Tuesday Poster Session
Category: Interventional Endoscopy
P5662 - Endoscopic Transpapillary Gallbladder Stenting Is Superior to Percutaneous Transhepatic Gallbladder Drainage in Deferred Acute Cholecystitis: A Propensity-Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Mohammad Abuassi, MD3, Dushyant S. Dahiya, MD4, Ahmad Bazarbashi, MD5
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3University of Central Florida, HCA Healthcare GME, Gainesville, FL; 4University of Kansas School of Medicine, Kansas City, KS; 5Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA
Introduction: Endoscopic transpapillary gallbladder stenting (ETGS) and percutaneous transhepatic gallbladder drainage (PTGBD) are commonly used for biliary decompression in patients with acute cholecystitis who are poor immediate surgical candidates. Despite their widespread use, no large-scale, head-to-head comparisons exist. This study aimed to compare the clinical and surgical outcomes of ETGS versus PTGBD in patients undergoing delayed cholecystectomy, to guide optimal drainage strategy.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify adults (≥18 years) with acute cholecystitis who underwent gallbladder drainage followed by cholecystectomy between 2010 and 2024. Patients were divided into two cohorts: ETGS and PTGBD. Propensity score matching (1:1) was performed based on demographics and comorbidities (Table 1). The primary outcome was 30-day clinical outcomes. Secondary outcomes included post-cholecystectomy surgical complications and conversion to open cholecystectomy. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated; two-sided p-values < 0.05 were considered statistically significant.
