Tuesday Poster Session
Category: Interventional Endoscopy
P5750 - Pneumoperitoneum Post Endoscopic Necrosectomy: Management of a Dreaded Complication
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmed Shehadah, MD (he/him/his)
United Health Services, Wilson Medical Center
Binghamton, NY
Presenting Author(s)
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Hammad Qadri, MD3, Khandokar Talib, MD4, Muhammad Ahmed, MD3, AbdulSubhan Talpur, MD1, Toseef Javaid, MD3
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY
Introduction: The management of walled-off pancreatic necrosis (WOPN) presents unique challenges. Morbidity and mortality of open surgical approach is high and there is a shift towards a minimally invasive endoscopic approach. Hereby, we present a case highlighting a complex management of a WOPN, involving multiple interventions over a year.
Case Description/
Methods: A 30-year-old male with a history of alcohol use disorder presented with severe abdominal pain and tachycardia, otherwise hemodynamically stable. Labs revealed an elevated lipase level of 390, and a CT scan showed a large WOPN measuring 37 x 26 cm. Antibiotics were started for the infected necrotizing pancreatitis.
The patient underwent endoscopic ultrasound guided cystogastrostomy (EUS-CG) with the placement of a 15 x 10 mm lumen-apposing metal stent (LAMS), followed by multiple direct endoscopic necrosectomy (DEN) sessions using a snare. ERCP showed incomplete pancreatic divisum with duct disruption in mid pancreatic body leading to ductal hypertension in the pancreatic tail for which he underwent pancreatic stent placement. Chemical necrosectomy using diluted hydrogen peroxide was frequently employed during DEN to manage persistent necrosis.
The patient developed severe abdominal pain after the final necrosectomy session and was found to have pneumoperitoneum on X-ray. An urgent CT scan with oral and IV contrast confirmed the stable position of the LAMS and revealed abdominal free air without evidence of viscus perforation. Pneumoperitoneum due to pseudocyst wall perforation was suspected. LAMS was removed due to concerns about potential peritoneal contamination and the site was closed using endoclips. A nasogastric tube was placed, antibiotics were initiated, and the patient improved without complications one week later.
Discussion: There is a paucity of literature on the management of post-procedural complications associated with DEN. Our case highlights a rare but serious complication of DEN in patients with WOPN. The complication was successfully managed with conservative measures, avoiding the need for surgical intervention or interventional radiological approaches. The exact etiology of the pneumoperitoneum remains unclear. It may have resulted from chemical or mechanical necrosectomy causing a rupture of the cyst’s free wall, despite the LAMS being well-positioned on imaging. This emphasizes the need for further studies to better understand the underlying mechanisms and to develop management strategies for such challenging scenarios.
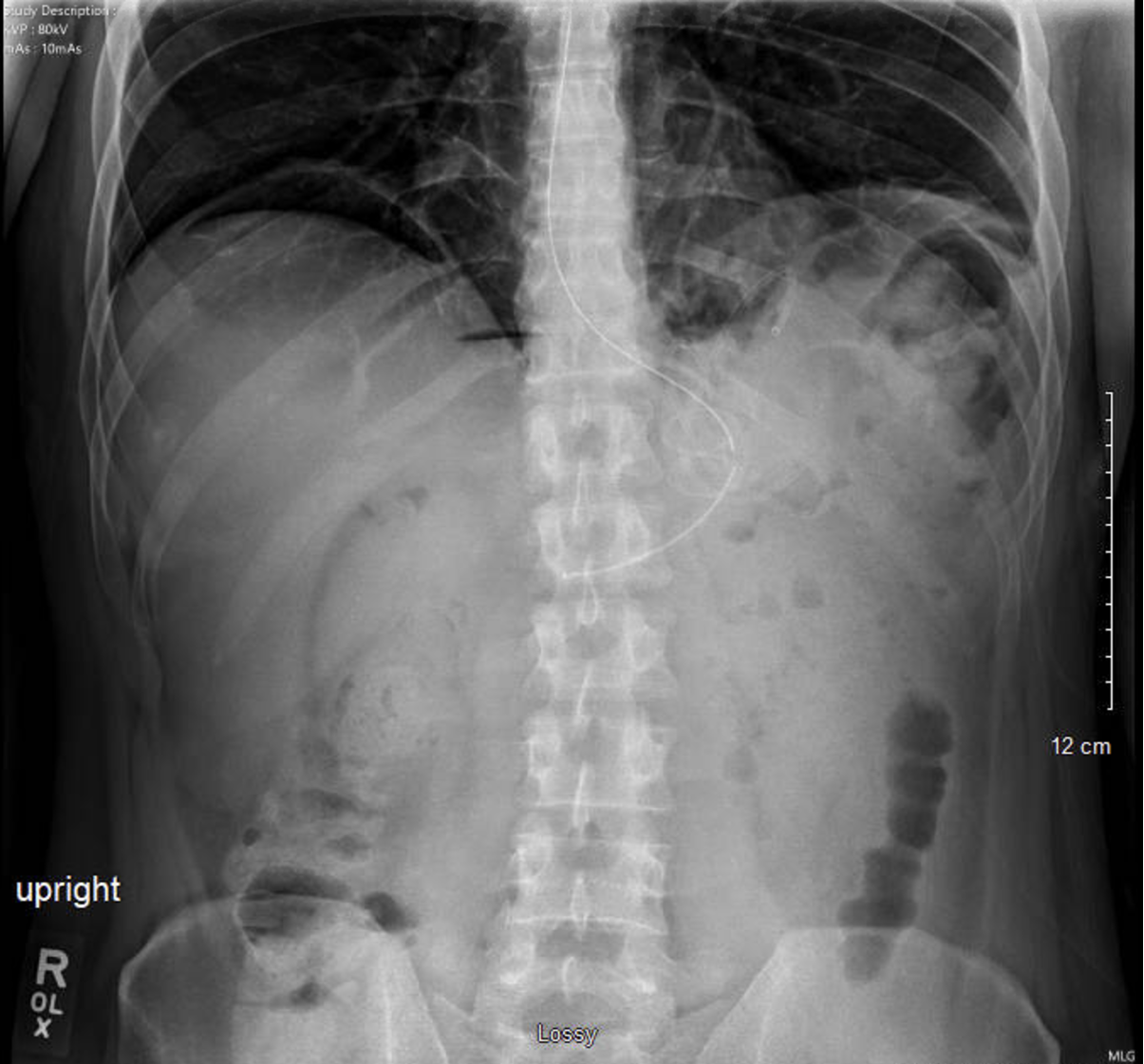
