Tuesday Poster Session
Category: Interventional Endoscopy
P5664 - Improvement of Obesity-Related Comorbidities After Various Bariatric Procedures: A Network Meta-Analysis of Endoscopic versus Surgical Interventions
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panisara Fangsaard, MD
Bassett Medical Center
Cooperstown, NY
Presenting Author(s)
Panisara Fangsaard, MD1, Noppachai Siranart, MD2, Patavee Pajareya, MD3, Peenaprapa Tangpradubkiat, MD3, Runchana Parnicharoende, MD4, Daniel Martin Simadibrata, MD5, Kittithat Tantitanawat, MD6
1Bassett Medical Center, Cooperstown, NY; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3King Chulalongkorn Memorial Hospital, Bangkok, Krung Thep, Thailand; 4King Chulalongkorn Memorial Hospital, Pathum Wan, Krung Thep, Thailand; 5MetroHealth Medical Center, Cleveland, OH; 6Phramongkutklao Hospital, Bangkok, Krung Thep, Thailand
Introduction: Advances in bariatric care have led to novel endoscopic and surgical techniques to enhance weight loss and reduce obesity-related comorbidities. However, comparative data on their effectiveness remain limited. This study evaluates the impact of different bariatric procedures on comorbidity management and patient outcomes
Methods: We performed a meta-analysis through January 2025, identifying comparative studies of endoscopic and surgical bariatric techniques. Primary endpoints include improvement hypertension (HTN), diabetes mellitus (DM), dyslipidemia (DLP), obstructive sleep apnea (OSA). Secondary endpoints comprised gastroesophageal reflux (GERD) improvement and incidence of de novo reflux.
Results: A total of 56 studies involving 64,520 patients were included in the analysis; RYGB 44 studies, OAGB 20, SASI 1, SADI 2, SG 42, SG+JB 2 ESG 2. For DM improvement, single anastomosis duodeno-ileal bypass with sleeve (SADI) ranked highest (P-score: 0.932), followed by SASI (0.800) and SG with jejunal bypass (SG+JB; 0.587); OAGB doubled odds of remission versus SG (OR: 2.472, 95% CI: 1.49-4.09 vs OR: 1.289, 95% CI: 1.01-1.65). OAGB also topped HTN (0.769) and DLP (0.731). For obstructive sleep apnea (OSA) improvement, OAGB led (0.681), followed by RYGB (0.605). Among surgeries, SG consistently demonstrated the lowest effectiveness across all outcomes. Compared to surgeries, ESG excelled in HTN control, ranking second only to OAGB (P-score 0.694 vs 0.769) but had minimal effects in diabetes remission and DLP improvement (ESG P-score 0.063, well below OAGB, SASI, RYGB and even SG (0.275)). For GERD improvement, single-anastomosis ileal bypass (SASI) ranked highest (P-score: 0.900), followed by one-anastomosis gastric bypass (OAGB; 0.699) and Roux-en-Y gastric bypass (RYGB; 0.563). Both OAGB and RYGB significantly outperformed sleeve gastrectomy (SG) with odds ratios (OR) of 5.48 (95% CI: 1.52-19.76) and 3.82 (95% CI: 2.09–6.98), respectively. SASI showed the lowest incidence of de novo GERD (P-score: 0.803), while endoscopic sleeve gastroplasty (ESG) and RYGB had significantly lower rates than SG (OR: 0.08, 95% CI: 0.01–0.72 and OR: 0.29, 95% CI: 0.18–0.48, respectively).
Discussion: Novel endoscopic (ESG) and surgical (OAGB, SASI, SADI) approaches offer superior relief of obesity-related comorbidities and GERD, with lower rates of de novo reflux than sleeve gastrectomy, and their minimally invasive profiles support their use as first-line treatments.