Results: Among 5,895 patients who underwent ETGS, the mean age was 61.6 ± 18.2 years; 51.7% were female and 67.2% were White. Compared to PTGBD, ETGS was associated with significantly lower risks of ICU admission (aOR: 0.40; 95% CI: 0.35–0.45), acute kidney injury (aOR: 0.40; 95% CI: 0.35–0.45), shock (aOR: 0.33; 95% CI: 0.24–0.45), and 30-day mortality (aOR: 0.25; 95% CI: 0.20–0.30), all p < 0.001. Hospital readmission rates were similar between groups (P = 0.62). However, ETGS was associated with a higher likelihood of conversion to open cholecystectomy (aOR: 1.27; 95% CI: 1.08–1.50) and increased need for antibiotics and postoperative blood transfusion (Table 2).
Discussion: In this large real-world analysis, ETGS was associated with significantly better short-term clinical outcomes including reduced ICU utilization, organ dysfunction, and mortality compared to PTGBD. Despite a modest increase in surgical complexity at the time of cholecystectomy, these results suggest ETGS may be a safer and more effective first-line drainage strategy in select patients with acute cholecystitis awaiting elective surgery. Incorporating ETGS into routine practice may improve outcomes while balancing operative planning considerations.
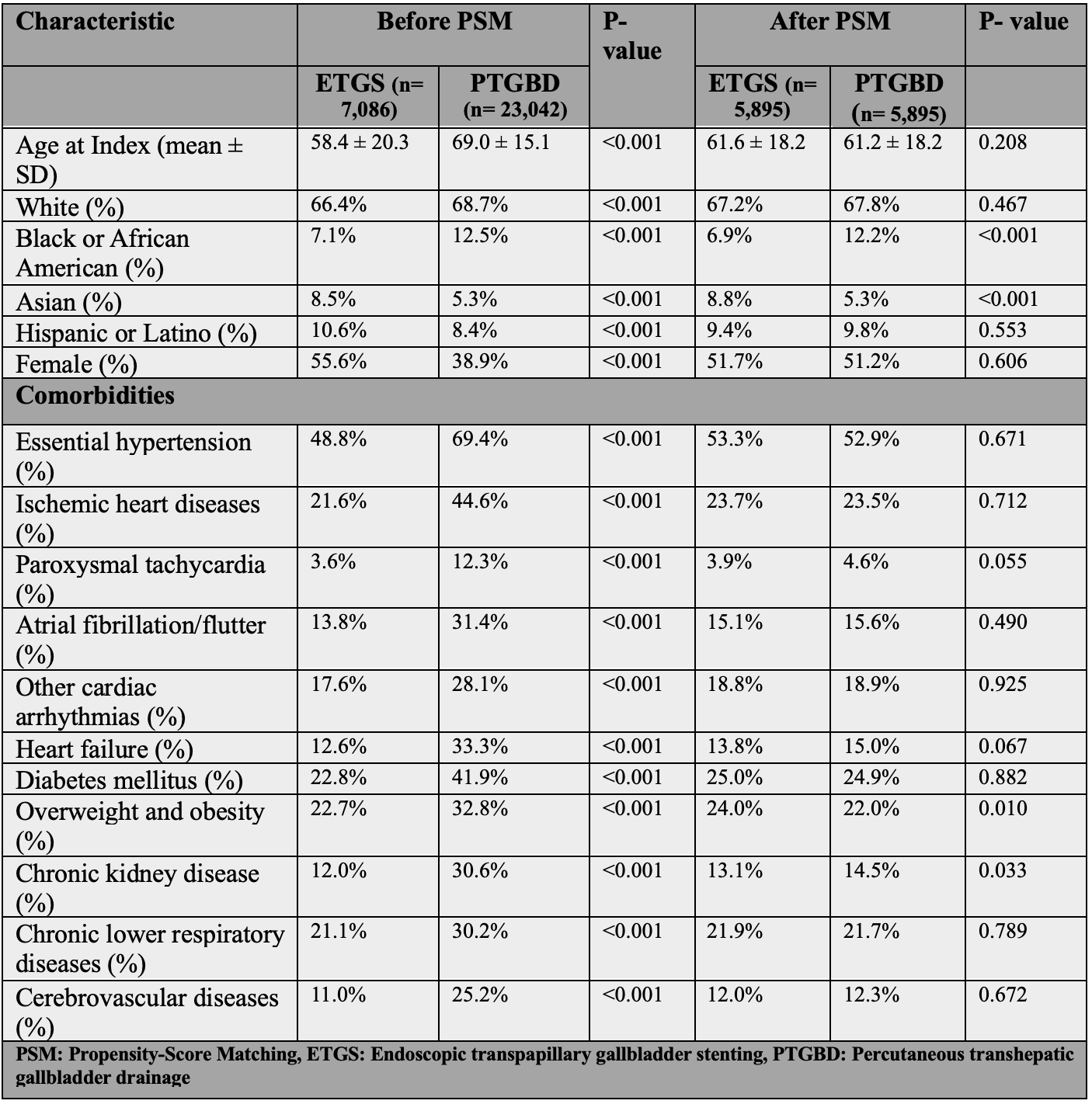
Figure: Table 1: Baseline Characteristics and Comorbidities Before And After Propensity-Score Matching.
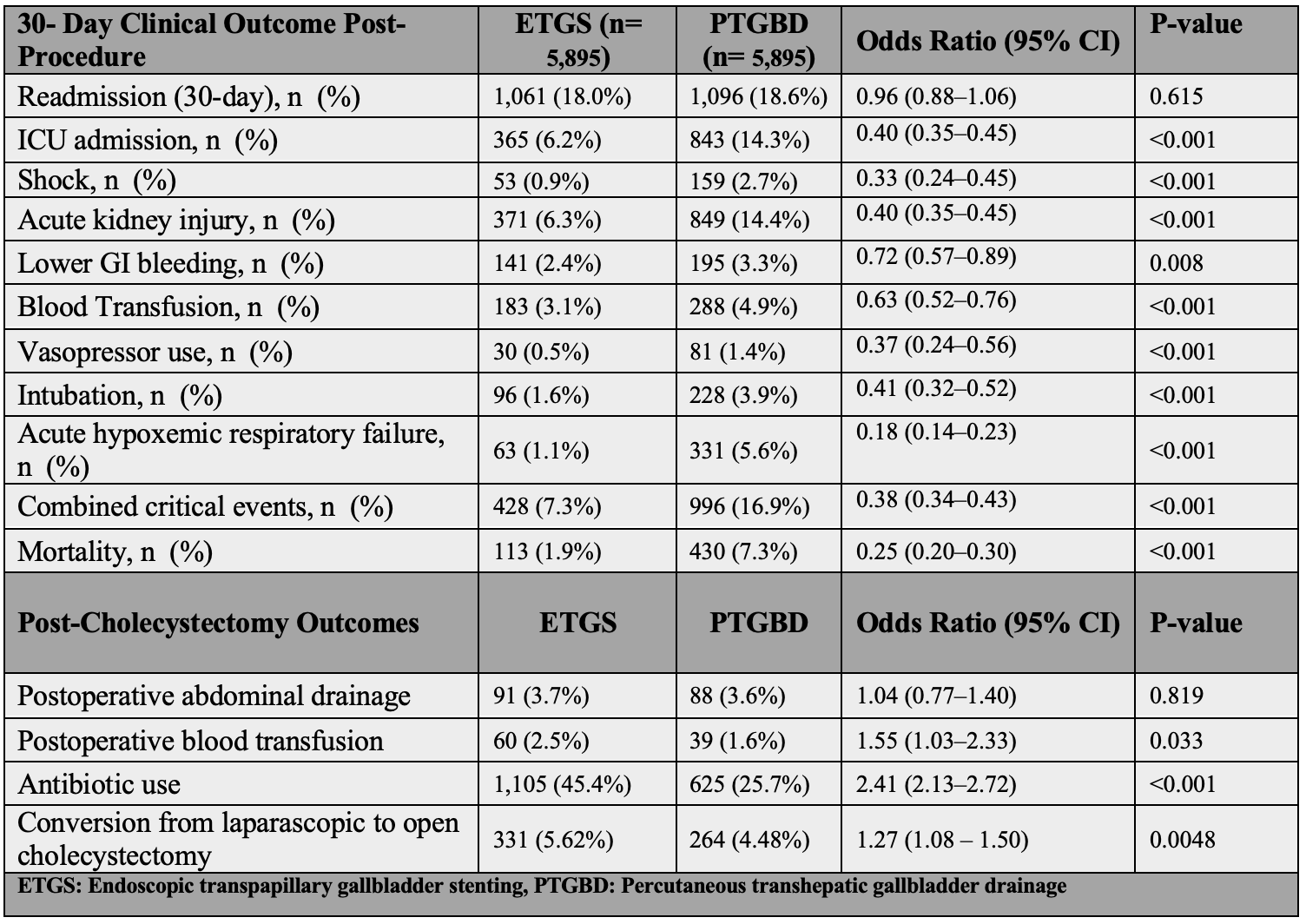
Figure: Table 2: Thirty-Day Clinical Outcomes and Post-Cholecystectomy Outcomes in Patients Undergoing ETGS vs. PTGBD After Propensity Score Matching.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Mohammad Abuassi, MD3, Dushyant S. Dahiya, MD4, Ahmad Bazarbashi, MD5. P5662 - Endoscopic Transpapillary Gallbladder Stenting Is Superior to Percutaneous Transhepatic Gallbladder Drainage in Deferred Acute Cholecystitis: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3University of Central Florida, HCA Healthcare GME, Gainesville, FL; 4University of Kansas School of Medicine, Kansas City, KS; 5Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, WA
