Tuesday Poster Session
Category: Interventional Endoscopy
P5737 - Endoscopic Vacuum Therapy for Boerhaave Syndrome and Recurrent Esophageal Perforation: A Minimally Invasive Approach
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Heather N. Gosnell, DO (she/her/hers)
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Heather N. Gosnell, DO1, Michael Daniel, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Tampa General Hospital / University of South Florida, Tampa, FL
Introduction: Endoscopic vacuum therapy (EVT) is increasingly recognized as an effective, minimally invasive therapy for esophageal perforation (EP). We present a complex case of Boerhaave Syndrome (BS) complicated by recurrent EP, ultimately managed successfully with EVT.
Case Description/
Methods: A 63-year-old male with a history of alcohol use disorder presented to the hospital in clinical shock following a three-day history of forceful hematemesis. Initial evaluation revealed severe duodenitis, marked gastric and esophageal distension, and extraluminal gas concerning for gastric outlet obstruction and BS. The patient was taken emergently to the operating room for thoracotomy, exploratory laparotomy, and primary esophageal repair.
His complicated hospital course was prolonged by recurrent esophageal leak, bilateral pleural effusions, and development of a chest abscess, requiring esophageal stent placement and video-assisted thoracoscopic surgery. Following stent removal (Figure 1A-1B), he developed increased green-brown output from the chest tube, and imaging suggested recurrent EP (Figure 1C). EGD with EVT for seven days resulted in successful healing of the defect. Three weeks later, the patient developed acute anemia and melena. Repeat EGD revealed LA Grade D esophagitis and a cratered esophageal ulcer with active bleeding, which was managed with epinephrine injection, bipolar cautery, and Purastat. Despite four weeks of high-dose PPI therapy, he experienced recurrent anemia and melena. Follow-up endoscopy showed severe diffuse esophagitis with contact oozing, and sucralfate was added to promote mucosal healing. He was ultimately discharged to a rehabilitation facility nearly four months after initial presentation.
Upon evaluation in gastroenterology clinic, the patient reported daily episodes of emesis and an esophageal stricture. Repeat EGD revealed a single, benign-appearing intrinsic stenosis measuring approximately 5 mm by 12 cm (Figure 1D); the stricture was successfully dilated using a TTS dilator. He required monthly dilations to maintain esophageal patency, adequate nutrition, and quality of life.
Discussion: This case highlights the complex management of recurrent EP following unsuccessful surgical repair and stenting. Emerging evidence suggests that EVT may offer improved clinical success and potential survival benefits compared to traditional modalities such as stenting. However, further randomized trials are needed to more clearly define its comparative efficacy and safety.
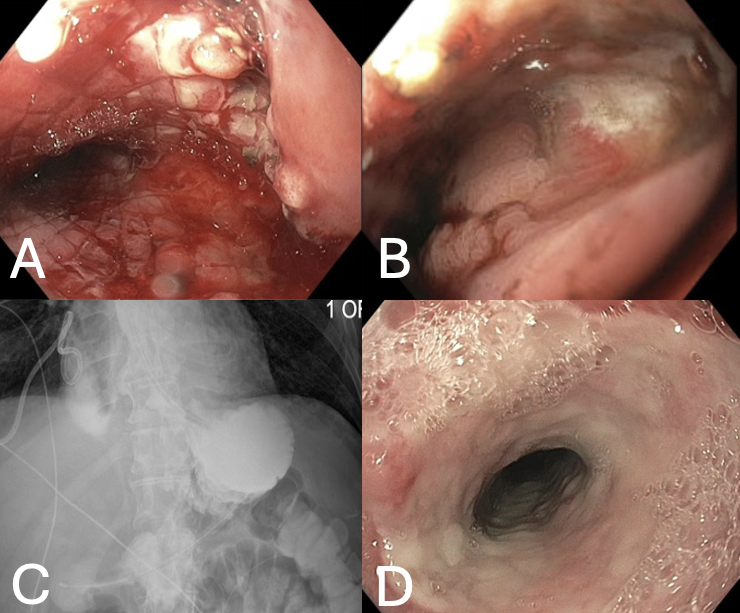
Figure: Figure 1: A) Distal third esophagus just after stent removal. B) Distal third esophagus demonstrating healed prior perforation site. C) Upper GI Series with Small Bowel Follow Through demonstrating gastrografin contrast accumulation in right lung base consistent with recurrent EP. D) Benign-appearing, intrinsic severe stenosis approximately 25cm from the incisors.
Disclosures:
Heather Gosnell indicated no relevant financial relationships.
Michael Daniel indicated no relevant financial relationships.