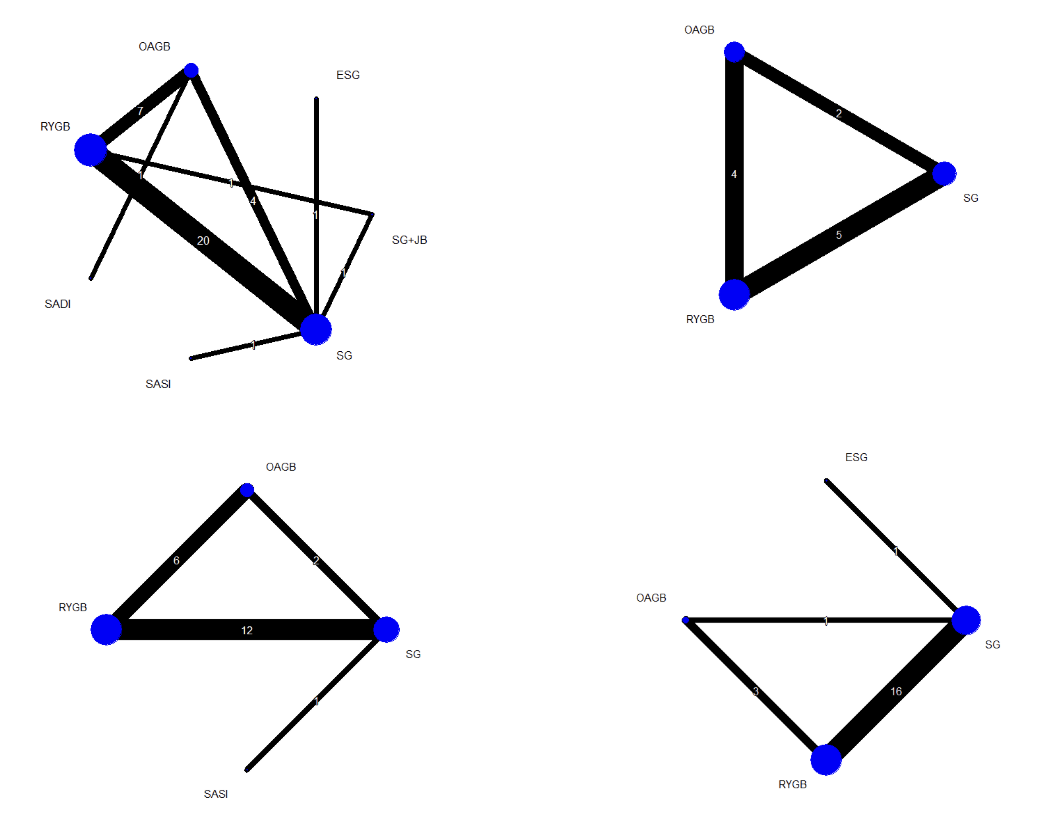
Figure: Figure 1. Primary endpoints include improvement hypertension (HTN), diabetes mellitus (DM), dyslipidemia (DLP), obstructive sleep apnea (OSA).
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Noppachai Siranart indicated no relevant financial relationships.
Patavee Pajareya indicated no relevant financial relationships.
Peenaprapa Tangpradubkiat indicated no relevant financial relationships.
Runchana Parnicharoende indicated no relevant financial relationships.
Daniel Martin Simadibrata indicated no relevant financial relationships.
Kittithat Tantitanawat indicated no relevant financial relationships.
Panisara Fangsaard, MD1, Noppachai Siranart, MD2, Patavee Pajareya, MD3, Peenaprapa Tangpradubkiat, MD3, Runchana Parnicharoende, MD4, Daniel Martin Simadibrata, MD5, Kittithat Tantitanawat, MD6. P5664 - Improvement of Obesity-Related Comorbidities After Various Bariatric Procedures: A Network Meta-Analysis of Endoscopic versus Surgical Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bassett Medical Center, Cooperstown, NY; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3King Chulalongkorn Memorial Hospital, Bangkok, Krung Thep, Thailand; 4King Chulalongkorn Memorial Hospital, Pathum Wan, Krung Thep, Thailand; 5MetroHealth Medical Center, Cleveland, OH; 6Phramongkutklao Hospital, Bangkok, Krung Thep, Thailand
Introduction: Advances in bariatric care have led to novel endoscopic and surgical techniques to enhance weight loss and reduce obesity-related comorbidities. However, comparative data on their effectiveness remain limited. This study evaluates the impact of different bariatric procedures on comorbidity management and patient outcomes
Methods: We performed a meta-analysis through January 2025, identifying comparative studies of endoscopic and surgical bariatric techniques. Primary endpoints include improvement hypertension (HTN), diabetes mellitus (DM), dyslipidemia (DLP), obstructive sleep apnea (OSA). Secondary endpoints comprised gastroesophageal reflux (GERD) improvement and incidence of de novo reflux.
Results: A total of 56 studies involving 64,520 patients were included in the analysis; RYGB 44 studies, OAGB 20, SASI 1, SADI 2, SG 42, SG+JB 2 ESG 2. For DM improvement, single anastomosis duodeno-ileal bypass with sleeve (SADI) ranked highest (P-score: 0.932), followed by SASI (0.800) and SG with jejunal bypass (SG+JB; 0.587); OAGB doubled odds of remission versus SG (OR: 2.472, 95% CI: 1.49-4.09 vs OR: 1.289, 95% CI: 1.01-1.65). OAGB also topped HTN (0.769) and DLP (0.731). For obstructive sleep apnea (OSA) improvement, OAGB led (0.681), followed by RYGB (0.605). Among surgeries, SG consistently demonstrated the lowest effectiveness across all outcomes. Compared to surgeries, ESG excelled in HTN control, ranking second only to OAGB (P-score 0.694 vs 0.769) but had minimal effects in diabetes remission and DLP improvement (ESG P-score 0.063, well below OAGB, SASI, RYGB and even SG (0.275)). For GERD improvement, single-anastomosis ileal bypass (SASI) ranked highest (P-score: 0.900), followed by one-anastomosis gastric bypass (OAGB; 0.699) and Roux-en-Y gastric bypass (RYGB; 0.563). Both OAGB and RYGB significantly outperformed sleeve gastrectomy (SG) with odds ratios (OR) of 5.48 (95% CI: 1.52-19.76) and 3.82 (95% CI: 2.09–6.98), respectively. SASI showed the lowest incidence of de novo GERD (P-score: 0.803), while endoscopic sleeve gastroplasty (ESG) and RYGB had significantly lower rates than SG (OR: 0.08, 95% CI: 0.01–0.72 and OR: 0.29, 95% CI: 0.18–0.48, respectively).