Introduction: Endoscopic transpapillary gallbladder stenting (ETGS) and percutaneous transhepatic gallbladder drainage (PTGBD) are commonly used for biliary decompression in patients with acute cholecystitis who are poor immediate surgical candidates. Despite their widespread use, no large-scale, head-to-head comparisons exist. This study aimed to compare the clinical and surgical outcomes of ETGS versus PTGBD in patients undergoing delayed cholecystectomy, to guide optimal drainage strategy.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify adults (≥18 years) with acute cholecystitis who underwent gallbladder drainage followed by cholecystectomy between 2010 and 2024. Patients were divided into two cohorts: ETGS and PTGBD. Propensity score matching (1:1) was performed based on demographics and comorbidities (Table 1). The primary outcome was 30-day clinical outcomes. Secondary outcomes included post-cholecystectomy surgical complications and conversion to open cholecystectomy. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated; two-sided p-values < 0.05 were considered statistically significant.
Results: Among 5,895 patients who underwent ETGS, the mean age was 61.6 ± 18.2 years; 51.7% were female and 67.2% were White. Compared to PTGBD, ETGS was associated with significantly lower risks of ICU admission (aOR: 0.40; 95% CI: 0.35–0.45), acute kidney injury (aOR: 0.40; 95% CI: 0.35–0.45), shock (aOR: 0.33; 95% CI: 0.24–0.45), and 30-day mortality (aOR: 0.25; 95% CI: 0.20–0.30), all p < 0.001. Hospital readmission rates were similar between groups (P = 0.62). However, ETGS was associated with a higher likelihood of conversion to open cholecystectomy (aOR: 1.27; 95% CI: 1.08–1.50) and increased need for antibiotics and postoperative blood transfusion (Table 2).