Figure: Image showing pneumoperitoneum on abdominal X-ray post-endoscopic necrosectomy.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Hammad Qadri, MD3, Khandokar Talib, MD4, Muhammad Ahmed, MD3, AbdulSubhan Talpur, MD1, Toseef Javaid, MD3. P5750 - Pneumoperitoneum Post Endoscopic Necrosectomy: Management of a Dreaded Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1United Health Services, Wilson Medical Center, Binghamton, NY; 2Rochester General Hospital, Rochester, NY; 3United Health Services, Wilson Medical Center, Johnson City, NY; 4United Health Services, Johnson City, NY
Introduction: The management of walled-off pancreatic necrosis (WOPN) presents unique challenges. Morbidity and mortality of open surgical approach is high and there is a shift towards a minimally invasive endoscopic approach. Hereby, we present a case highlighting a complex management of a WOPN, involving multiple interventions over a year.
Case Description/
Methods: A 30-year-old male with a history of alcohol use disorder presented with severe abdominal pain and tachycardia, otherwise hemodynamically stable. Labs revealed an elevated lipase level of 390, and a CT scan showed a large WOPN measuring 37 x 26 cm. Antibiotics were started for the infected necrotizing pancreatitis.
The patient underwent endoscopic ultrasound guided cystogastrostomy (EUS-CG) with the placement of a 15 x 10 mm lumen-apposing metal stent (LAMS), followed by multiple direct endoscopic necrosectomy (DEN) sessions using a snare. ERCP showed incomplete pancreatic divisum with duct disruption in mid pancreatic body leading to ductal hypertension in the pancreatic tail for which he underwent pancreatic stent placement. Chemical necrosectomy using diluted hydrogen peroxide was frequently employed during DEN to manage persistent necrosis.
The patient developed severe abdominal pain after the final necrosectomy session and was found to have pneumoperitoneum on X-ray. An urgent CT scan with oral and IV contrast confirmed the stable position of the LAMS and revealed abdominal free air without evidence of viscus perforation. Pneumoperitoneum due to pseudocyst wall perforation was suspected. LAMS was removed due to concerns about potential peritoneal contamination and the site was closed using endoclips. A nasogastric tube was placed, antibiotics were initiated, and the patient improved without complications one week later.
Discussion: There is a paucity of literature on the management of post-procedural complications associated with DEN. Our case highlights a rare but serious complication of DEN in patients with WOPN. The complication was successfully managed with conservative measures, avoiding the need for surgical intervention or interventional radiological approaches. The exact etiology of the pneumoperitoneum remains unclear. It may have resulted from chemical or mechanical necrosectomy causing a rupture of the cyst’s free wall, despite the LAMS being well-positioned on imaging. This emphasizes the need for further studies to better understand the underlying mechanisms and to develop management strategies for such challenging scenarios.