Heather N. Gosnell, DO1, Michael Daniel, MD2. P5737 - Endoscopic Vacuum Therapy for Boerhaave Syndrome and Recurrent Esophageal Perforation: A Minimally Invasive Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Tampa General Hospital / University of South Florida, Tampa, FL
Introduction: Endoscopic vacuum therapy (EVT) is increasingly recognized as an effective, minimally invasive therapy for esophageal perforation (EP). We present a complex case of Boerhaave Syndrome (BS) complicated by recurrent EP, ultimately managed successfully with EVT.
Case Description/
Methods: A 63-year-old male with a history of alcohol use disorder presented to the hospital in clinical shock following a three-day history of forceful hematemesis. Initial evaluation revealed severe duodenitis, marked gastric and esophageal distension, and extraluminal gas concerning for gastric outlet obstruction and BS. The patient was taken emergently to the operating room for thoracotomy, exploratory laparotomy, and primary esophageal repair.
His complicated hospital course was prolonged by recurrent esophageal leak, bilateral pleural effusions, and development of a chest abscess, requiring esophageal stent placement and video-assisted thoracoscopic surgery. Following stent removal (Figure 1A-1B), he developed increased green-brown output from the chest tube, and imaging suggested recurrent EP (Figure 1C). EGD with EVT for seven days resulted in successful healing of the defect. Three weeks later, the patient developed acute anemia and melena. Repeat EGD revealed LA Grade D esophagitis and a cratered esophageal ulcer with active bleeding, which was managed with epinephrine injection, bipolar cautery, and Purastat. Despite four weeks of high-dose PPI therapy, he experienced recurrent anemia and melena. Follow-up endoscopy showed severe diffuse esophagitis with contact oozing, and sucralfate was added to promote mucosal healing. He was ultimately discharged to a rehabilitation facility nearly four months after initial presentation.
Upon evaluation in gastroenterology clinic, the patient reported daily episodes of emesis and an esophageal stricture. Repeat EGD revealed a single, benign-appearing intrinsic stenosis measuring approximately 5 mm by 12 cm (Figure 1D); the stricture was successfully dilated using a TTS dilator. He required monthly dilations to maintain esophageal patency, adequate nutrition, and quality of life.
Discussion: This case highlights the complex management of recurrent EP following unsuccessful surgical repair and stenting. Emerging evidence suggests that EVT may offer improved clinical success and potential survival benefits compared to traditional modalities such as stenting. However, further randomized trials are needed to more clearly define its comparative efficacy and safety.
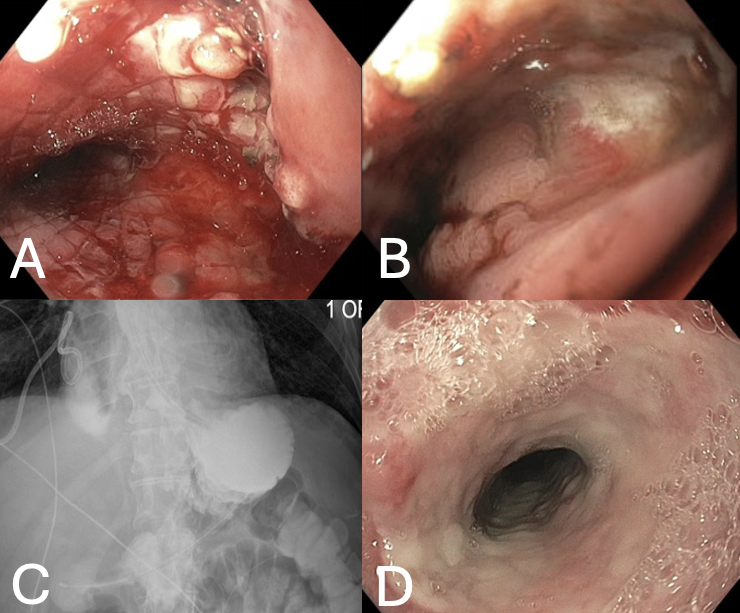
Figure: Figure 1: A) Distal third esophagus just after stent removal. B) Distal third esophagus demonstrating healed prior perforation site. C) Upper GI Series with Small Bowel Follow Through demonstrating gastrografin contrast accumulation in right lung base consistent with recurrent EP. D) Benign-appearing, intrinsic severe stenosis approximately 25cm from the incisors.
Disclosures:
Heather Gosnell indicated no relevant financial relationships.
Michael Daniel indicated no relevant financial relationships.
Heather N. Gosnell, DO1, Michael Daniel, MD2. P5737 - Endoscopic Vacuum Therapy for Boerhaave Syndrome and Recurrent Esophageal Perforation: A Minimally Invasive Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