Discussion: Novel endoscopic (ESG) and surgical (OAGB, SASI, SADI) approaches offer superior relief of obesity-related comorbidities and GERD, with lower rates of de novo reflux than sleeve gastrectomy, and their minimally invasive profiles support their use as first-line treatments.
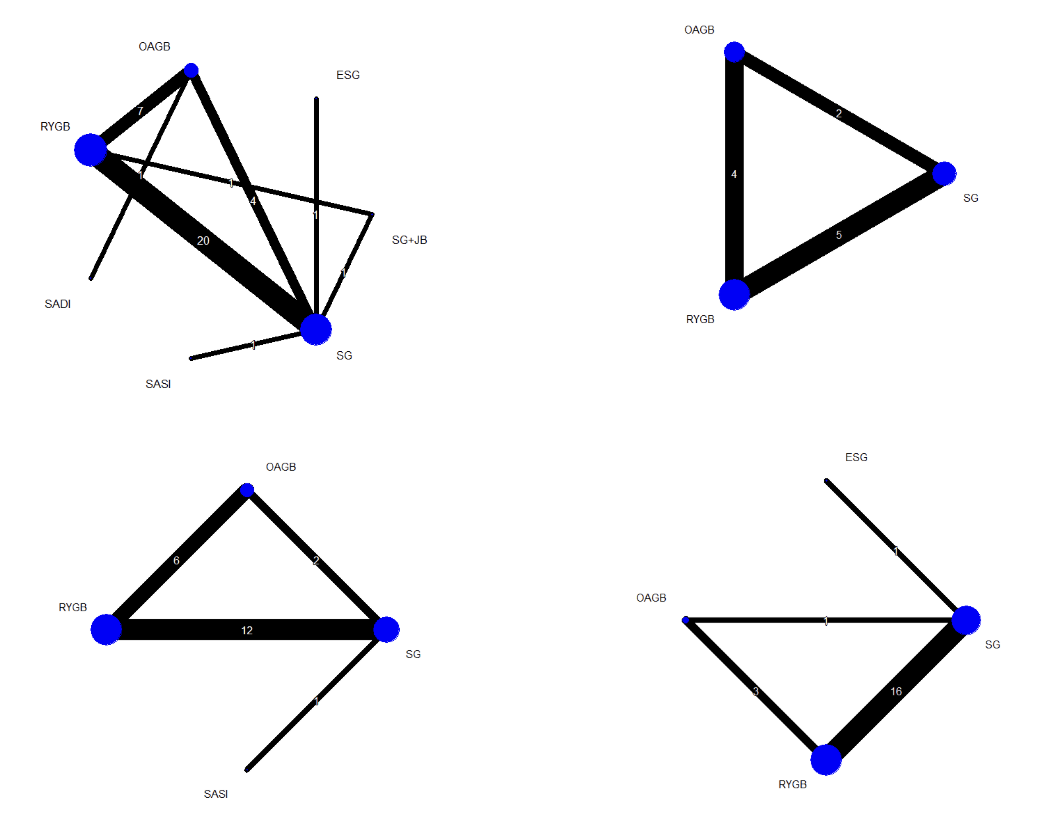
Figure: Figure 1. Primary endpoints include improvement hypertension (HTN), diabetes mellitus (DM), dyslipidemia (DLP), obstructive sleep apnea (OSA).
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Noppachai Siranart indicated no relevant financial relationships.
Patavee Pajareya indicated no relevant financial relationships.
Peenaprapa Tangpradubkiat indicated no relevant financial relationships.
Runchana Parnicharoende indicated no relevant financial relationships.
Daniel Martin Simadibrata indicated no relevant financial relationships.
Kittithat Tantitanawat indicated no relevant financial relationships.
Panisara Fangsaard, MD1, Noppachai Siranart, MD2, Patavee Pajareya, MD3, Peenaprapa Tangpradubkiat, MD3, Runchana Parnicharoende, MD4, Daniel Martin Simadibrata, MD5, Kittithat Tantitanawat, MD6. P5664 - Improvement of Obesity-Related Comorbidities After Various Bariatric Procedures: A Network Meta-Analysis of Endoscopic versus Surgical Interventions, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