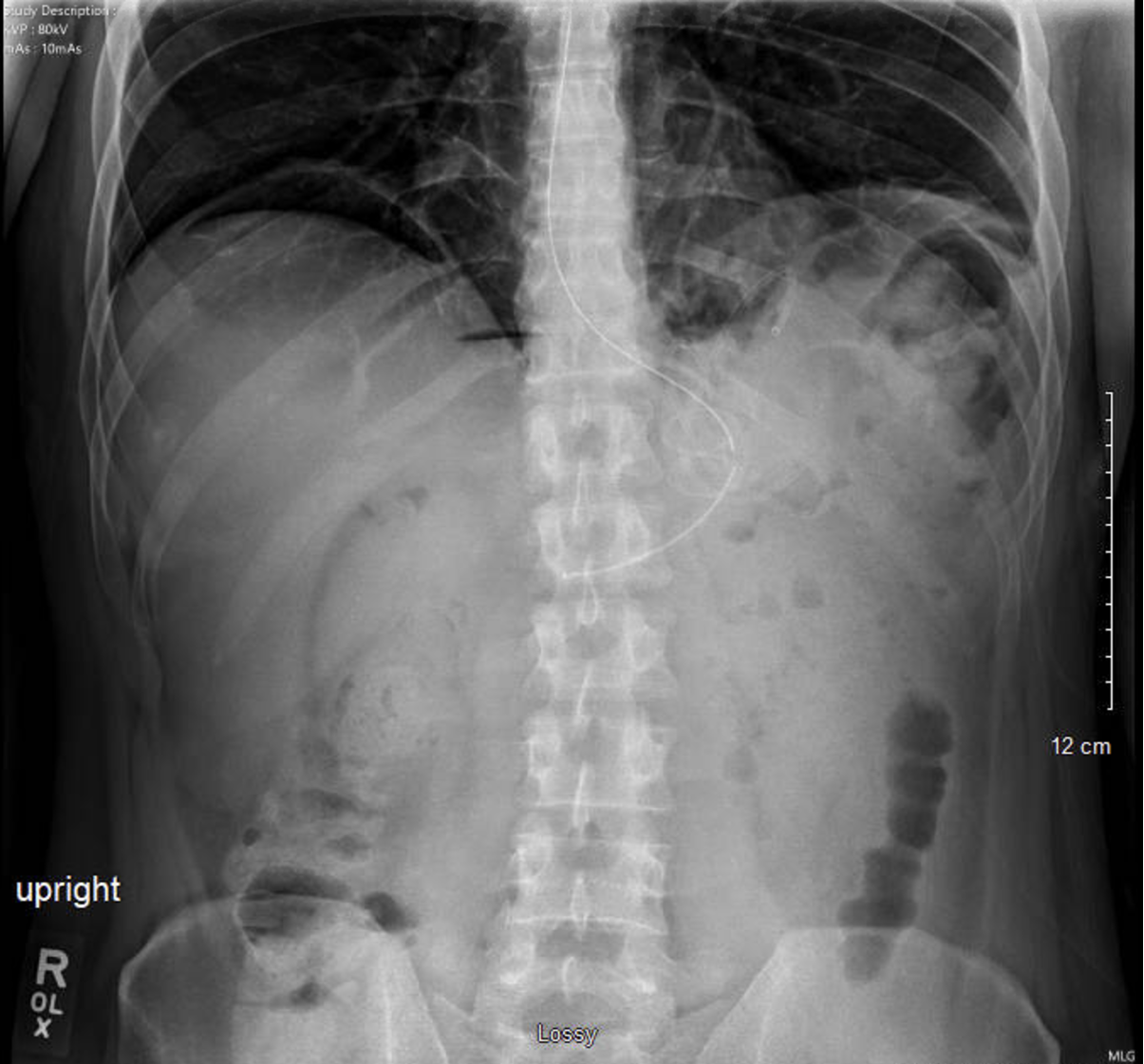
Figure: Image showing pneumoperitoneum on abdominal X-ray post-endoscopic necrosectomy.
Disclosures:
Ahmed Shehadah indicated no relevant financial relationships.
Alshaima Yousef indicated no relevant financial relationships.
Usama Sakhawat indicated no relevant financial relationships.
Sadia Tabassum indicated no relevant financial relationships.
Ibrar Atiq indicated no relevant financial relationships.
Hammad Qadri indicated no relevant financial relationships.
Khandokar Talib indicated no relevant financial relationships.
Muhammad Ahmed indicated no relevant financial relationships.
AbdulSubhan Talpur indicated no relevant financial relationships.
Toseef Javaid indicated no relevant financial relationships.
Ahmed Shehadah, MD1, Alshaima Yousef, MD2, Usama Sakhawat, MD3, Sadia Tabassum, MD1, Ibrar Atiq, MD3, Hammad Qadri, MD3, Khandokar Talib, MD4, Muhammad Ahmed, MD3, AbdulSubhan Talpur, MD1, Toseef Javaid, MD3. P5750 - Pneumoperitoneum Post Endoscopic Necrosectomy: Management of a Dreaded Complication, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
