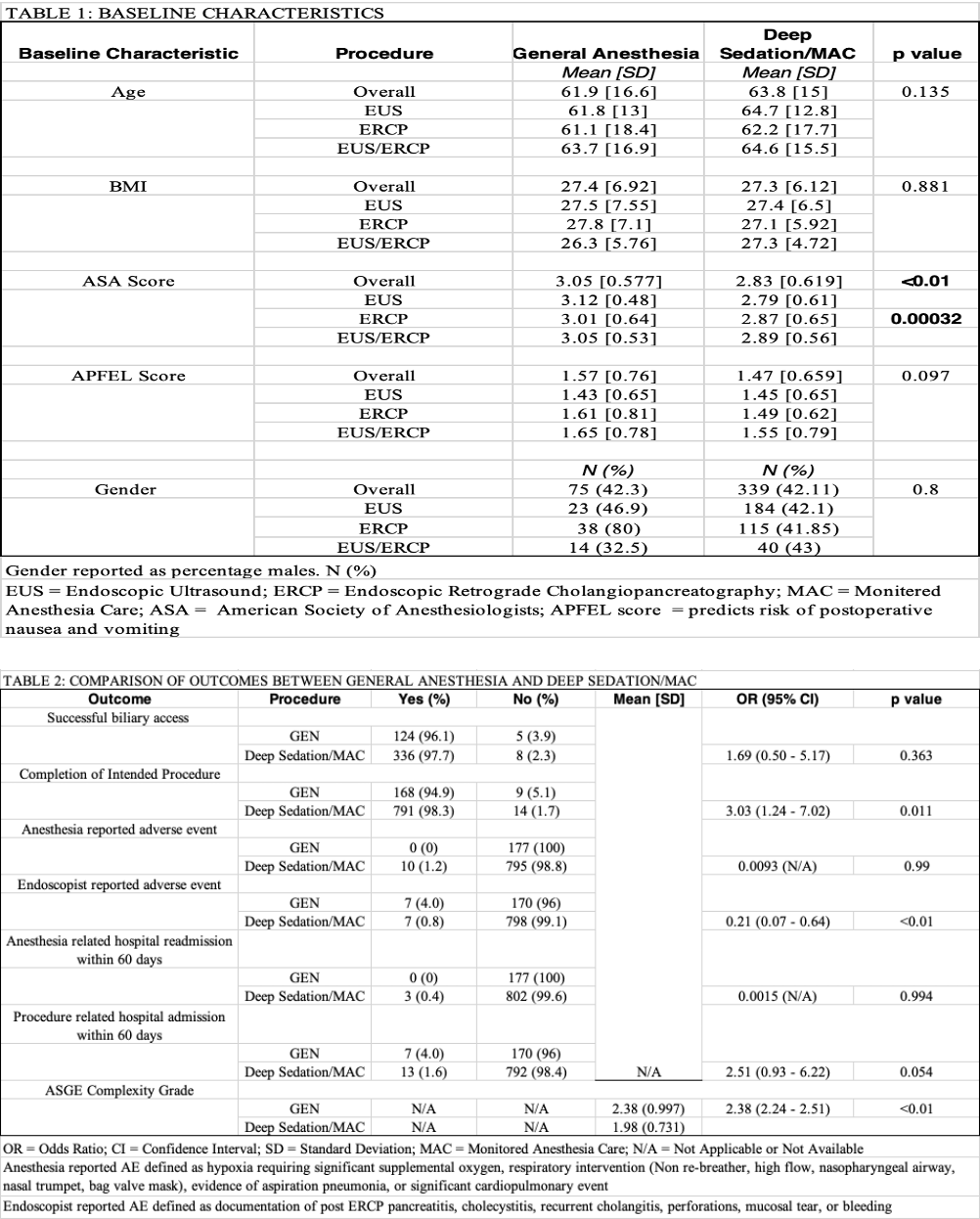
Figure: Figure 1: Flowsheet of included procedural encounters subdivided based on anesthesia type and procedures performed
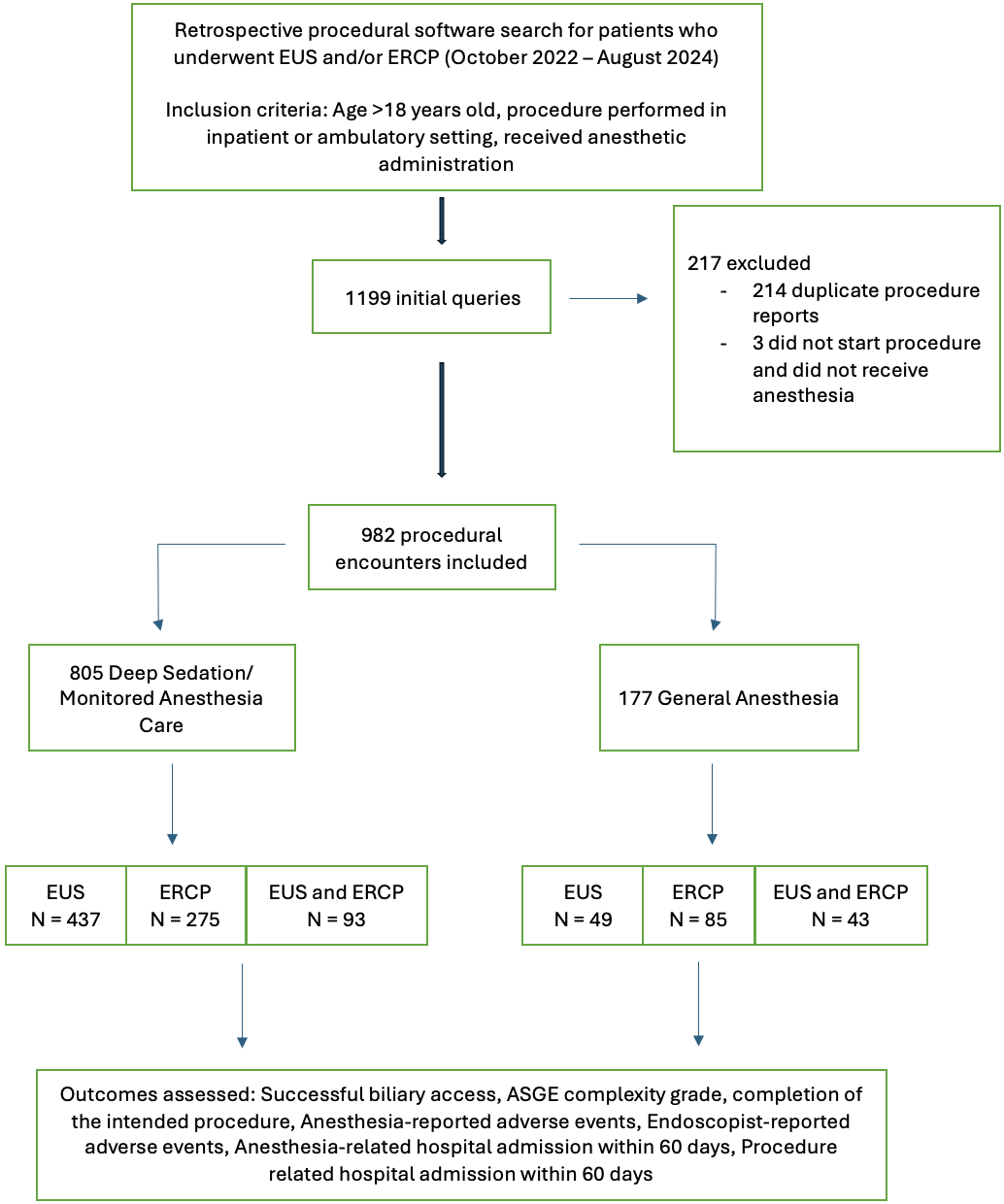
Figure: Figure 2: Baseline characteristics and outcomes
Disclosures:
Harsh Patel indicated no relevant financial relationships.
Kin Li indicated no relevant financial relationships.
Muhammad Bouso indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Karthik Chandrasekaran indicated no relevant financial relationships.
Arshish Dua indicated no relevant financial relationships.
Harsh Patel, MD1, Kin Li, MD2, Muhammad Bouso, MD2, Anas Zaher, MD2, Karthik Chandrasekaran, MD2, Arshish Dua, MD2. P5675 - Comparative Outcomes of Deep Sedation and General Anesthesia in Therapeutic Endoscopy With Complexity Stratification, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