Discussion: In this large real-world analysis, ETGS was associated with significantly better short-term clinical outcomes including reduced ICU utilization, organ dysfunction, and mortality compared to PTGBD. Despite a modest increase in surgical complexity at the time of cholecystectomy, these results suggest ETGS may be a safer and more effective first-line drainage strategy in select patients with acute cholecystitis awaiting elective surgery. Incorporating ETGS into routine practice may improve outcomes while balancing operative planning considerations.
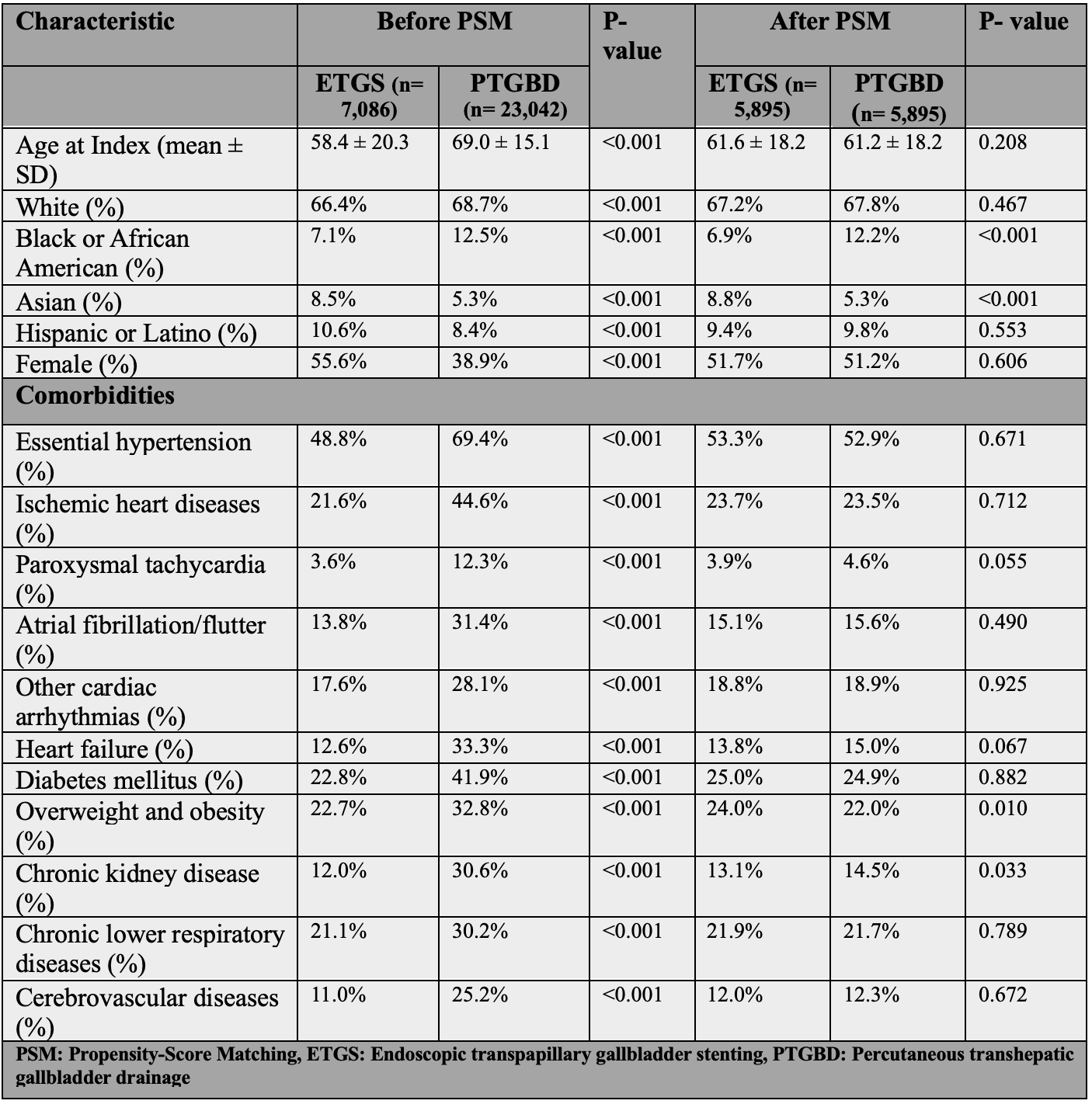
Figure: Table 1: Baseline Characteristics and Comorbidities Before And After Propensity-Score Matching.
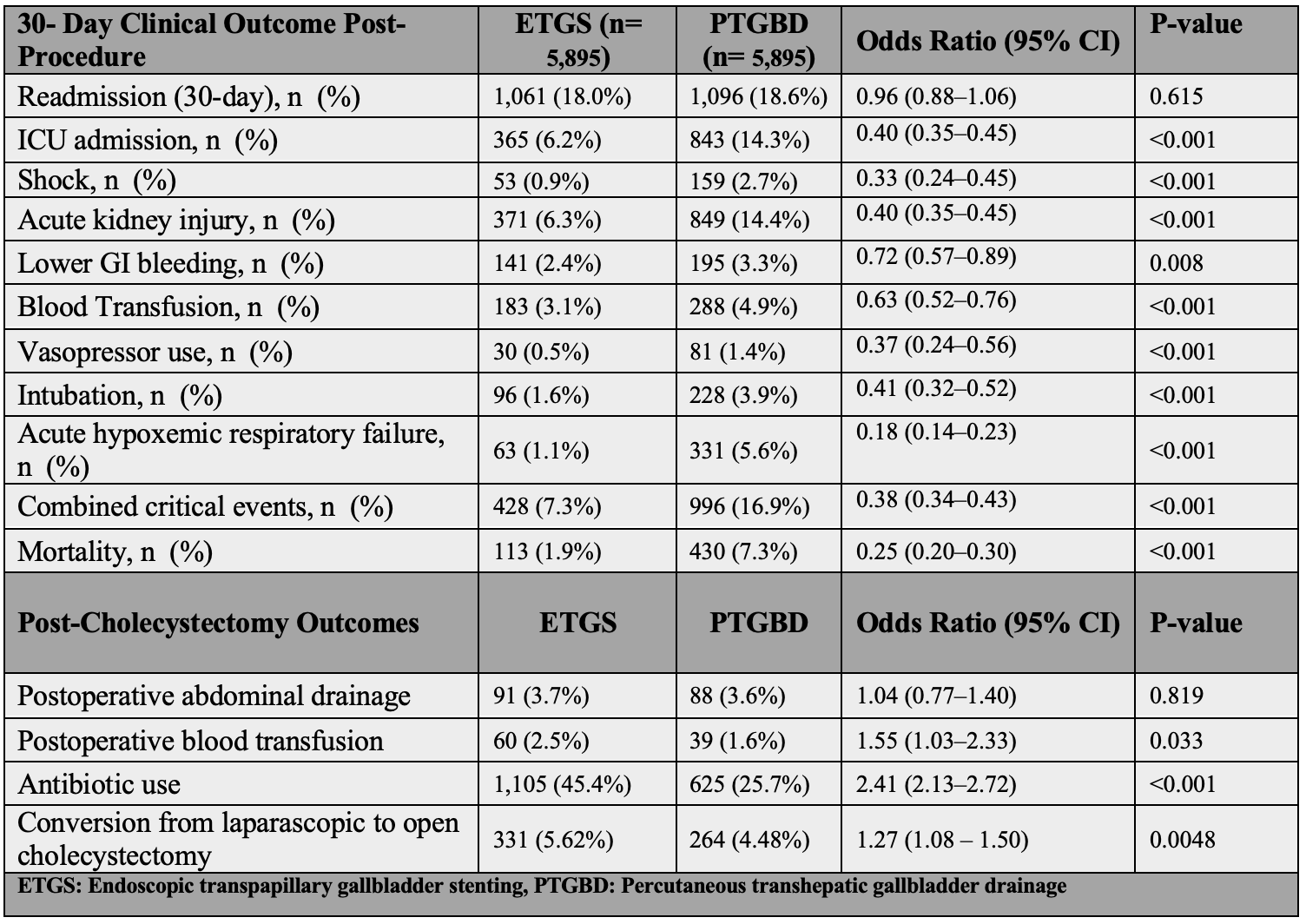
Figure: Table 2: Thirty-Day Clinical Outcomes and Post-Cholecystectomy Outcomes in Patients Undergoing ETGS vs. PTGBD After Propensity Score Matching.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Ahmad Bazarbashi indicated no relevant financial relationships.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Mohammad Abuassi, MD3, Dushyant S. Dahiya, MD4, Ahmad Bazarbashi, MD5. P5662 - Endoscopic Transpapillary Gallbladder Stenting Is Superior to Percutaneous Transhepatic Gallbladder Drainage in Deferred Acute Cholecystitis: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
